Abstract
Trauma Triage errors are frequent and costly. What happens in pre-hospital care remains anecdotal because of the dual responsibility of treatment (resuscitation and stabilization) and documentation in a time-critical environment. Continuous pre-hospital vital signs waveforms and numerical trends were automatically collected in our study. Abnormalities of pulse oximeter oxygen saturation (< 95%) and validated heart rate (> 100/min) showed better prediction of injury severity, need for immediate blood transfusion, intra-abdominal surgery, tracheal intubation and chest tube insertion than Trauma Registry data or Pre-hospital provider estimations. Automated means of data collection introduced the potential for more accurate and objective reporting of patient vital signs helping in evaluating quality of care and establishing performance indicators and benchmarks. Addition of novel and existing non-invasive monitors and waveform analyses could make the pulse oximeter the decision aid of choice to improve trauma patient triage.
Introduction
The American College of Surgeons projects that pre-hospital over-triage occurs in 30–50% of all patients who are taken to trauma centers and under-triage occurs in 5–15% who were transported to non-trauma centers, only to require later inter-hospital transfer to a trauma center. Thus there is a net estimated misdiagnosis rate of 35%, but this could be as high as 65%. The costs associated with triage errors for trauma patients in the U.S. are valued to be approximately $10 billion annually1. The site, extent, and severity of traumatic injuries are difficult to assess accurately under hostile emergency conditions, where level and type of care must be decided immediately. This is true, particularly of injuries occurring in the ‘hidden compartments’ of the body, the abdomen and chest. Currently, it is extremely difficult to accurately compile information and know what is happening in the pre –hospital care of the trauma patient because documentation is fraught with ommissions due to the dual task of treatment (resuscitation and stabilization) and record keeping. Collection of continuous vital signs signals (VS) is one way of addressing the deficiencies by providing information about the abnormal physiological state as a pre-cursor of life-saving interventions during pre-hospital trauma care and, thereby, help in establishing the evidence-base for triage decisions and Emergency Medical Services (EMS) Quality Management (QM). We hypothesized that analysis of continuous vital signs signals can improve QM documentation, predict injury severity scores (ISS), interventions and outcomes, including need for abdominal surgery better than the field care provider or the use of retrospectively completed Trauma Registry data.
Methods
We collected continuous VS to evaluate dynamic changes, response to interventions and linked these VS to field care providers predictions of abdominal surgery completed at the time of patient admission to the trauma center, and outcome as determined from the Trauma Registry.
Continuous real-time waveforms of the electrocardiogram (ECG), pulse oximetry (SpO2), end-tidal carbon dioxide (ETCO2) and numerical values of ECG heart rate (HR), SpO2 HR and Oxygen Saturation, and non-invasive blood pressure (NIBP), and Respiration were collected. Data was automatically recorded during helicopter EMS transport2,3,4 (Table 1). A PDA (HP-iPAQ) based real-time VS data and event record system was developed for this project. The system interfaces with the pre-hospital monitor device (Propaq model 206EL) through the RS 232 cable and a specially designed interface Black Box which stores all the waveforms and trends as a VS repository.
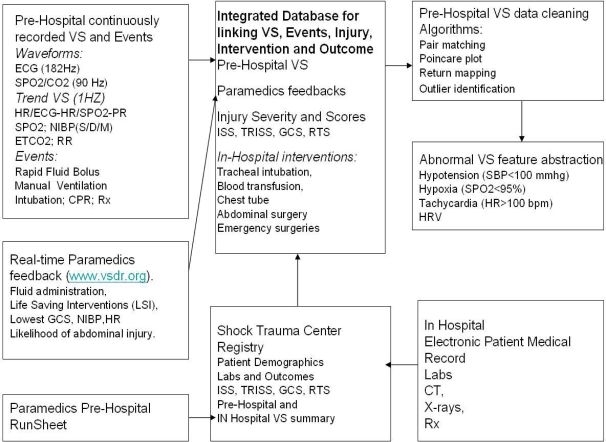
Table 1.
Pre-Hospital VS Prediction of Injury and Intervention Data Processing
The system can store up to 350 hrs (1 GB SD card) of waveforms (ECG at 182 Hz, SpO2/ETCO2 at 90 Hz) and numerical data (HR/SpO2/ETCO2 at 1Hz) for data mining, evaluation, processing and analysis. On arrival to the Trauma Center, the field care providers documented fluids, interventions, and their predictions of the need for intra abdominal surgery, on a scale of 1–5 (where 1= highly unlikely, 5 = highly likely).
