Abstract
Care of mechanically ventilated patients requires coordination between multiple caregivers, necessitating the availability of accurate and timely information on patient status. Researchers have documented positive effects of several interventions on the rates of developing ventilator associated complications, such as providing regular oral care and elevating the head of the bed. Informatics tools, such as electronic whiteboards, reminders, and alerts have been shown to aid in clinician compliance with guidelines or protocols. The purpose of this project was to design and implement a real-time ventilator management dashboard to show patient status with respect to elements important for ventilator management and infection prevention in the adult Intensive Care Units at Vanderbilt University Medical Center.
Introduction
Complications associated with being on a mechanical ventilator account for significant morbidity and mortality in Intensive Care Unit (ICU) populations1. Many Quality-focused organizations, such as the Institute for Healthcare Improvement and the Centers for Disease Control and Prevention (CDC), have focused on strategies to reduce the occurrence of complications such as ventilator associated pneumonia, as well as to minimize the time a patient spends on a ventilator2–3. Researchers have documented positive effects of several interventions on the rates of developing ventilator associated complications, such as regular oral care, and elevating the head of the bed4–6. Informatics tools, such as electronic whiteboards, reminders, and alerts have been shown to aid in clinician compliance with guidelines or protocols7–8. Care of mechanically ventilated patients requires coordination between multiple caregivers, necessitating the availability of accurate and timely information on patient status. The purpose of this project was to design and implement a real-time ventilator management dashboard to show patient status with respect to elements important for ventilator management and infection prevention in the adult Intensive Care Units at Vanderbilt University Medical Center.
The Ventilator Management Bundle
In the winter of 2007 Vanderbilt Medical Center held a retreat that included leaders from Quality, Hospital Administration, Respiratory Therapy, Nursing, Informatics, and the Medical Directors from each of the intensive care units. At the retreat, evidence and published guidelines were reviewed and discussed, and agreement was reached to implement a standard ventilator management protocol across all adult ICUs9–10. A leadership team that included representatives from each discipline present at the retreat was formed to oversee the details of implementing the standardized protocol, with the goal to hardwire the protocol into clinical workflow and achieve a high level of compliance. Because coordination of multiple tasks and caregivers is required for effective ventilator management, Information Technology (IT) solutions were targeted as a key component in monitoring and delivering necessary care components. This included discipline-specific documentation tools, standardized order sets, and an electronic dashboard to display real-time patient status with respect to protocol elements. Specific protocol elements were derived from existing ventilator management “bundle” recommendations from the Institute for Healthcare Improvement, Guidelines.gov, the CDC, and other evidence sources2–5. Table 1 describes Vanderbilt’s agreed-upon set of protocol elements.
Table 1.
Vanderbilt’s Ventilator Management Bundle
| Protocol Element | Roles Involved | Process Step |
|---|---|---|
| DVT Prophylaxis | Physician + Nurse | MD generates order, RN implements |
| Stress Ulcer Prophylaxis | Physician + Nurse | MD generates order, RN implements |
| Sedation management and daily assessment of readiness to extubate | Physician + Nurse + Respiratory Therapist | Daily monitoring and respiratory screening, with spontaneous breathing trials where appropriate |
| Elevate head of bed 35-45 degrees | Physician + Nurse | MD generates order, RN implements |
| Oral Swabs | Nurse + Care Partner | RN / Care Partner implements |
| Teeth Brushing | Nurse + Care Partner | RN / Care Partner implements |
| Hypopharyngeal Suctioning | Nurse + Respiratory Therapist + Care Partner | RN / RT / Care Partner implements |
The Ventilator Management Dashboard
In order to aid in “hardwiring” the ventilator management bundle into clinical practice, two goals were set. The first was to provide up-to-the-minute status for each ventilated patient, to aid in real-time course correction. The second goal was to continuously monitor ongoing status with respect to the bundle, to aid in identification of bottlenecks and system barriers to compliance through daily, weekly and monthly status reports and drill downs. The implementation of the ventilator management bundle, as shown in Table 1, includes DVT and stress ulcer prophylaxis, head-of-bed elevation, sedation management with daily assessments of readiness to extubate, and oral care. Each element of the bundle requires the coordination of multiple roles (Nurse, Physician, Respiratory Therapist, Care Partner), and requires action and documentation of the action taken. It was decided that clinical staff would be best served by an implementation that required no additional work beyond what is ordinarily carried out. Thus, the dashboard was created to indicate the status of each bundle element based on items already routinely charted or ordered within each discipline’s documentation tool and the hospital’s order entry system. Each bundle element has associated business rules that are driven by clinician workflow associated with performing and documenting the required action(s). Because a team is involved in ventilator management, coordination of tasks and communication across provider roles is critical to ensure appropriate patient care. In order to facilitate open communication of a patient’s bundle status, it was decided to develop a ventilator management dashboard for display on a computer screensaver application on all workstations within each of the six adult intensive care units at Vanderbilt University Hospital. The dashboard is additionally available for display on-demand within the hospital’s electronic medical record (EMR).
