Abstract
Medical procedures in outpatient settings have limited options of managing pain and anxiety pharmacologically. We therefore assessed whether this can be achieved by adjunct self-hypnotic relaxation in a common and particularly anxiety provoking procedure. 236 women referred for large core needle breast biopsy to an urban tertiary university-affiliated medical center were prospectively randomized to receive standard care (n=76), structured empathic attention (n= 82), or self-hypnotic relaxation (n=78) during their procedures. Patients’ self-ratings at 10 minute-intervals of pain and anxiety on 0–10 verbal analog scales with 0=no pain/anxiety at all, 10=worst pain/anxiety possible, were compared in an ordinal logistic regression model. Women’s anxiety increased significantly in the standard group (logit slope = 0.18, p < 0.001), did not change in the empathy group (slope = −0.04, p = 0.45), and decreased significantly in the hypnosis group (slope = −0.27, p < 0.001). Pain increased significantly in all three groups (logit slopes: standard care = 0.53, empathy = 0.37, hypnosis = 0.34; all p < 0.001) though less steeply with hypnosis and empathy than standard care (p = 0.024 and p = 0.018 respectively). Room time and cost were not significantly different in an univariate ANOVA despite hypnosis and empathy requiring an additional professional: 46 minutes/$161 for standard care, 43 minutes/$163 for empathy, and 39 minutes/$152 for hypnosis. We conclude that, while both structured empathy and hypnosis decrease procedural pain and anxiety, hypnosis provides more powerful anxiety relief without undue cost and thus appears attractive for outpatient pain management.
1. Introduction
Medical procedures in outpatient settings have limited options of managing pain and anxiety pharmacologically. Nonpharmacologic adjuncts in these busy settings are largely under-investigated. This leaves patients with little help. The situation is aggravated when the procedure involves pain and is highly anxiety provoking. We therefore chose large core breast biopsy as a model in which to assess the efficacy of biobehavioral interventions.
Breast cancer is one of the most common and feared cancers among women, affecting as many as one in eight (American Cancer Society 2005). Screening mammography enables early detection and can improve chances of successful treatment and survival (Tabar et al. 2003). In the US, more than 60% of women aged 40 or older undergo mammography each year (Centers of Disease Control and Prevention (CDC) 2002). Five to ten percent of mammograms yield abnormal or inconclusive results that require further work-up (American Cancer Society 2005). For these patients and also those with lumps found by palpation, image-guided large core needle biopsy (LCNB) has evolved as a reliable diagnostic tool (Meyer et al. 1999).
LCNB is typically performed in outpatient settings with local anesthetic (American College of Radiology 2000) which reduces cost (Groenewoud et al. 2004) but limits the use of intravenous drugs to reduce pain and anxiety. Some advocate the use of oral anxiolytics (van Vlymen et al. 1999; Bugbee et al. 2005) but these restrict patients from driving and working after the procedure. In a mammography study, psychological intervention was found to reduce distress in select patients (Caruso et al. 2001). In a study of breast biopsies, relaxation treatment yielded no demonstrable effects (Bugbee et al. 2005). Encouraged by a prior report which showed less pain, anxiety, and need for intravenous medication in patients having self-hypnotic relaxation during more invasive medical procedures (Lang et al. 2000), we hypothesized that such an intervention could reduce pain and anxiety in patients undergoing LCNB. Thus we designed the following prospective randomized trial.
2. Methods
2.1. Patients
Review boards of the institution and the funding agency approved this study. Outpatients referred for LCNB in the Radiology Department of an urban, tertiary, University-affiliated Medical Center who were willing and able to give written informed consent and were able to hear and understand English were eligible for this study. Consecutive eligible patients were asked to participate in this study to assess the effect of a self-hypnotic relaxation exercise applied in addition to local anesthetic. Patients who passed screening for mental impairment with the Mini Mental-State Exam (Folstein et al. 1975) and for psychosis with the Schedule for Affective Disorders and Schizophrenia (Spitzer and Endicott 1979) were randomly assigned to receive standard care treatment, empathy, or self-hypnotic relaxation treatment on the procedure table.
2.2. Large Core Needle Biopsy
Breast biopsy was performed according to standard clinic practice using povidone scrub, local anesthetic, a 5mm-wide blade incision for insertion of an 11 or 14 gauge biopsy gun (Bard, Covington, GA), ultrasonographic or radiographic guidance, and steri strips for closing wound margins. For local anesthesia 5 mL 1% lidocaine were used superficially and 10 mL 1% lidocaine with epinephrine for the depth. Patients had neither before nor during the procedure oral or peroral anxiolytics or analgesics.
Adverse events were recorded according to the Standards of the Society of Interventional Radiology (Sachs et al. 2003). Room time was defined as the time the patient occupied the procedure room. Total procedure costs were based on calculations suggested for mammography teams (Raza et al. 2001) using the following local cost per minute: $2.135 for staff radiologists, $0.692 for fellows/ residents, $0.726 for technologists, $0.730 for room and equipment, and $0.373 for the research assistants providing empathy and hypnosis.
2.3. Test and Control Treatments
The experiment included three conditions: Standard care, Empathy, and Hypnosis. The behaviors that define the Empathy condition were also included in the Hypnosis condition. The empathy behaviors were designed to develop rapid rapport and set the stage for inducing hypnosis in even hypnosis-naïve patients. Since these behaviors alone might affect reported pain and anxiety, they were included in a separate empathic attention control condition.
As standard care, the biopsy team attempted to comfort patients in their usual way: they warned of upcoming stimuli, asked patients about their experience, commiserated with them about discomfort, and generally expressed sympathy.
The Empathy condition was defined by a set of structured attentive behaviors engaged in by a research assistant. These behaviors were standardized according to a manual and proven suitable for invasive procedures in radiology (Lang and Berbaum 1997; Lang et al. 1999) The behaviors included matching the patient’s verbal and nonverbal communication pattern, listening attentively, providing the perception of control (“Let us know at any time what we can do for you”), swiftly responding to patient’s requests, encouraging the patient, avoiding negatively-valued language (e.g “You will feel a burn and a sting”), and use of emotionally neutral descriptors instead (“This is the local anesthetic”).
In the Hypnosis condition, patients received all of the attentive behaviors used in the Empathy condition. In addition, the research assistant read a standardized hypnotic induction script (Lang et al. 1999), and, as needed, addressed the patient’s anxiety, pain, or worries according to the prescriptions of the script. The script invited patients to roll their eyes upwards, close their eyes, breathe deeply, focus on a sensation of floating, and experience a pleasant setting of their choice with all their senses. The text suggested transforming potential discomfort into a sensation of warmth, coolness, or tingling. If needed, a provision in the script guided patients to project their worries and fears onto the left side of an imaginary split screen and find solutions on the right side of the screen. The research assistants coached the patients according to the script in developing their own imagery and solutions to further the self-hypnotic process. The script is included in the appendix.
The research assistants included one male and one female physician, two female medical students, and one female premedical student with a background in mental health sciences. They had received standardized training in empathic structured attention and hypnosis under supervision of physicians and psychologists. The training included workshops, teaching videos, reading material, a web-based course, and supervised practice with patients (Lang and Berbaum 1997; Lang et al. 1999; Lang et al. 2002). Only individuals who reliably mastered all key component behaviors were allowed to serve as research assistants in the study.