Analysis consisted of evaluation of episodes of abnormalities (> 100/min) in ECG HR and SpO2 HR, oxygen saturation (< 95%) and NIBP (< 100 mmHg). To validate HR, a systematic process of artifact elimination was attempted. Strength of agreement between the ECG HR and Oximeter HR, evaluation of trendforms and expert inter-observer correlation matrix analysis were used as signal-noise enhancement strategies. Patient outcomes from the Trauma Registry data, their Injury Severity Score (ISS) >=15 and interventions (including blood transfusion, chest tube insertion, abdominal surgery, tracheal intubation) was linked to a combination of processed abnormal field VS; i.e. HR > 100/min +SpO2 < 95% and SBP<90 mm Hg. The specificity (a measure of over triage) and sensitivity (a measure of under triage) of abnormal VS was calculated for prediction of the need for life saving interventions and ISS. Unpaired t-tests and logistic regression techniques were used to detect differences in outcomes. P<0.05 was considered significant, data reported as mean +− standard deviation unless stated otherwise.
Results
Seventy patients underwent pre-hospital VS collection for 25.5 (Range 8–60) min of transport. Among these patients, VS parameters captured during helicopter flight were: SpO2 HR, 98.6%; respiratory rate, 30%, systolic/diastolic blood pressure, 98.6%; ECG waveforms, 95.7%, SpO2 waveform, 98.6%, ETCO2 4.3% and respiratory impedance waveforms 7.1%. VS data collection and outcomes were complete in 64 patients of whom 16 were severely injured with ISS >= 15. Subsequent data analyses included these 64 patients.
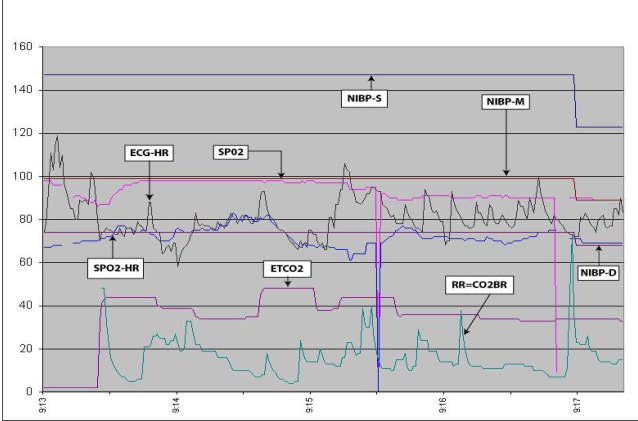
During pre-hospital transport, 3 patients required tracheal intubation and none underwent field Cardio Pulmonary Resuscitation (CPR). In the Trauma Center, 2 patients died, 3 had abdominal surgery, 4 required chest tube placement to relieve hemo or pneumothorax, 1 received blood immediately on arrival. Logistical regression of field provider diagnoses was 76% accurate for predicting abdominal surgery and 82% for abdominal surgery and chest tube insertion. Frequency of NIBP measurement varied from 3–10 times during transport. When the linkage of data between abnormal VS (ECG and SpO2 and NIBP) and outcomes were analyzed without the discontinuous NIBP data, there was no difference in predictions of interventions or injury severity. As a result validated HR data was used. Fifteen of the 64 patients had the defined combination of abnormal HR & SpO2. They had greater ISS (16±10.7 versus 8± 6.9 (p<0.02)) than the rest of the patients and included 3 out of 3 pre-hospital intubations, 2 out of 4 chest tube insertions, 2 out of 3 abdominal surgeries (missed 1 penetrating),1 of 1 blood transfusions within 1 hr, and 2 of 2 deaths (sensitivity = 50–100% / specificity = 78–85%). Three patients (1 pre-hospital intubation and 2 patients with ISS >= 15) were identified from the Trauma Registry using the same VS combination of SpO2 < 95% and HR > 100/min (sensitivity 0–33%). As an example of the QM potential of continuous VS waveforms, Fig 1 shows VS changes during 4 min associated with pre-hospital tracheal intubation, including oximeter desaturation to 90% lasting 2min 30 seconds, NIBP decrease following intubation from SBP 145 to 125 (and then to 104 mm Hg not shown in Fig 1). After tracheal intubation ETCO2 ranged from 48 – 23mm Hg and was mean 26 +− 3.2 mmHg during transport. Manual hyperventilation led to a nadir ETCO2 of 23 mm Hg, 7 min after intubation (not shown in Fig 1). Respiratory rate ranged between 5– 60/min with mean 14 +− 9.7 breaths/min after intubation. SpO2 HR is within 5% of ECG HR for about 1 min 30 sec of data shown in Fig 1
Figure 1.