In addition to display of real-time patient status with respect to bundle elements, the dashboard was designed to aid in supporting existing, or desired, clinician work flow. For each element of the bundle, an indicator is displayed showing status with regard to the process step. The simple color scheme of red, yellow, and green was chosen to represent various states of compliance with the process steps. Red indicates “out of compliance”, yellow indicates “in compliance but the item is coming due”, and green indicates compliance. For example, a patient must have teeth brushed every 12 hours by protocol. At 8 hours the dashboard item turns yellow indicating the task is due soon. A grace period is built in to each item to allow for patient variability (patient off the floor for a CT scan, etc); in the case of teeth brushing the indicator does not turn red until 16 hours after the last documentation event. In addition to allowing for patient variability, the dashboard is also designed to support clinician workflow such as shift changes, physician rounding patterns, and unit staffing patterns. For example, spontaneous breathing trial screening and trials are set to be initiated by the night shift, and completed by the day shift within an agreed-upon time window. The target sedation score is also designed to promote a rhythm of setting the target for each day on morning rounds. Table 2 contains a list of the current high-level business rules for each element of the bundle.
Table 2.
High Level Business Rules
| Protocol Element | Dashboard Indicator | Source† | Interval | Green | Yellow | Red |
|---|---|---|---|---|---|---|
| DVT Prophylaxis | DVT Prophylaxis | Order Entry | On admission | Done | n/a | Not done |
| Stress Ulcer Prophylaxis | Stress Ulcer Prophylaxis | Order Entry | On admission | Done | n/a | Not done |
| Sedation management and daily assessment of readiness to extubate | Spontaneous Breathing Trial (SBT) Screening | Respiratory Therapy System | Every 24 hours | Done P=Pass F=Fail | >18 hours | Not done |
| SBT Trial | Respiratory Therapy System | Within 6 hours of a successful screen | Done P=Pass F=Fail | <6 hours from successful screen | >6 hours from successful screen | |
| Target Sedation Score (RASS) | Order Entry | Every 24 hours | Done | 5am – 12pm | Not done | |
| Actual RASS | Documentation | Every 2 hours | Done | >1.5 hours | >3.5 hours | |
| HOB elevation | HOB elevation | Documentation | Every 2 hours | Done | >1.5 hours | >3.5 hours |
| Oral Care | Oral Swabs | Documentation | Every 2 hours | Done | >1.5 hours | >3.5 hours |
| Hypopharyngeal Suctioning | Documentation | Every 4 hours | Done | >3.5 hours | >5.5 hours | |
| Teeth Brushing | Documentation | Every 12 hours | Done | >8 hours | >16 hours |
Source system abbreviations used above are as follows: Order Entry: Data captured from the CPOE system. Documentation: Data captured from the Nurse charting system. Respiratory Therapy System: Data captured from the Respiratory Therapy documentation system
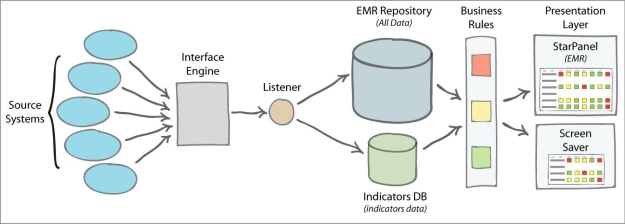
System Architecture
The dashboard utilizes data from various source systems already in use by clinical personnel, including clinical documentation systems and computerized provider order entry (CPOE). These systems pass results through an interface engine which in turn routes the results to subscriber systems. One such subscriber system is the electronic medical record which houses all text-related clinical data. A listener on the front end of the EMR siphons off data points relevant to the ventilator bundle to a database specifically designed to house dashboard indicator data. A business rules layer applies rules to the data to decide which color and status to display on the clinical dashboard. The EMR allows aggregation of patients into panels, which include defined clinical units such as the medical ICU, as well as other aggregations such as all current inpatients on a ventilator. The dashboard display is driven off of a defined panel of patients, and displays current status as of the last refresh. This display is available both within the EMR, and also as a screen saver on each workstation in all ICUs. The screen saver is pre-configured to display the status for each patient within a particular ICU.
Reporting
Reports are a critical piece of the system, allowing clinicians and managers to identify and address people, process, and technology barriers to successful compliance. Snapshots of the dashboard indicators are exported to the Vanderbilt Enterprise Data Warehouse every 5 minutes and made available for reports. Reports provide the status of bundle elements over time and can be viewed for a single ICU or across ICUs. Daily reports show hourly compliance status to aid in determining potential workflow or system barriers to compliance, such as issues at shift change, or nighttime staffing. The reports also allow detailed assessments of areas on which a unit can focus to improve overall compliance.
Preliminary Results
Overall the system has been well received. The bundle was implemented in the spring of 2007, and the dashboard was initially rolled out on a pilot unit starting in the summer of 2007. By September of 2007 the screen saver was active in all adult ICUs.