The research assistants were monitored to assess their adherence to prescribed and proscribed behaviors for each of the three treatment conditions (Moncher and Prinz 1991). Procedures were videotaped throughout the study. Fifty-seven randomly selected videotapes (24%) were analyzed by two reviewers not involved in the procedures. In assessing key behaviors, the reviewers had an inter-rater reliability of 0.73. The research assistants demonstrated high adherence to the protocol. The reviewers noted that the behavior of the biopsy team was relatively unaffected by that of the research assistant. Team members used their characteristic vocabulary and mannerisms under all three conditions.
2.4. Measures of Anxiety and Pain
Prior to entering the procedure room, patients were given a Spielberger State Anxiety Questionnaire (STAI-Y) (Spielberger 1983) which assessed their baseline anxiety with a summary score between 20 and 80. In the procedure room, verbal 0–10 scales were used to evaluate the patients’ pain and anxiety. A rating of 0 indicated “no pain” or “no anxiety” and 10 indicated “worst possible pain,” or “worst possible anxiety”(Murphy et al. 1988; Paice and Cohen 1997; Benotsch et al. 2000). Patients were asked to make pain and anxiety ratings every 10 minutes These scales were used because patient’s self-report is considered the single most reliable descriptor of the pain experience (National Institutes of Health 1987; Acute Pain Management Guideline Panel 1992).
2.5. Experimental Design
Computer-generated random numbers contained on cards in sealed envelopes were used for treatment group assignment. Patients remained in their assigned group regardless of their reaction to the treatment. A research assistant obtained the patient’s informed consent, performed the screening, and supplied the STAI questionnaire. Randomization envelopes were opened just prior to patient entry into the biopsy room. The research assistant also obtained pain and anxiety ratings during the procedure.
2.6. Statistical Methods
Prior to this study, a power analysis was performed to identify an appropriate sample size. This analysis was based on the intention to perform a repeated measures analysis of pain and anxiety to compare trends in ratings for the three treatment groups over the procedure time (Laird and Ware 1982; Jennrich and Schluchter 1986). The analysis suggested that sample size of 240 patients would provide an 80% probability of detecting differences in trends as small or smaller than those seen in prior work (Lang et al. 2000). The power analysis was based on the assumption that patient ratings would be normally distributed. The pain ratings from this study, however, were clearly not normally distributed (47% of pain responses were zero). To accommodate the strong skew in reported pain, we changed our statistical approach to ordinal regression (Long 1997). Although reported anxiety data did not exhibit marked non-normality among its levels, for ease of understanding, a similar analysis was used for that variable.
We assumed that treatment groups shared a common intercept, and that each had its own linear trend term (slope). We tested whether the intercept differed from zero, whether the groups’ trends differed from zero, and whether trends differed between groups.
Owing to the sparseness of data in the highest response categories of pain and anxiety, we recoded categories 9 to 10 as category 8, yielding 0 to 8 scales. This is equivalent to collapsing rating categories of 8, 9, and 10 into a single category. This recoding affected less than 4% of the data overall on pain and less than 9% of the data overall on anxiety. The recoding allowed the proportional odds assumption of ordinal regression to be met. Statistical analyses were performed using PROC NLMIXED in SAS 8.2 (SAS Institute 1999). Results are presented in terms of the slopes of the time course of pain and anxiety on the logit scales. Significant deviations from 0 (no change over time) were accepted as positive or negative trends and compared among groups using two-sided tests.
Room time and cost were compared among groups by means of univariate analyses of variance with a between-patient factor for treatment group (Standard, Attention, Hypnosis) (Kirk 1995). Logarithmic transformation was applied to remove skewness from the time and cost data; however, results are presented in terms of the original scales (Kirk 1995). Differences in frequencies of adverse effects among the treatment groups were tested by Fisher exact tests.
3. Results
3.1. Patient Profile
Between February 2002 and March 2004, 240 eligible patients were recruited and randomly assigned to treatments (Fig.1). Four patients (including the only male) withdrew after entering the biopsy suite. The final groups included 76 patients in the Standard group, 82 patients in the Empathy group, and 78 patients in the Hypnosis group. Groups were relatively homogenous with regard to their personal and biopsy characteristics (Table 1).
Fig. 1.
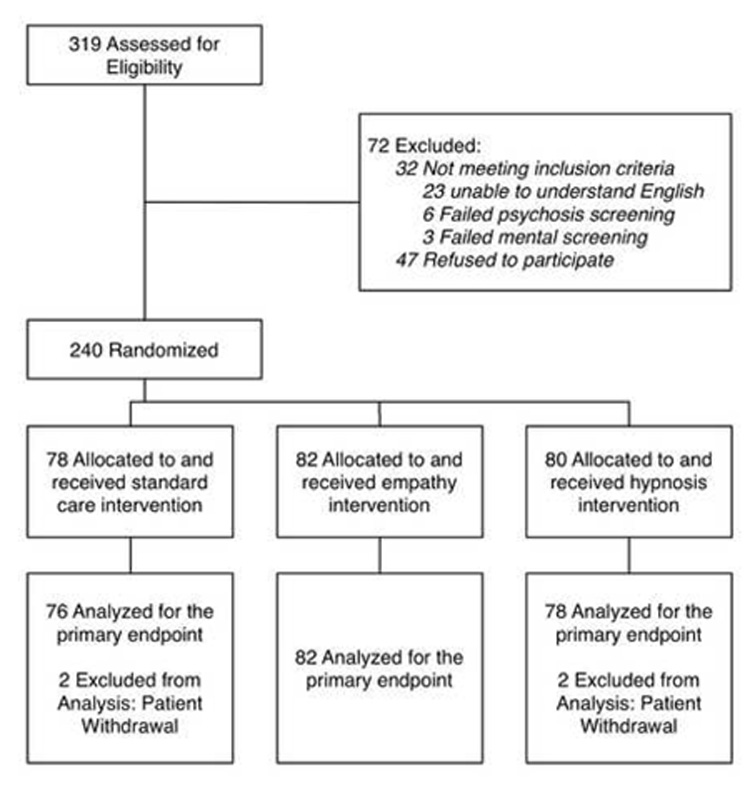
Flow Chart of Enrollment
Table 1.
