Abstract
Purpose
Circular external fixators have several advantages over other surgical options in the treatment of limb length discrepancy and axial deformity. The innovative Taylor Spatial Frame (TSF) combines a rigid hexapod fixation system with the support of a web-based software program, and thus offers the possibility of simultaneous corrections of multidirectional deformities. Whilst there is still some scepticism of many Ilizarov device users about the advantages of the TSF, the purpose of the study was to perform a comparison between the TSF and the Ilizarov ring fixator (IRF) with regard to the accuracy of deformity correction in the lower limb.
Methods
Two hundred and eight consecutive deformity corrections in 155 patients were retrospectively evaluated. There were 79 cases treated with the IRF and 129 cases treated with the TSF. The mean age of the patients at the time of surgery was 13.2 years (range; 2–49 years). Standing anteroposterior and lateral radiographs were evaluated preoperatively and immediately after removal of the frames. The final result was compared to the preoperatively defined aim of the deformity correction. According to the treated count of dimensions, we differentiated four types of deformity corrections. The results were graded into four groups based on the persisting axial deviation after removal of the frame.
Results
The aim of the deformity correction was achieved in a total of 90.7% in the TSF group, compared to 55.7% in the IRF group. On the basis of the count of dimensions, the TSF achieved obviously higher percentages of excellent results (one dimension: TSF 100%; IRF 79.3%; two dimensions: TSF 91.8%; IRF 48.6%; three dimensions: TSF 91.1%; IRF 28.6%; four dimensions: TSF 66.7%; IRF 0%). In addition, the degree of the persisting deformity increased with the number of planes of the deformity correction.
Conclusions
The TSF allowed for much higher precision in deformity correction compared to the IRF. In two-, three- and four-dimensional deformity corrections in particular, the TSF showed clear advantages. This may derive from the TSF-specific combination of a hexapod fixator with the support of an Internet-based software program, enabling precise simultaneous multiplanar deformity corrections.
Keywords: Deformity correction, Comparison, Accuracy, Taylor Spatial Frame, Ilizarov ring fixator
Introduction
Current methods of limb lengthening are based on gradual distraction osteogenesis [1–4].
The Ilizarov ring fixator (IRF) is thought to have several advantages over other surgical options in the treatment of limb length discrepancy and axial deformity [5], and has become widely accepted for the correction of various deformities of the upper and lower limb. For correction, the surgeon uses hinges and translation mechanisms to build a custom-made frame system for each distinct deformity [6]. During treatment, correction of complex deformities may require changes of the frame construct, which may be very time-consuming or even impossible [7, 8].
As a hexapod fixator with lengthening struts in oblique positions, the Taylor Spatial Frame (TSF) (Smith & Nephew, Memphis, TN, USA) offers the possibility of simultaneous correction of multidirectional deformities without the need of extensive changes to the system during correction [7–12]. Thus, in comparison to the traditional IRF the TSF uses one single frame construct, and no additional devices are needed for correction of translation or rotation deformities. With the prerequisite of accurate initial assessment of the mounting parameters and proper and stable implantation of the circular hexapod fixator, deformity correction is easily performed by using the Total residual web-based program [7, 10]. The software-generated frame adjustments schedule allows an accurate overview of the course of the deformity correction for the surgeon and the patient (Fig. 1).
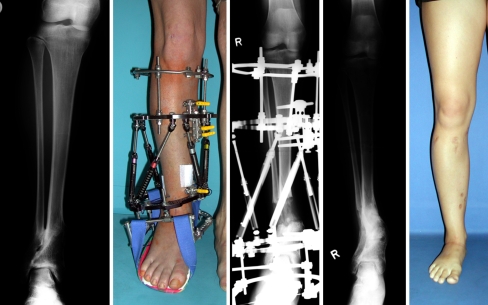
Fig. 1.
Treatment of a posttraumatic multidimensional deformity with the Taylor Spatial Frame (TSF). Deformity correction included lengthening, correction of varus malalignment and translational deformity
Since there is still vivid discussion amongst the users of external devices about the benefit of the TSF in complex deformity correction, the purpose of the present study was to investigate the accuracy of deformity correction achieved in the lower limb in a comparison between the TSF and the IRF.