Pre-Hospital Emergency Intubation Vital Signs
Discussion
Pulse oximetry, a current in-use EMS monitoring tool with the aforementioned additional potential of helping to improve triage decisions, is an exciting, but not unreasonable prospect. Shock is a compensated state and ventilation perfusion mismatch (V/Q) causing hypoxemia is an accompaniment to the early stages after injury. V/Q mismatch may only be intermittently revealed by events such as administration of analgesic or sedation drugs, tasks such as tracheal intubation or pain on positioning during resuscitation and stabilization. Decreased SpO2 in combination with the multi-causative physiological response of tachycardia is proposed as the new triage tool. If the HR value obtained from SpO2 is artifact free, validation by matching with ECG HR would be unnecessary. This could be obtained by SpO2 pulsatile waveform analysis5. ECG waveform analysis could add triage related information (HR variablility, R-R interval, respiratory rate) and confirm SpO2 HR6. In addition other existing non-invasive monitors (transcutaneous CO2, hemoglobin concentration) could be built into a pulse oximeter probe .It is not surprising that NIBP was unhelpful, as blood pressure is notoriously inaccurate as a marker for shock due to compensatory mechanisms which maintain pressure despite the loss of 30% or more of circulating blood to hemorrhage. In addition, as shown by continuous VS data collection, NIBP is only an intermittent data point. In some instances NIBP was only measured every 15 minutes, so that it is unlikely to be a predictor of dynamic events occurring in the severely injured patient.
Because VS waveforms were recorded as continuous data (as they are normally displayed to the field care provider), documentation of life saving events (management of Airway, Breathing, Circulation) and interventions (tracheal intubation), was obtained automatically by the dynamic VS waveforms. It is clear from these preliminary data that analysis of trends and waveforms may reveal even greater predictions of severity of injury. QM measures such as duration of abnormal VS, conformity to EMS protocols (e.g. ventilation of intubated patients can be determined from data such as that in Fig1) frequency of measurement (e.g. NIBP), time of scene management and transport were recorded without any interruption of field provider care for the patient. For Trauma Registry and QM documentation purposes, the current standard is for the field care provider to report one NIBP, SpO2 and HR as VS for the Pre-Hospital phase, which are entered into the Trauma Registry. This study suggests that with only the processed HR and SpO2 record, we could identify patients with high risk for injuries within the ‘hidden body compartments’ as well as those with severe injury (ISS>= 15). As such, these signals, dynamically processed, could be a simple triage tool, directing the need for Trauma Center care and reducing errors in triage.
The scope of over triage is illustrated by studies in Minnesota, California and Maryland. In Minnesota among 9174 trauma patients having, in retrospect, at least one triage criterion indicating that their level of injury required trauma center care, 60% were transported to non-trauma centers. Of cases with injury severity scores of greater than 15 as well as one triage criterion, 77% were taken to trauma centers. In two large counties, 58% and 27% of trauma patients were under-triaged and taken to trauma centers7 In Orange County CA, there was a 74% increase in over-triage after revisions to the Injury Severity Scoring System for motor vehicle crashes between 1981–1988, when more than 30,000 trauma patients were transported8. In a retrospective analysis in Maryland, of 1995 data among 32,950 trauma patient transports, 86% meeting injury triage criteria were appropriately transported to trauma centers, meeting mechanistic triage criteria (46%) and physiologic triage criteria (34%) 9.
The process of integrating multiple inputs in the triage process is difficult to teach or automate. In the battlefield or civilian life threatening circumstances, successful triage depends on the experience of the care provider. Because the course of intra- abdominal bleeding and peritoneal irritation from blood (causing abdominal pain) takes a finite time to develop, with short helicopter transport times the signs and symptoms of intra abdominal bleeding may not be apparent and may not be noted by the pre-hospital provider. Automated, continuous monitoring of VS can potentially facilitate more rapid, accurate triage and better treatment 10. The prime goal should be to develop decision support aids by using a commonly used device like the pulse oximeter capable of providing near real-time estimates of the level of injury early in the prehospital phase of trauma care.