Patient Characteristics
| Characteristic | Standard (n=76) | Empathy (n=82) | Hypnosis (n=78) |
|---|---|---|---|
| Age – years; median (range) | 50 (18 –82) | 47 (19–86) | 49 (22–84) |
| Weight – kg; median (range) | 71 (48–108) | 70 (43–154) | 69 (41–116) |
| Ethnicity | |||
| Caucasian | 57 | 67 | 66 |
| African American | 10 | 8 | 7 |
| Hispanic | 5 | 2 | 2 |
| Asian | 4 | 3 | 3 |
| Pacific Islander | 0 | 1 | 0 |
| More than one | 0 | 1 | 0 |
| Age of menarche – years; median (range) | 12.5 (9–17) | 12.7 (9–17) | 12.7 (10–16.5) |
| State Anxiety – STAI-Y; median (range) | 47 (20–77) | 49 (20–64) | 47 (20–77) |
| Image Guidance | |||
| Ultrasound | 43 | 55 | 48 |
| Stereotactic mammography | 33 | 27 | 30 |
| Biopsy result | |||
| Cancer | 17 | 22 | 19 |
| Benign | 34 | 36 | 38 |
| Increased risk lesion* | 6 | 5 | 4 |
| Biopsy not completed, assumed benign lesion¶ | 12 | 10 | 9 |
| Biopsy not completed because of technical reasons†† | 7 | 9 | 8 |
Increased risk lesions were defined as those which may not be clearly malignant but for which surgical removal is recommended (e.g., atypical lobular hyperplasia, atypical ductal hyperplasia, lobular carcinoma in situ).
Lesions were assumed to be benign when aspiration yielded fluid (cysts) or imaging during biopsy attempt showed the lesion to be smaller or resolved
Biopsies were not completed for technical reasons such as the lesion being too close to the chest wall or skin, and surgical biopsy was recommended.
3.2. Validation of Statistical Model
Using the 0–8 pain and anxiety scales, we tested the proportional odds assumption of ordinal regression by comparing the reported model to one in which a full set of category-specific slopes were employed, but the alternative model did not offer a significant improvement (likelihood ratio test G2 = 27.1, df = 21, p = 0.17 for pain, and G2 = 21.8, df = 21, p = 0.41 for anxiety). Thus the assumption was not violated. We also tested whether different intercepts among groups were required; they were not (p = 0.19 for pain, and p = 0.52 for anxiety), indicating group equivalence following randomization and suitability of the common intercept model (common pain intercept = −0.94, p < 0.001; common anxiety intercept = 4.41, p < 0.001). Thus the statistical model was validated for use in the analyses.
3.3. Anxiety and Pain
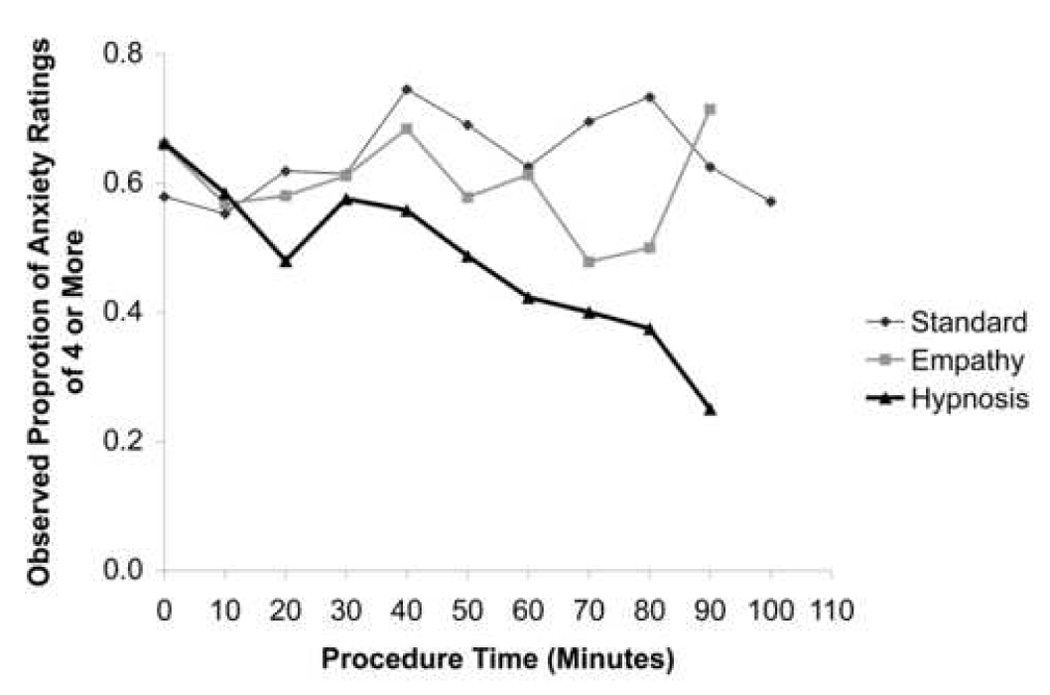
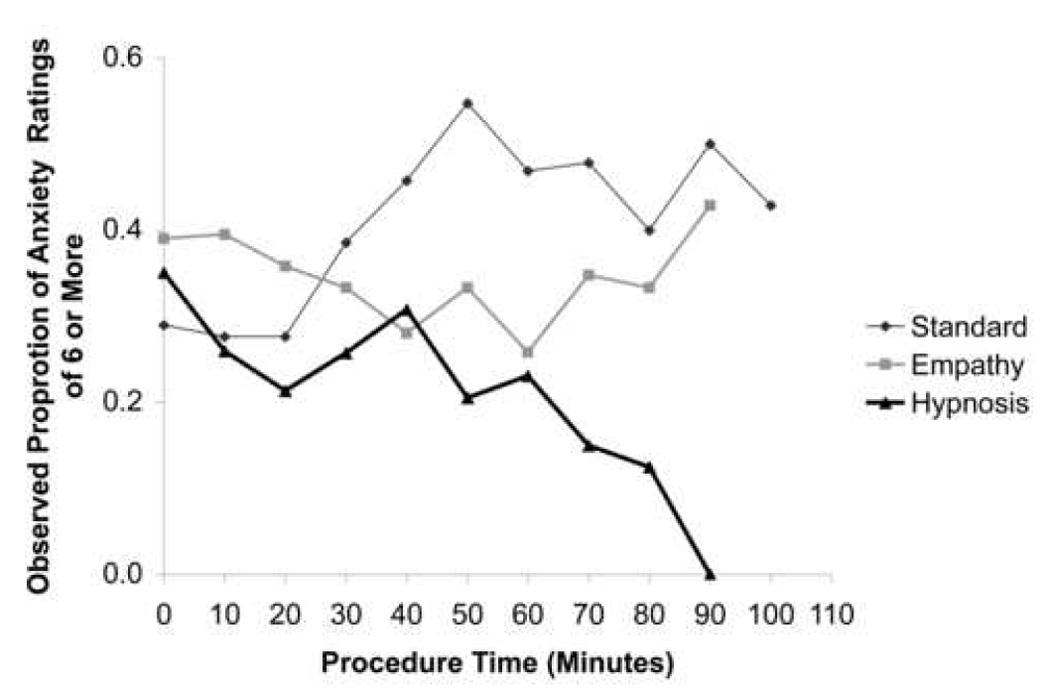
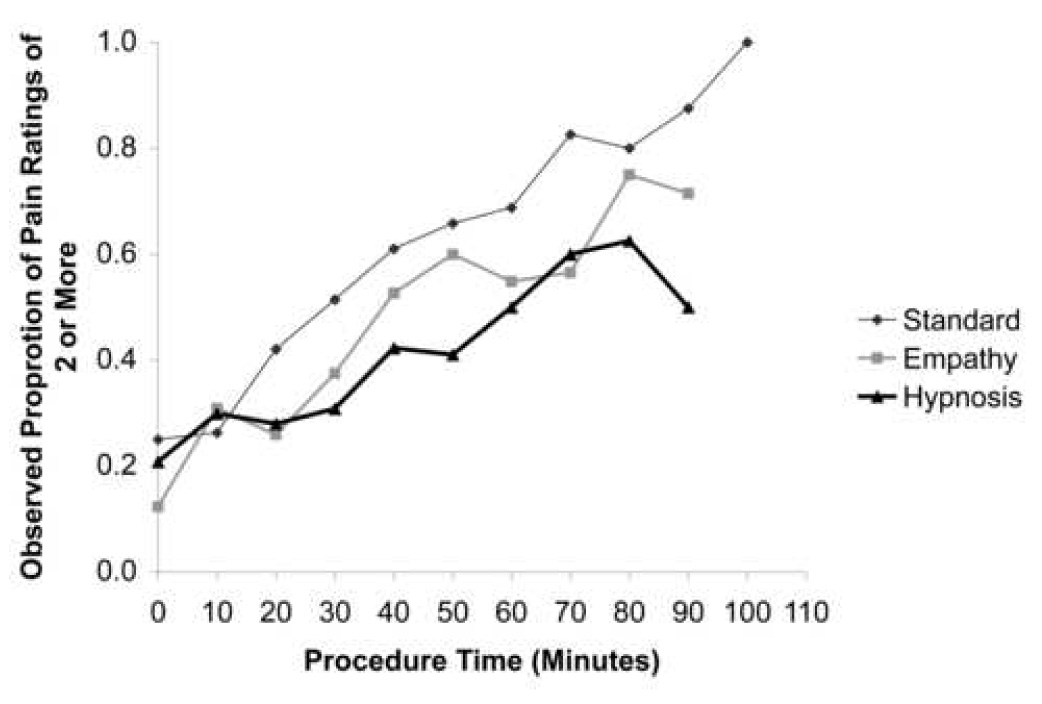
Table 2 gives a sense of the raw data for illustrative purposes. Ordinal regression analysis looks at data as a series of possible splits of patient responses and assesses the odds of experiencing a value at or above as compared to below the splits. Fig. 2 and Fig. 3 demonstrate examples of splits showing the change over time in the observed proportions of pain or anxiety responses at level ≥2 , ≥ 4, and ≥6 as compared to lower levels. Graphs, not presented here, showing all other splits of the ordinal data (e.g. level 0 vs. 1–10; 0–2 vs. 3–10; 0–4 vs. 5–10; 0–6 vs. 7–10; 0–7 vs. 8–10) gave similar results with lines representing splits at higher split points (e.g. 0–6 vs. 7–10) lying lower than those representing splits at lower split points (e.g. 0 vs. 1–10) as