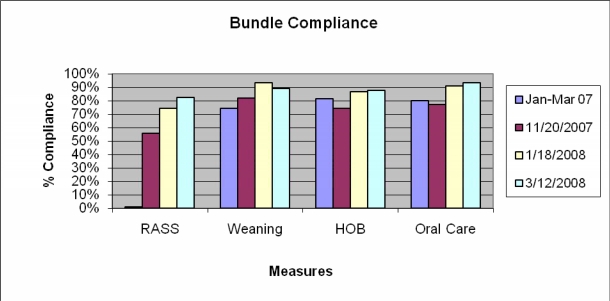
Compliance has improved over time as shown in Figure 2, and workflow and system barriers are still being addressed to further improve compliance. In addition to aiding with bundle execution and identification of barriers to compliance, there have been several other added benefits of the system. Nurse Managers and Charge Nurses have noted that dashboard status allows them to more quickly see when a nurse is becoming overloaded with a patient, and can divert resources to help early without having to be called by the busy nurse. The system has also led to reports of more frequent collaboration among members of the healthcare team. Studies are underway to assess any positive impact on time to extubation, reintubation rate, and other accepted measures of ventilator management.
Figure 2.
Bundle Compliance Jan-Mar 2007 data by manual audits (n=1001). No RASS data for Jan-Mar 2007. All other data are post intervention and are sampled every 5 minutes (daily average n=30101).
Discussion
The system has overall been received as a help, but challenges remain. Because indicator status is driven off of timely documentation, indicators are not always up to date with what a provider has actually performed. Some units utilize a batch charting process for some items, which can lead to higher levels of non-compliance noted on dashboard reports. This mainly involved charting of hypopharyngeal suctioning in some of the units, and subsequent analysis of the results show this to have a small actual impact on the overall measures. The issue still remains, however, that the tool does not necessarily adequately support a batch charting workflow.
Other challenges stem from organizational buy-in and accountability in an environment where medical residents frequently rotate on and off a unit. This has highlighted the need for team accountability with ownership by individual roles, and accountability structures within each particular role (Physicians, Nurses, Respiratory Therapists). Changes to the charter and function of Vanderbilt’s Institutional Critical Care Committee are being enacted to better highlight the importance and accountability for each ICU director for the ventilator management bundle.
A final challenge is appropriate integration with charting tools and CPOE. The dashboard is easily available, but when someone enters a particular source system for documentation tasks, the dashboard may no longer be visible. This leads to some workflow inefficiencies when trying to assess the current status while in the nurse charting application, for example. The usefulness of the dashboard needs to be further evaluated, and studies are underway to assess its effectiveness for elements of ventilator care, including links to patient outcomes. The dashboard is continuing to evolve, with the addition of the capture of contraindications for some patients to particular interventions, and further enhancements to improve integration into clinical workflow. The dashboard is proving to be a useful tool for both real-time course correction and ongoing monitoring of high-quality ventilator management.
Figure 1.
Dashboard System Architecture
References
- 1.Bueno-Cavanillas A, Delgado-Rodriguez M, Lopez-Luque A, Schaffino-Cano S, Galvez-Vargas R. Influence of nosocomial infection on mortality rate in an intensive care unit. Crit Care Med. 1994;22:55–60. doi: 10.1097/00003246-199401000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Healthcare Improvement’s 5,000,000 Lives Campaign. http://www.ihi.org/IHI/Programs/Campaign/
- 3.Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recomm Rep. 2004 Mar 26;53(RR-3):1–36. [PubMed] [Google Scholar]
- 4.Dodek P, Kennan S, Cook D, et al. Evidence-Based Clinical Practice Guideline for the Prevention of Ventilator-Associated Pneumonia. Ann Intern Med. 2004;141:305–313. doi: 10.7326/0003-4819-141-4-200408170-00011. [DOI] [PubMed] [Google Scholar]
- 5.Tolentino-DelosReyes AF, Ruppert SD, Shiao PK. Evidence-Based Practice: Use of the Ventilator Bundle to Prevent Ventilator-Associated Pneumonia. American Journal of Critical Care. 2007;16:20–27. [PubMed] [Google Scholar]
- 6.Kollef MH. The prevention of ventilator-associated pneumonia. N Engl J Med. 1999;340:627–34. doi: 10.1056/NEJM199902253400807. [DOI] [PubMed] [Google Scholar]
- 7.McDonald CJ. Protocol-based computer reminders, the quality of care and the nonperfectibility of man. N Engl J Med. 1976 Dec 9;295(24):1351–5. doi: 10.1056/NEJM197612092952405. [DOI] [PubMed] [Google Scholar]
- 8.Starmer JM, Russ S, Jones I, Giuse D, Waitman LR, Doulis J, Aronsky D. Implementing Pneumonia Quality Care Measures with an Informatics-Driven Intervention. Proc AMIA Symp. 2007 [PubMed] [Google Scholar]
- 9.Stead WW, Starmer JM. Leadership Commitments to Improve Value in Health Care, Toward Common Ground: Workshop Summary. Washington, DC: The National Academies Press; 2008. Practical Frontline Challenges to Moving Beyond the Expert-based Practice. Institute of Medicine (IOM) [Google Scholar]
- 10.Stead WW, Patel N, Starmer JM.Closing the Loop in Practice to Assure the Desired PerformanceIn press, 2008 Trans Am Clin Climatol Association [PMC free article] [PubMed]