Abstract
Many vendors of electronic medical records support structured and free-text entry of clinical documents using configurable templates. At a healthcare institution comprising two large academic medical centers, a documentation management data mart and a custom, Web-accessible business intelligence application were developed to track the availability and usage of electronic documentation templates. For each medical center campus, template availability and usage trends were measured from November 2007 through February 2008. By February 2008, approximately 65,000 electronic notes were authored per week on the two campuses. One site had 934 available templates, with 313 being used to author at least one note. The other site had 765 templates, of which 480 were used. The most commonly used template at both campuses was a free text note called “Miscellaneous Nursing Note,” which accounted for 33.3% of total documents generated at one campus and 15.2% at the other.
Introduction
Enabling healthcare providers to efficiently author documents in an electronic medical record (EMR) is challenging.1 Many commercial EMR vendors support both structured and free-text entry of clinical documents using configurable templates. This paper describes the design of a business intelligence tool for tracking usage of electronic documentation templates within a vendor-based electronic medical record.
Background
The setting for this research was NewYork-Presbyterian Hospital (NYP), composed of five main facilities located in and around New York City. NYP included two academic medical centers, NewYork-Presbyterian Hospital/Columbia University Medical Center, and NewYork-Presbyterian Hospital/Weill Cornell Medical Center, which together had over 2,200 patient beds. The foundation of the clinical information systems at NYP was a comprehensive clinical data repository (CDR) and clinical data warehouse (CDW). The CDR was a longitudinal electronic health record optimized for fast transactional processing to support patient care2, and the CDW facilitated queries and analyses across multiple patients to support quality improvement and research goals. The open architectural design of the clinical information systems enabled data integration from vendor systems as well as internal development.
Both the Columbia and Weill Cornell campuses of NYP recently completed the installation of a vendor-based electronic medical record (Eclipsys Sunrise Clinical Manager 4.5 XA, Eclipsys Corp., Atlanta, GA), which was being used in conjunction with several other commercial and locally-developed systems. The Eclipsys system was used for computerized provider order entry, and was also the primary source for clinical documentation entered by nursing and ancillary staff.
In 2007, hospital leadership encouraged physicians, physician assistants, and nurse practitioners to adopt electronic documentation within Eclipsys on a voluntary basis. Different providers were previously using a variety of methods for documentation, including paper forms, other computer applications3, and dictation. To support the migration to electronic documentation in Eclipsys, hundreds of free-text and structured documentation templates were created to supplement the pre-defined templates supplied by the vendor. Creating templates was an iterative process that typically paired an Information Technology analyst with a clinical domain expert. After passing a quality assurance check, locally-developed templates were made available to providers. Over time, the growing number of templates became difficult to manage, more so because templates used at the two hospital campuses were not always identical. Tracking the usage of templates was rarely performed because it required time- and labor-intensive database queries and manual aggregation of statistics.
Related research on transitioning to electronic documentation has identified several factors affecting adoption. These included organizational and clinical leadership; functionality and speed of the note-writing application; training; professional billing considerations; and workflow issues such as access to computers and time required to author notes electronically.4–7 Discussions have continued about the benefits and risks associated with copying and pasting text into EMRs.8,9 Other research has emphasized possible cognitive side-effects of electronic documentation, including disruptions to information flow and changes in the way providers obtain, organize, and reason with knowledge.10,11
Several investigators have pointed out benefits of developing an ontology or classification scheme for naming documents.12–14 Naming conventions are important because they may influence both the authoring process (i.e., the choice of which template to use), and the document review process (i.e., the speed and completeness of searching for data in a patient's health record). Furthermore, clinical document exchange between disparate computer systems is hindered by differences in document-naming practices across organizations. To address these problems, an ontology for clinical documents has been developed within the Health Level 7 (HL7) and Logical Observation Identifiers, Names, and Codes (LOINC) standards organizations. The HL7/LOINC document ontology enabled a rich polyhierarchical structure for classifying documents based on characteristics such as the role of the author, the purpose of the note, and the location of care (e.g., inpatient vs. outpatient).