is also seen in Fig. 2 and Fig. 3. When fitting slopes that represent the lines using ordinal regression, positive slopes indicate an increase of pain or anxiety responses above the split point over time, negative slopes indicates a decrease, flat lines indicate no significant change. In the proportional odds model, an encompassing slope - a probability function or linear trend - is generated that not only applies to the logit form of individual splits (such as the three splits in Fig 2 and 3) but to the logit forms of graphs that portray all other splits.(Long 1997) The resultant representative slopes then facilitate comparison among groups.
Table 2.
Descriptive Statistics for Ratings of Anxiety and Pain as a Function of Room Time Presented solely for illustrative purposes, these Table gives unconnected “snapshots” across the procedure not taking into account the longitudinal nature of the ordinal data. Because of the skew of the data, medians and interquartile ranges (25th to 75th percentile range) are given as measures of center and variability. N refers to number of patients providing ratings at any given time interval.
| Ratings of Anxiety | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Standard of Care | Empathy | Hypnosis | |||||||
| Time (Min) | Median | N | Inter-Quartile Range | Median | N | Inter-Quartile Range | Median | N | Inter-Quartile Range |
| 0 | 4.5 | 76 | (2 – 6) | 5 | 82 | (3 – 7) | 5 | 78 | (3 – 6) |
| 10 | 4 | 76 | (2 – 6) | 4 | 81 | (2 – 7) | 4 | 77 | (2 – 6) |
| 20 | 4 | 76 | (2 – 6) | 4 | 81 | (2 – 7) | 3 | 75 | (2 – 5) |
| 30 | 4 | 70 | (2 – 6.25) | 4.5 | 72 | (2 – 6) | 4 | 66 | (2 – 6) |
| 40 | 5 | 59 | (3 – 7) | 5 | 57 | (3 – 6) | 4 | 52 | (1.25 – 6) |
| 50 | 6 | 42 | (2.75 – 7) | 4 | 45 | (2 – 6) | 3 | 39 | (1 – 5) |
| 60 | 5 | 32 | (2.25 – 8) | 4 | 31 | (2 – 6) | 2.5 | 26 | (0 – 5.25) |
| 70 | 5 | 23 | (3 – 8) | 3 | 23 | (2 – 6) | 2.5 | 20 | (0 – 4) |
| 80 | 5 | 15 | (2 – 8) | 4 | 12 | (2 – 6) | 3 | 8 | (0 – 4.75) |
| 90 | 5 | 8 | (0.5 – 8.75) | 5 | 7 | (1 – 8) | 0.5 | 4 | (0 – 4) |
| 100 | 4 | 7 | (0 – 9) | 3 | 5 | (0 – 5.5) | 2 | 5 | (0 – 5) |
| 110 | 4.5 | 4 | (0.5 – 8.5) | 2 | 2 | (0 – 3) | 5 | 1 | (5 – 5) |
| Ratings of Pain | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Standard of Care | Empathy | Hypnosis | |||||||
| Time (Min) | Median | N | Inter-Quartile Range | Median | N | Inter-Quartile Range | Median | N | Inter-Quartile Range |
| 0 | 0 | 76 | (0 – 1.75) | 0 | 81 | (0 – 0) | 0 | 78 | (0 – 1) |
| 10 | 0 | 76 | (0 – 2) | 0 | 81 | (0 – 1) | 0 | 77 | (0 – 2) |
| 20 | 1 | 76 | (0 – 4) | 0 | 81 | (0 – 2) | 0 | 75 | (0 – 2) |
| 30 | 2 | 70 | (0 – 4) | 0 | 72 | (0 – 3) | 0 | 65 | (0 – 2) |
| 40 | 2 | 59 | (0 – 5) | 2 | 57 | (0 – 4) | 0 | 52 | (0 – 3) |
| 50 | 4 | 41 | (0 – 6) | 2 | 45 | (0 – 4.5) | 1 | 39 | (0 – 3) |
| 60 | 2.5 | 32 | (0 – 4) | 2 | 31 | (0 – 5) | 1 | 26 | (0 – 6) |
| 70 | 4 | 23 | (2 – 6) | 2 | 23 | (0 – 1) | 2 | 20 | (0 – 4.5) |
| 80 | 5 | 15 | (2 – 7) | 3.5 | 12 | (1.25 – 4.75) | 2.5 | 8 | (0 – 7) |
| 90 | 5 | 8 | (5 – 8) | 2 | 7 | (1 – 5) | 1.5 | 4 | (0 – 7.5) |
| 100 | 9 | 7 | (7 – 9) | 2 | 5 | (1 – 4.5) | 2 | 5 | (0.5 – 5.5) |
| 110 | 8.5 | 4 | (8 – 9.75) | 3 | 2 | (3 – 3) | 10 | 1 | (10 – 10) |
Fig 2.