For the patient with severe life-threatening abdominal or thoracic hemorrhage, the anatomic source of bleeding must be identified; this is the overarching principle of “The Golden Hour” of the Advanced Trauma Life Support (ATLS) course. The challenge for the pre-hospital care provider is to recognize the injured patient as early as possible, so that they can receive expedited diagnosis, early control of the source of bleeding and definitive trauma center care,. SpO2 and HR monitoring may be a promising real-time decision aid to enable this.
Conclusions
Data on EMS quality management is available from continuous VS collection, beyond that available in Trauma Registry data. Continuous data from the pulse oximeter oxygen saturation and HR are better predictors of need for abdominal surgery than pre-hospital clinicians. Pre-hospital episodes of low oxygen saturation may be surrogate for V/Q mismatch of shock which, in addition to the multi-causative increased HR, identifies high injury /intervention patients. Decreased SpO2 < 95% + HR > 100/min could be useful as a real-time triage decision aid and be improved with addition of novel and existing resuscitation monitors and VS waveform analyses.
Acknowledgments
This research was funded in part by the grants form DoD-TATRC #W81XWH-05-0374, W81XWH-06-C-0034, and W81XWH-07-2-0118. Additional institutional supports were provided by State Maryland Police Aviation Command, R Adams Cowley Shock Trauma Center, National Study Center for Trauma and EMS, University of Maryland School of Medicine, and Maryland Institute for Emergency Medical Services Systems (MIEMSS). We also like to thank Mr. Christopher Handley, MS, EMT-P for his support on statewide deployment of pre-hospital vital signs data collection network, Sean Jordan MHS, EMT-B, Anne Conway RN MS, Ryan Gens BA, Danny Ho MS, Rebecca Webb BA, CCRC, Betsy Kramer RN, David Overturf BA, Peter Smitt EMT, Lisa Gettings MS, Kelly Bochicchio, RN, MS, and Melvin Alexander MS, for their support on data collection, mining and processing.
References
- 1.Committee on Trauma, American College of Surgeons: Advanced Trauma Life Support Program for Doctors . Chicago: American College of Surgeons; 1997. [Google Scholar]
- 2.Hu P, Mackenzie C, Floccare D, et al. What is happening to the patient during Pre-Hospital Trauma Care? American Medical Informatics Association (AMIA) Annual Symposium Proceedings. 2006:p61. [PMC free article] [PubMed] [Google Scholar]
- 3.Hu P, Mackenzie C, Floccare D, et al. Challenges in Developing Real-Time In-Flight Patient Vital-Signs Data Collection System. American Telemedicine Association Annual Symposium Proceedings. 2008 [Google Scholar]
- 4.Hu P, Mackenzie C, Scalea T, et al. Real-time Patient Vital Sign Data Collection Network for Trauma Care. American Telemedicine Association Annual Symposium Proceedings. 2008 [Google Scholar]
- 5.Yu C, Liu Z, McKenna T, Reisner AT, Reifman J. A Method for Automatic Identification of Reliable Heart rates Calculated from ECG and PPG Waveforms. Journal of AMIA. 2006;1:309–320. doi: 10.1197/jamia.M1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooke WH, Salinas J, Convertino VA, et al. “Heart rate variability and its association with mortality in prehospital trauma patients.”. Journal of Trauma. 2006;60:363–370. doi: 10.1097/01.ta.0000196623.48952.0e. [DOI] [PubMed] [Google Scholar]
- 7.Baez AA, Lane PL, Sorondo B.System compliance with out-of-hospital trauma triage criteriaJournal of Trauma 2003; 54: 344–35J of Trauma 200354344–351. [DOI] [PubMed] [Google Scholar]
- 8.O’Rourke B, Bade RH, Drezner T. Trauma Triage ; A nine year experience. Ann Emerg Med. 1992;21:680–687. doi: 10.1016/s0196-0644(05)82779-9. [DOI] [PubMed] [Google Scholar]
- 9.Ma MH, Mackenzie EJ, Alcorat R, Kelen GD. Compliance with prehospital triage protocols for major trauma patients. Journal of Trauma. 1999;46:168–175. doi: 10.1097/00005373-199901000-00029. [DOI] [PubMed] [Google Scholar]
- 10.Hoyt R, Reifman J, Coster T, Buller M. “Combat Medical Informatics: Present and Future”. AMIA Annual Symposium Proceedings. 2002:335–339. [PMC free article] [PubMed] [Google Scholar]