Methods
Care providers entered structured and free-text clinical notes using the Eclipsys “Document Entry Worksheet.” The note-authoring application allowed a care provider to select a documentation template in two ways: 1) using a “tree” widget which displayed a three-level hierarchy of template names (e.g., Inpatient Physician/Provider Notes → Medicine → Medicine Attending Follow-up Note); or 2) picking the desired template from a dynamically filtered list, where filtering was performed by matching template names with user-entered text in a search field. Some advanced users configured the application to display by default a short list of templates relevant to them (known as “Personal Documents”), but anecdotal evidence suggested that this feature was not commonly used.
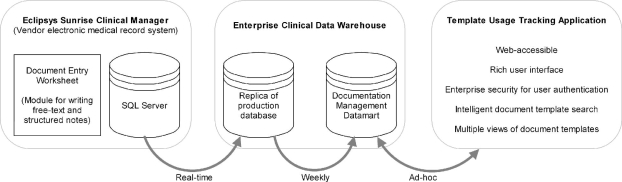
Figure 1 shows an architectural diagram of information systems that existed or were developed to support a clinical documentation template usage tracking application. Notes authored in the Eclipsys Document Entry Worksheet were stored in the system’s SQL Server database (Microsoft Corp., Redmond, WA). Real-time replication of the SQL Server database into the enterprise clinical data warehouse was accomplished using Transactional Data Management software (GoldenGate Software, Inc., San Francisco, CA). A data mart for documentation management was created within the CDW and was updated weekly with template maintenance information and usage statistics.
Figure 1.
Information systems architecture supporting a clinical documentation template usage tracking application.
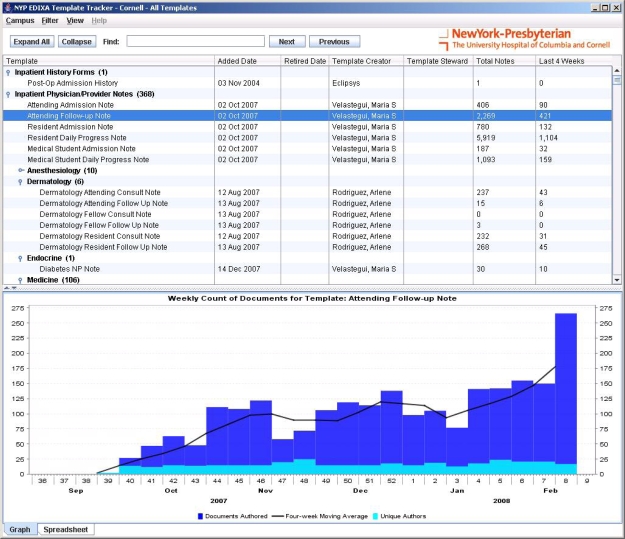
A Web-accessible tool was developed in Java (Sun Microsystems, Inc., Santa Clara, CA) for the purpose of tracking the availability and usage of electronic documentation templates (see Figure 2). Features of the template tracking tool included:
Figure 2.
Web-accessible tool for tracking the availability and usage of clinical documentation templates at NewYork-Presbyterian Hospital.
a rich user interface developed with Java Swing and JFreeChart (www.jfree.org) that provided interactive graphical displays of usage trends for both individual templates as well as for composite groupings of templates;
enterprise security based on the Lightweight Directory Access Protocol (LDAP) for authenticating users to the application;
an intelligent search mechanism for locating templates; and
multiple views of document templates, including a fully sortable list (e.g., by template creation date or number of documents authored) in addition to a tree-based (hierarchical) view comparable to the Eclipsys display.
Using the template tracking application, an analysis was undertaken to identify template availability and usage trends from November 2007 through February 2008. The documentation management data mart created in the CDW was based on one-week granularity for storing data; because of this, the analysis considered November to be weeks 44–48, December to be weeks 49–52, January to be weeks 1–5, and February to be weeks 6–9. (Determination of the week of year was performed according to the International Organization for Standards ISO8601 specification.)
The analysis of template availability and usage trends was performed for the Columbia and Weill Cornell campuses of NYP. The analysis examined the number of templates available at the end of each month, and the number of templates added or “retired” during each month. Additional measurements included the number of templates used to author at least one note during each month, as well as the average weekly count of notes for three categories: Physician/Provider, Nursing, and Ancillary. (Ancillary included domains such as respiratory car, physical therapy, social work, and nutrition.) Finally, the most frequently used templates were identified for each campus.