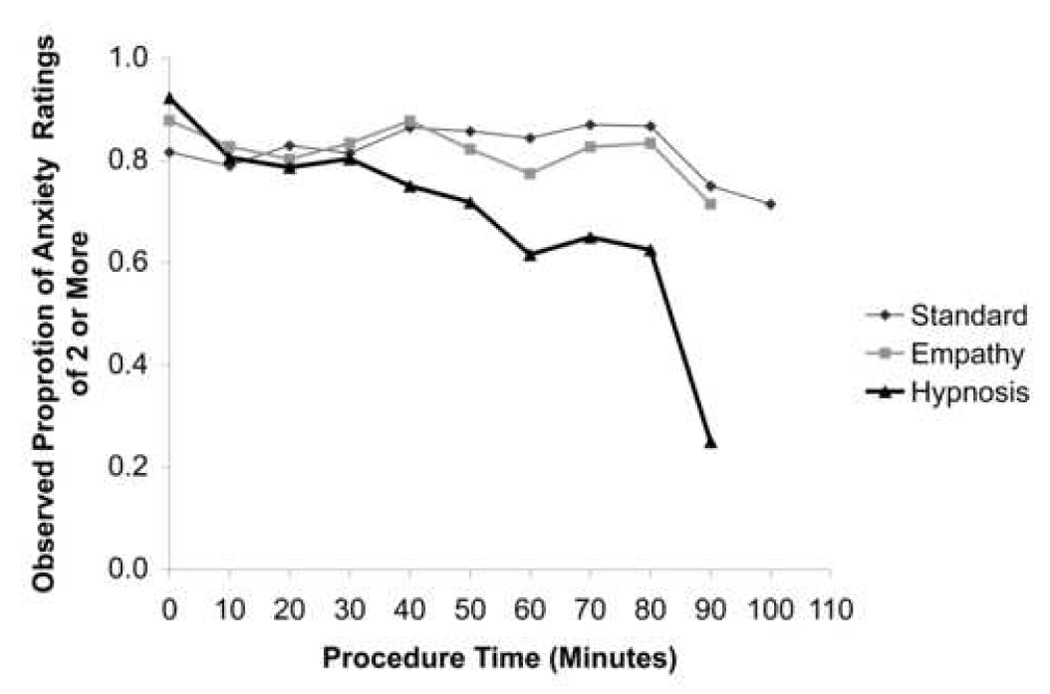
Observed proportion of anxiety responses 2 or above (top graph), 4 or above (middle graph), and 6 or above (bottom graph) over time for the three groups.
Fig. 3.
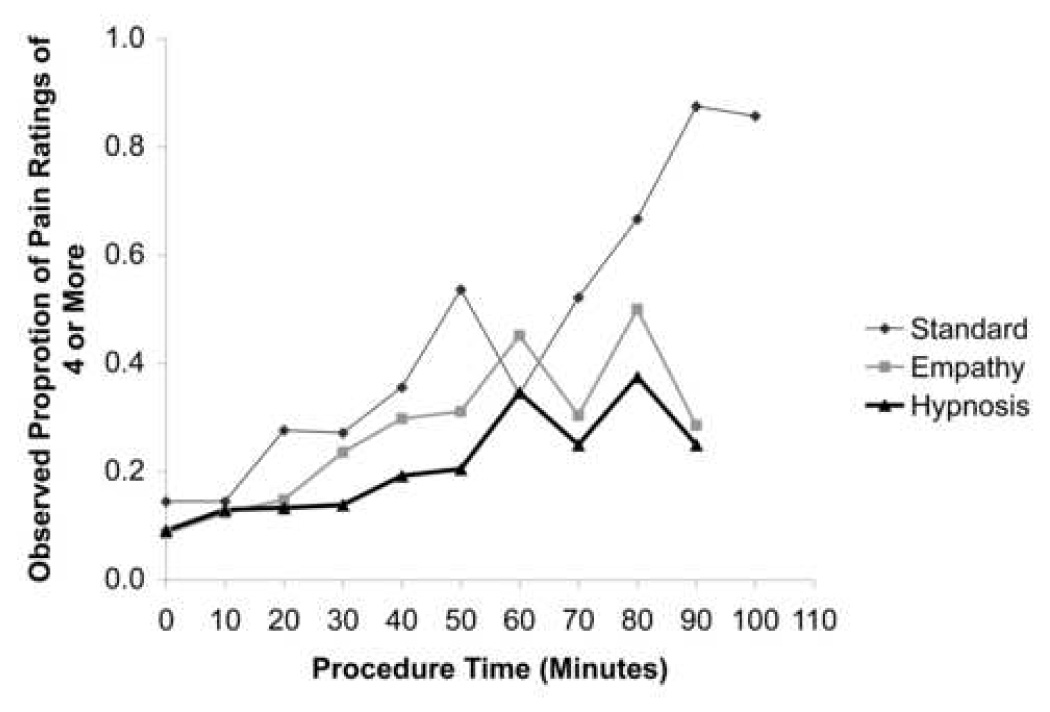
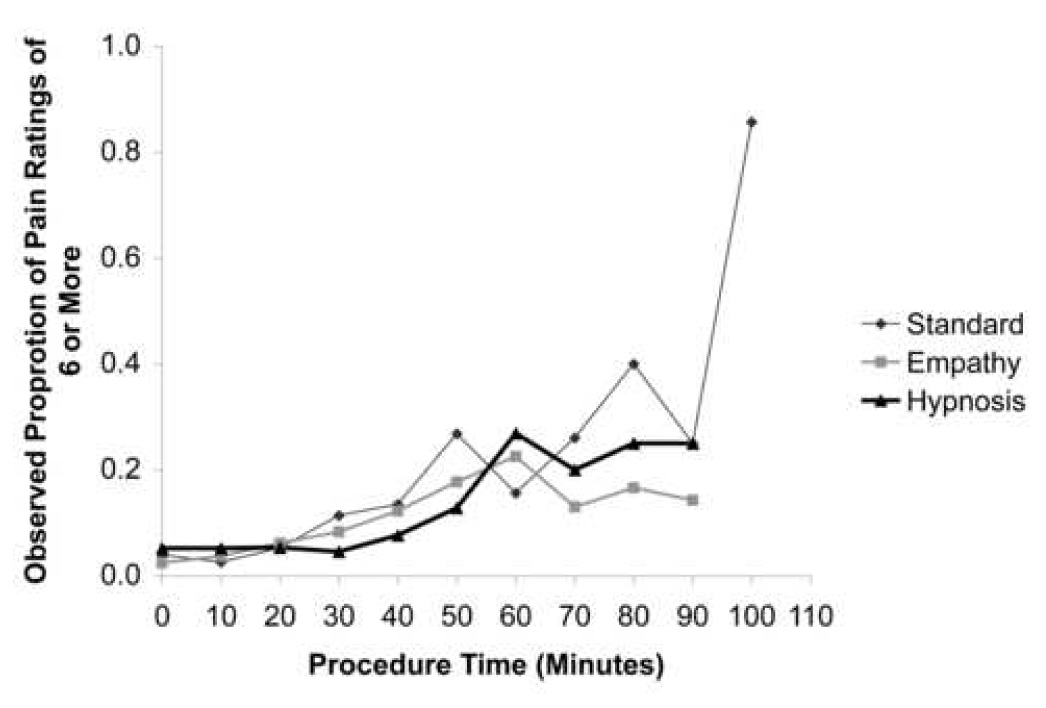
Observed probability of pain responses 2 or above (top graph), 4 or above (middle graph), and 6 or above (bottom graph) for the three groups.
The linear trends for anxiety were positive for Standard care, indicating that patients experience an increase in anxiety during the procedure (standard care slope = 0.18, p < 0.001). The linear trend for Empathy was not different from zero (empathy slope = −0.04, p = 0.45), indicating that patients experienced no change in anxiety. The linear trend for anxiety was negative for Hypnosis, indicating that patients experienced a decrease in anxiety (hypnosis slope = −0.27, p < 0.001). Anxiety increased more with Standard care than Empathy (p < 0.01), and more with Standard care than Hypnosis (p < 0.001). Moreover, anxiety decreased more with Hypnosis than Empathy (p < 0.01).
Pain increased over the procedure in all three groups (Standard slope = 0.53, p < 0.001; Empathy slope = 0.37, p < 0.001; Hypnosis slope = 0.34, p < 0.001). Pain rose more slowly with Empathy than Standard care (p = 0.024), and pain rose more slowly with Hypnosis than Standard care (p = 0.018). There was no evidence that rate of change in pain differed for hypnosis and empathy (p = 0.73).
3.4. Adverse Events
There were 7 adverse events in the Standard group (5 hematomas, one vasovagal and one vomiting episode), 11 in the Empathy group (9 hematomas, 2 vasovagal episodes), and 3 hematomas in the Hypnosis group. Fisher exact tests demonstrated no statistically significant differences in proportions among the groups.
3.5. Room Time and Cost
Medians (and 95% confidence intervals) of back-transformed (exponential (logarithmic)) room times were 46 minutes (41–52 minutes) for Standard care, 43 minutes (38–48 minutes) for Empathy, and 39 minutes (35–45 minutes) for Hypnosis (p = 0.18). Corresponding data for cost were $161 ($140–$186) for Standard care, $163 ($142–$188) for Empathy, and $152 ($133–$174) for Hypnosis (p = 0.74).
4. Discussion
Women in our study entered the biopsy suite with no pain but markedly elevated anxiety anxiety. Pain increased linearly over time in all three groups, but significantly less so with Empathy and Hypnosis treatment. Anxiety increased in the Standard group, did not change in the Empathy group, and decreased in the Hypnosis group. While structured empathic behaviors were associated with a smaller increase in pain and anxiety as compared to standard care, the addition of hypnotic elements produced greater reduction in anxiety. Self-hypnotic relaxation was the more powerful of the interventions tested.
Increase in pain over time under standard care and empathy conditions, and less increase with self-hypnotic relaxation has also been reported for image-guided interventions of the vasculature and kidneys where patients had access to intravenous sedatives and narcotics (Lang et al. 2000). In the current study, patients had lidocaine for local anesthesia but did not have access to intravenous or oral medication before or during the procedure. Hypnotizability was not a prerequisite for patients to be included in either study. Our results are consistent with a meta-analysis that reported 89% of surgical patients benefit from adjunct hypnosis and concluded that most patients have enough “hypnotizability” to benefit clinically (Montgomery et al. 2002).
The women in our study presented with a higher state anxiety (mean STAI 48) than one would expect in a nonpsychiatric female population (normative mean 35) (Spielberger 1983). This is consistent with findings by others who reported STAIs between 45 and 71 prior to breast biopsy (Helbich et al. 1996; Maxwell et al. 2000; Novy et al. 2001; Bugbee et al. 2005). Not surprisingly, 13–29% of women would choose premedication even for less invasive fine needle biopsy (Helbich et al. 1996). Bugbee et al. compared the effects of oral premedication with an anxiolytic and relaxation treatment in a randomized study using a 0–10 self-assessment anxiety scale similar to ours (Bugbee et al. 2005). They found a significant decrease in anxiety from the pre- to intraprocedure level (5.1 to 3.8) in the premedication group, but not in their usual care control and relaxation groups. Their relaxation treatment used music and ocean sound tapes, which – like our empathy group – provides an external focus of attention. Hypnosis, in contrast, relies on an internal focus of attention.
Compared to the longer and more invasive medical procedures reported in the Lancet study The specific characteristics of this patient population and procedure (Lang et al. 2000)., large core breast biopsy is shorter in duration; patients do not tend to have as many associated comorbidities; and anxiety plays a greater role. The challenge for patients is lying prone on the table for the stereotactic biopsies with the breast exiting under the table where the work is done, not visible to the patients with relatively noisy vacuum suctioning equipment and having exposed breast. The fear of receiving a cancer diagnosis adds to the anxiety, while pain is predominantly driven by immobilization on a relatively hard table and breast compression. Pain tends to increase over time on the procedure table, and the ability to detect differences among pain reducing treatments therefore is expected to be smaller with the shorter breast biopsy procedure. These specific characteristics of the breast-biopsy patient population and procedure may texplain why the effect of hypnosis on anxiety was more pronounced than that on pain.
The use of hypnosis did not add room time. The sample size in this study was not great enough to show a significant difference in time required for standard care (46 minutes) and hypnosis (39 minutes). This may also be based on the relatively short LCNB procedure; studies involving lengthier vascular and renal procedures showed significant time savings with hypnosis as compared to standard care (61 vs. 78 min) (Lang et al. 2000).
Within our local cost structure, the addition of a hypnosis professional did not add cost ($151 with hypnosis vs. $162 under standard of care). If a higher paid nurse/senior technologist would have been added to provide the hypnosis an additional $13 per case (differential between the prorated salary of the research assistant and nurse/senior technologist) might be added. Alternatively, if – as has been shown for other procedures (Lang and Berbaum 1997) – an appropriately trained, already present member of the clinical team structures the hypnotic intervention the average cost for hypnosis could theoretically be reduced by $14.50. These assessments do not include the cost of amortization of training, obtainable for about $350–$500 per person from a professional hypnosis society or at local cost during in house training from available suitable trainers on staff.
A limitation of this study was the impossibility to blind the clinical team and those recording outcome data to the intervention. Space in breast biopsy suites is sparse and expensive (Raza et al. 2001). The attending physician, fellow, technologist, research assistant/therapist, and occasional resident already crowded the space around the patient. The physicians and technologists needed to remain able to circulate and communicate with the patient even when the research assistant provided a behavioral intervention, and the research assistant needed to see stimulating events. Adding an uninvolved blinded observer to collect pain and anxiety data would have required this extra person to enter and leave the room repeatedly during the breast biopsy and was judged disruptive for this procedure requiring privacy and millimeter accuracy of targeting. One cannot exclude that data collection by the research assistant/therapist might have induced some patients to give lower pain and anxiety ratings in order to please. This, however, would not explain the significantly lower anxiety ratings under hypnosis.