Results
At the end of November 2007, there were 907 templates available in the Eclipsys system at the NYP/Columbia University Medical Center campus; by February 2008, there were 934 templates (see Table 1). The number of templates at the NYP/Weill Cornell Medical Center campus increased from 704 in November 2007 to 765 in February 2008. About 30% of templates at the NYP/Columbia campus were used to write notes each month compared to around 60% for NYP/Weill Cornell. The largest volume of notes for both campuses was generated with nursing documentation templates.
Table 1.
Template availability and usage data for each hospital campus from November 2007 through February 2008.
| Nov. 2007 | Dec. 2007 | Jan. 2008 | Feb. 2008 | |
|---|---|---|---|---|
| NewYork-Presbyterian/Columbia University Medical Center | ||||
| Available templates | 907 | 909 | 923 | 934 |
| Templates added | 1 | 2 | 26 | 12 |
| Templates retired | 0 | 0 | 9 | 1 |
| Number of templates used to author ≥1 note | 281 | 263 | 292 | 313 |
| Average weekly count of Physician/Provider Notes | 2,984 | 2,618 | 2,854 | 3,298 |
| Average weekly count of Nursing Notes | 17,687 | 16,220 | 17,145 | 18,751 |
| Average weekly count of Ancillary Notes | 8,412 | 8,178 | 9,169 | 9,398 |
| NewYork-Presbyterian/Weill Cornell Medical Center | ||||
| Available templates | 704 | 705 | 757 | 765 |
| Templates added | 6 | 2 | 65 | 9 |
| Templates retired | 0 | 1 | 11 | 1 |
| Number of templates used to author ≥1 note | 413 | 405 | 460 | 480 |
| Average weekly count of Physician/Provider Notes | 10,984 | 10,947 | 11,419 | 12,336 |
| Average weekly count of Nursing Notes | 13,771 | 13,268 | 13,840 | 14,252 |
| Average weekly count of Ancillary Notes | 6,581 | 6,350 | 6,718 | 7,102 |
A list of the most frequently used templates for each campus is shown in Table 2. The most used template on both NYP hospital campuses was a free-text “Miscellaneous Nursing Note.” At NYP/Columbia, this template accounted for 33.3% of all documents authored in the Eclipsys note-writing application. The Miscellaneous Nursing Note template was responsible for 15.2% of all Eclipsys documents written at NYP/Weill Cornell. The 10 most common templates at NYP/Columbia were used to create 61.7% of total documents, while the top 10 templates at NYP/Weill Cornell accounted for 41.1% of notes authored there.
Table 2.
The ten most frequently used templates for each NewYork-Presbyterian (NYP) hospital campus, and cumulative percentage of total documents authored for which each template was responsible.
| NYP/Columbia | NYP/Weill Cornell | ||
|---|---|---|---|
| Template | Cum. % | Template | Cum. % |
| Miscellaneous Nursing Note | 33.3 | Miscellaneous Nursing Note | 15.2 |
| Respiratory Care Patient Assessment | 37.8 | Medicine Resident Daily Progress Note | 20.2 |
| RT Plan of Care | 42.4 | SW Progress Note-Adult | 23.8 |
| Physical Therapy | 45.9 | Respiratory Care Patient Assessment | 26.9 |
| Restraints Maintained: 2Pt Wrist | 49.0 | Problem | 29.4 |
| Nutrition Assessment | 52.0 | RT Plan of Care | 31.8 |
| OB/GYN Miscellaneous | 54.8 | PACU Continuation Note | 34.2 |
| SW Progress Note-Adult | 57.6 | Admission/Receiving | 36.6 |
| SW High Risk Screen | 59.9 | Nutrition Assessment | 38.9 |
| Case Manager Plan of Care | 61.7 | General Surgery Note | 41.1 |
Discussion
The creation of an enterprise documentation management data mart facilitated the development of a template usage tracking application. The tracking application minimized the effort required to identify trends and calculate statistics related to template usage. Based on a four-month analysis of documentation template usage patterns, several interesting results were identified.