It is difficult to assess how the outcome of the study might have been if we could have employed established experts in hypnosis and used instead of a standardized script a patient-tailored induction which is considered to be superior by authorities in the field (Barabasz and Christensen, 2006). The rigor of a prospective randomized clinical trial however demanded a highly reproducible approach that could be exported into practice settings in which highly specialized hypnosis personnel may not always be available.
Whether self-hypnotic relaxation provides more or less anxiety relief than premedication with anxiolytics is unknown. Some may question the need for a behavioral approach when there is cheap and effective oral medication. While this might be true for the providers of care, the patients incur cost: they are legally not allowed to drive, have to find a responsible adult to accompany them, and cannot engage in work involving machinery or possible liability for 24hrs. Self-hypnotic relaxation offers patients during large core needle breast biopsy a drug-free choice for reducing pain and anxiety without adding procedure time, cost or side-effects. This may have implications for the conduct of other outpatient procedures that have access to lidocaine only for pain management.
Acknowledgements
This work was supported by the US Army Medical Research and Materiel Command DAMD17-01-01 and the National Institutes of Health, National Center for Complementary and Alternative Medicine 1K24 AT 01074 and RO1-AT-0002-07. The funding agencies were not involved in the design and conduct of the study, data analysis, and approval of the manuscript. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the funding agencies.
We greatly appreciate the invaluable help in the study design and consultation of Susan Lutgendorf, PhD and Henrietta Logan, PhD and expert technical assistance during patient enrollment and data analysis received throughout the course of the study of Gloria Salazar, MD , Verena Stinshoff, B.S., Christine Schupp, B.S., Tony Wong, B.S., and technical excellence of Brad Anderson, B.A. in data processing, and analysis; and the staff of the mammography team. Our greatest gratitude goes to the women who participated in this study.
Appendix Script
"We want you to help us to help you to learn a concentration exercise to help you get through the procedure more comfortably. It can be a way to help your body be more comfortable through the procedure and also deal with any discomfort that may come up during the procedure. It is just a form of concentration, like getting so caught up in a movie or a good book that you forget you are watching a movie or reading a book.
Now what I want to do is to show you how you can use your imagination to enter a state of focused attention and physical relaxation. If you hear sounds or noises in the room, just use these to deepen your experience. And use only the suggestions that are helpful for you. There are a lot of ways to relax but here is one simple way:
On one, I want you to do one thing - look up.
On two, do two things, slowly close your eyes and take a deep breath.
On three, do three things, breath out, relax your eyes, and let your body float.
That's good, just imagine your whole body floating, floating through the table, each breath deeper and easier. Right now I want you to imagine that you are floating somewhere safe and comfortable, in a bath, a lake, a hot tub, or just floating in space, each breath deeper and easier. Notice how with each breath you let a little more tension out of your body as you let your whole body float, safe and comfortable, each breath deeper and easier. Good, now with your eyes closed and remaining in this state of concentration please describe for me how your body is feeling right now. Where do you imagine yourself being, what is it like? Can you smell the air? Can you see what is around you? Good, now this is your safe and pleasant place to be and you can use it in a sense to play a trick on the doctors. Your body has to be here, but you don't. So just spend your time being somewhere you would rather be.
Now, if there is some discomfort, and there may be some with the procedure as they prepare you and insert the line, or as you feel the dye entering your body, there is no point in fighting it. You can admit it, but then transform that sensation. If you feel some discomfort, you might find it helpful to make that part of your body to feel warmer, as if you were in a bath. Or cooler, if that is more comfortable, as if you had ice or snow on that part of your body. This warmth and coolness becomes a protective filter between you and the pain.
If you have any discomfort right now imagine that you are applying a hot pack or you are putting snow or ice on it and see what it feels like. Develop the sense of warm or cool tingling numbness to filter the hurt out of the pain.
With each breath, breathe deeper and easier, your body is floating, filter the hurt out of the pain.
Now again with your eyes closed and remaining in the state of concentration, describe what your are feeling right now.
(1) If they are at their safe and comfortable place - reinforce it.
What is it like now? What do you see around you? What are you doing?
(2) If they are in pain -
The pain is there but see if you can add coolness, more warmth, or make it lighter or heavier
If no longer in pain: Good continue focus on those sensations
If still in pain: Try to focus on sensations in another p[art of your body. Now rub your fingertips together and notice all of the delicate sensations in your fingertips and see how much you can observe about what it feels like to rub your thumb and forefingers together. how do you feel now ?
If not in pain - Good continue to focus on these sensations
If still in pain - Now imagine yourself being at ________ (patient's safe place) where you said you felt relaxed and comfortable. What is it like now? What is the temperature? What do you see around you?
(3) If they state that they are worried - Okay, your main job right now is to help your body feel comfortable so we will talk about what is worrying you. But first no matter what we discuss concentrate on your body floating. So let's get the floating back into your body. Imagine that you are in this favorite spot and when you are ready let me know by nodding your head and then we will talk about what is worrying you. But remember no matter what we discuss concentrate on your body floating, and feel safe and comfortable. So what is worrying you? (Discuss)
How do you feel now? If not worried: Good, now continue to concentrate on body floating, and feel safe and comfortable in your favorite place.
If after discussing patient has persistent worry, then - Okay picture in your mind a screen like a movie screen, TV screen or a piece of clear blue sky. First picture a pleasant scene on it. Now picture a large piece of blue screen divided in half. All right, now on the left half, picture what you are worrying about on the screen. Now on the right half, picture what you will do about it, or what you would recommend someone else to do about it. Keep your body floating, and if you are worrying about the outcome, okay admit it to yourself, but your body does not have to get uptight about it. You may, but your body does not have to.
Good, you know that whatever happens there is always something you can do. But for now just concentrate on keeping your body floating and feeling safe and comfortable.
Sometimes throughout the procedure say - If you feel any sense of discomfort you are welcome to let me know about it. Try to use the filter to filter the hurt out of the pain, but by all means let me know and I will do what I can to help you with it as well. Whatever you do just keep your body floating and concentrate on being in the place where you feel safe and comfortable.
When finished, say - Okay the procedure is over now. We are going to leave formally this state of concentration by counting backwards from three to one. On three get ready, on two with your eyes closed roll up your eyes, and on one let your eyes open and take a deep breath and let it out. That will be the end of the formal exercise, but when you come out of it you will still have the feeling of comfort that you felt during it. Ready, three, two, one.