First, only a fraction of the available templates were used by care providers writing clinical notes (30% at one campus, 60% at the other). This finding has provoked discussion about the “template life cycle,” i.e., specifying policies and procedures for creating, modifying, combining, sharing, and retiring templates. A graphical trend of template usage over time, for example, is a powerful tool for determining whether templates are being used appropriately, compared to being underused, overused, or not used at all. Before the availability of the tracking application, templates at our institution were seldom retired—typically only when a template was replaced by an updated version. Having access to the usage frequency for each template allows system administrators to judiciously prune unused templates, resulting in a more organized and parsimonious collection of templates available for clinical documentation.
Second, a small number of templates was responsible for most of the electronic notes that were written. At one campus, “Miscellaneous Nursing Notes” constituted one-third of the total. Payne et al. reported a similar finding, where 32 out of 244 available templates (13.1%) accounted for 75% of all notes authored.14 Additional exploration is warranted to determine important characteristics of frequently used templates (e.g., whether they use structured vs. free-text entry, average time authors spend writing each note) and how templates can be optimized to support clinical workflow.
Conclusions
The results of this research suggest that management of electronic documentation templates is important for improving the overall quality of clinical documentation. There is a high degree of complexity involved in managing large libraries of templates. It is recommended for commercial vendors of electronic documentation tools to reduce complexity by incorporating the existing HL7/LOINC standard for naming clinical documents.13 Names of electronic clinical documents within institutions should be derived from—or mapped to—the standard in order to streamline document sharing among healthcare providers.
References
- 1.Wilcox AB, Narus SP, Bowes WA., 3rd Using natural language processing to analyze physician modifications to data entry templates. AMIA Annu Symp Proc. 2002:899–903. [PMC free article] [PubMed] [Google Scholar]
- 2.Hripcsak G, Cimino JJ, Sengupta S. WebCIS: large scale deployment of a Web-based clinical information system. Proc AMIA Symp. 1999:804–808. [PMC free article] [PubMed] [Google Scholar]
- 3.Stetson PD, Keselman A, Rappaport D, et al. Electronic discharge summaries. AMIA Annu Symp Proc. 2005:1121. [PMC free article] [PubMed] [Google Scholar]
- 4.Apkon M, Singhaviranon P. Impact of an electronic information system on physician workflow and data collection in the intensive care unit. Intensive Care Med. 2001;27:122–130. doi: 10.1007/s001340000777. [DOI] [PubMed] [Google Scholar]
- 5.Embi PJ, Yackel TR, Logan JR, et al. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc. 2004;11:300–309. doi: 10.1197/jamia.M1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Payne TH, Perkins M, Kalus R, et al. The transition to electronic documentation on a teaching hospital medical service. AMIA Annu Symp Proc. 2006:629–633. [PMC free article] [PubMed] [Google Scholar]
- 7.Puffer MJ, Ferguson JA, Wright BC, et al. Partnering with clinical providers to enhance the efficiency of an EMR. J Healthc Inf Manag. 2007;21:24–32. [PubMed] [Google Scholar]
- 8.Hirschtick RE. A piece of my mind. Copy-and-paste. JAMA. 2006;295:2335–2336. doi: 10.1001/jama.295.20.2335. [DOI] [PubMed] [Google Scholar]
- 9.Yackel TR, Embi PJ. Copy-and-paste-and-paste. JAMA. 2006;296:2315–2316. doi: 10.1001/jama.296.19.2315-a. [DOI] [PubMed] [Google Scholar]
- 10.Patel VL, Kushniruk AW, Yang S, et al. Impact of a computer-based patient record system on data collection, knowledge organization, and reasoning. J Am Med Inform Assoc. 2000;7:569–585. doi: 10.1136/jamia.2000.0070569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weir CR, Hurdle JF, Felgar MA, et al. Direct text entry in electronic progress notes: An evaluation of input errors. Methods Inf Med. 2003;42:61–67. [PubMed] [Google Scholar]
- 12.Shapiro JS, Bakken S, Hyun S, et al. Document ontology: supporting narrative documents in electronic health records. AMIA Annu Symp Proc. 2005:684–688. [PMC free article] [PubMed] [Google Scholar]
- 13.Frazier P, Rossi-Mori A, Dolin RH, et al. The creation of an ontology of clinical document names. Medinfo. 2001;10:94–98. [PubMed] [Google Scholar]
- 14.Payne TH, Kalus R, Zehner J. Evolution and use of a note classification scheme in an electronic medical record. AMIA Annu Symp Proc. 2005:599–603. [PMC free article] [PubMed] [Google Scholar]