If necessary: Three - get ready. two with your eyes closed roll up your eyes. One - let your eyes open and take a deep breath.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acute Pain Management Guideline Panel. Clinical practice guideline. AHCPR Pub. No.92-0032. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services; 1992. Acute pain management: operative or medical procedures and trauma. [Google Scholar]
- American Cancer Society. Breast cancer facts & figures 2005–2006. Atlanta: American Cancer Society Inc; 2005. [Google Scholar]
- American College of Radiology. ACR practice guidelines for the performance of stereotactically guided breast interventional procdures. Reston, VA: ACR; 2000. [Google Scholar]
- Barabasz A, Christensen C. Age regression: Tailored versus scripted inductions. Am J Clin Hypn. 1006;48:251–261. doi: 10.1080/00029157.2006.10401532. [DOI] [PubMed] [Google Scholar]
- Benotsch E, Lutgendorf SK, Watson DW, Fick LJ, Lang EV. Rapid anxiety assessment in medical patients: evidence for the validity of verbal anxiety ratings. Ann Behav Med. 2000;22:199–203. doi: 10.1007/BF02895114. [DOI] [PubMed] [Google Scholar]
- Bugbee ME, Wellisch DK, Arnott IM, Maxwell JR, Kirsch DL, Sayre JW, Bassett LW. Breast core-needle biopsy clinical trial of relaxation technique versus medication versus no intervention for anxiety reduction. Radiology. 2005;234:73–78. doi: 10.1148/radiol.2341030163. [DOI] [PubMed] [Google Scholar]
- Caruso A, Efficace F, Parrila A, Angelone L, Ferranti F, Grandinetti M. Pain and anxiety related to mammography in breast cancer patients. Radiol Med. 2001;102:335–339. [PubMed] [Google Scholar]
- Centers of Disease Control and Prevention (CDC) Behavioral risk factor surveillance system survey data. Atlanta, Georgia: Department of Health and Human Services, Centers for Disease Control and Prevention; 2002. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. "Mini-Mental State": A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Groenewoud JH, Pijnappel RM, van den Akker-Van Marle ME, et al. Cost-effectiveness of stereotactic large-core needle biopsy for nonpalpable breast lesions compared to open breast biopsy. Br J Cancer. 2004;90:383–392. doi: 10.1038/sj.bjc.6601520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helbich TH, Dantendorfer K, Mostbeck GH, Schick S, Wunderbaldinger P, Amering M, Alexandrowicz R, Wolf G. Randomized comparison of sitting and prone positions for stereotactic fine-needle aspiration breast biopsy. Br J Surg. 1996;83:1252–1255. [PubMed] [Google Scholar]
- Jennrich RI, Schluchter MD. Unbalanced repeated measures models with structured covariance matrices. [PubMed] [Google Scholar]
- Kirk RE. Experimental design: procedures for the behavioral sciences. 3rd ed. Pacific Grove, CA: Brooks/Cole Publishing Company; 1995. [Google Scholar]
- Laird NM, Ware JH. Random effects model for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- Lang EV, Benotsch EG, Fick LJ, Lutgendorf S, Berbaum ML, Berbaum KS, Logan H, Spiegel D. Adjunctive non-pharmacologic analgesia for invasive medical procedures: a randomized trial. Lancet. 2000;355:1486–1490. doi: 10.1016/S0140-6736(00)02162-0. [DOI] [PubMed] [Google Scholar]
- Lang EV, Berbaum KS. Educating interventional radiology personnel in nonpharmacologic analgesia: effect on patients' pain perception. Acad Radiol. 1997;4:753–757. doi: 10.1016/s1076-6332(97)80079-7. [DOI] [PubMed] [Google Scholar]
- Lang EV, Laser E, Anderson B, Potter J, Hatsiopoulou O, Lutgendorf SK, Logan H. Shaping the experience of behavior: Construct of an electronic teaching module in nonpharmacologic analgesia and anxiolysis. Acad Radiol. 2002;9:1185–1193. doi: 10.1016/s1076-6332(03)80520-2. [DOI] [PubMed] [Google Scholar]
- Lang EV, Lutgendorf S, Logan H, Benotsch E, Laser E, Spiegel D. Nonpharmacologic analgesia and anxiolysis for interventional radiological procedures. Sem Intervent Radiol. 1999;16:113–123. [Google Scholar]
- Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- Maxwell JR, Bugbee ME, Wellisch DK, Shalom A, Sayre J, Bassett LW. Image-guided core needle biopsy of the breast: Study of psychological outcomes. Breast J. 2000;6:53–61. doi: 10.1046/j.1524-4741.2000.98079.x. [DOI] [PubMed] [Google Scholar]
- Meyer JE, Smith DN, Lester SC, Kaelin C, DiPiro PJ, Denison CM, Christian RL, Harvey SC, Selland DL, Durfee sM. Large-core breast needle biopsy of nonpalpable breast lesions. JAMA. 1999;281:1638–1641. doi: 10.1001/jama.281.17.1638. [DOI] [PubMed] [Google Scholar]
- Moncher FJ, Prinz RJ. Treatment fidelity in outcome studies. Clin Psychol Rev. 1991;11:247–266. [Google Scholar]
- Montgomery GH, David D, Winkel G, Silverstein JH, Bovberg DH. The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesth Analg. 2002;94:1639–1645. doi: 10.1097/00000539-200206000-00052. [DOI] [PubMed] [Google Scholar]
- Murphy D, McDonald A, Power A, Unwin A, MacSullivan R. Measurement of pain: A comparison of the visual analogue with a nonvisual analogue scale. J Clin Pain. 1988;3:197–199. [Google Scholar]
- National Institutes of Health. The integrated approach to the management of pain. J Pain Symptom Management. 1987;2:35–44. [PubMed] [Google Scholar]
- Novy DM, Price M, Huynh PT, Schuetz A. Percutaneous core biopsy of the breast. Acad Radiol. 2001;8:467–472. doi: 10.1016/S1076-6332(03)80617-7. [DOI] [PubMed] [Google Scholar]
- Paice JA, Cohen FL. Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs. 1997;20:88–93. doi: 10.1097/00002820-199704000-00002. [DOI] [PubMed] [Google Scholar]
- Raza S, Rosen MP, Chorny K, Mehta TS, Hulka CA, Baum JK. Patient expectations and costs of immediate reporting of screening mammography: Talk isn't cheap. AJR. 2001;177:579–583. doi: 10.2214/ajr.177.3.1770579. [DOI] [PubMed] [Google Scholar]
- Sachs D, McClenny T, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Intervent Radiol. 2003;14:S199–S202. doi: 10.1097/01.rvi.0000094584.83406.3e. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS/STAT user's guide, Version 8. Cary, NC: SAS Institute Inc; 1999. [Google Scholar]
- Spielberger C. Manual for the state-trait anxiety inventory STAI (form Y) Palo Alto: Consulting Psychologists; 1983. [Google Scholar]
- Spitzer RL, Endicott J. Schedule for Affective Disorders and Schizophrenia. 3rd. edition. 1979. [DOI] [PubMed] [Google Scholar]
- Tabar L, Yen MF, Vitak B, Tony Chen HH, Smith RA, Duffy SW. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361:1405–1410. doi: 10.1016/S0140-6736(03)13143-1. [DOI] [PubMed] [Google Scholar]
- van Vlymen JM, Sa Rego MM, White PF. Benzodiazepine premedication: Can it improve outcome in patients undergoing breast biopsy procedures? Anesthesiology. 1999;90:740–747. doi: 10.1097/00000542-199903000-00016. [DOI] [PubMed] [Google Scholar]