Patients and methods
We reviewed a total of 278 lower-limb deformity corrections in 207 patients performed with either the IRF or the TSF between January 1, 1985 and December 31, 2004.
The inclusion criterion for the current study was the use of the IRF or the TSF for any gradual deformity correction in the lower limb.
Cases with incomplete medical reports and X-ray documentation were excluded, due to lacking information about the aim of the deformity correction and inaccurate radiological documentation before or after the deformity correction.
Any cases with acute intraoperative corrections of the deformity were excluded, because the study solely aimed at investigating the accuracy of gradual deformity correction. Cases with any major complications that obviated an uncomplicated distraction progress were also excluded from the current study as long as they were not directly fixator-related. Bi-level corrections were also excluded from the study, whilst possible interference between the two different deformity corrections in the combined frame constructs was observed.
After application of the exclusion criteria, we included 208 gradual deformity corrections in 155 patients in this study.
All patients provided informed consent to participate in the study, and the study was approved by an institutional review board.
The conventional IRF (Smith-Nephew-Richards, Memphis, TN, USA) was used in 79 cases, and the TSF (Smith & Nephew) was used in 129 cases. There were 72 female and 83 male patients. The mean age of the patients at the time of implantation of the ring fixators was 13.2 years (range; 2–49 years).
Femoral corrections were performed in 58 cases; tibial corrections were performed in 150 cases. In the majority of the cases, a singular correction of one segment was performed (53.9%). In this group of patients, there were 33 femoral corrections and 79 tibial corrections.
Diagnosis in the majority of the cases was congenital deficiency (n = 85), followed by acquired posttraumatic or postinfectious deformities (n = 44), idiopathic deformities (n = 26) and miscellaneous other deformities (n = 53) (Table 1). Idiopathic deformity was defined as any frontal, coronal or axial (rotational) deformity without any underlying congenital, acquired or posttraumatic cause.
Table 1.
Diagnosis of all 208 cases included in the study
| Diagnosis | n |
|---|---|
| Congenital deficiency | |
| Fibular hemimelia | 54 |
| Congenital femoral deficiency | 29 |
| Tibial aplasia | 2 |
| Acquired deformity | |
| Posttraumatic | 33 |
| Postinfectious | 11 |
| Idiopathic deformity | 26 |
| Hypo-, Pseudo-, Achondroplasia | 16 |
| Rickets | 9 |
| Syndromes | 8 |
| Enchondromatosis | 4 |
| Blount’s disease | 5 |
| Mucopolysacharidosis | 4 |
| Myelomeningocele | 2 |
| Peromelia | 2 |
| Multiple hereditary exostoses | 1 |
| Amniotic disease | 1 |
| Hemihypertrophy | 1 |
| All | 208 |
Medical records and radiographs were retrospectively analyzed with regard to demographic data, course of treatment, complications and radiographic data. All radiographs were made using the same technique, distance and machine. For preoperative deformity analysis and evaluation of the final result, we used anteroposterior long leg standing X-rays and lateral views of the deformed segments. Deformity analysis was performed according to Paley et al. [13]. In cases with leg length discrepancy, orthoradiography and standing anteroposterior–pelvis radiographs were taken to determine the true discrepancy of each segment. In cases with rotational malalignment, CT-scan was used to determine the deformity. All measurements were undertaken by the first and second author at the same time. CT-scans were measured by the radiologist and the first author.
For evaluation of the achieved result, we compared the final result with the initial aim of the deformity correction and lengthening. In cases where a normal alignment of the segment was the aim of the correction, any deviations from the physiological values [13] were described as persistent axial deformity after removal of the frame. In cases where the aim of the correction was outside the physiological range (i.e., intended over- or undercorrection) the final result of the correction was compared to the preoperative aim, with any deviation described as a persistent deformity.
Intraoperatively, prior to osteotomy, the preassembled fixator was placed on the segment, with reference to the knee joint in distal femoral and proximal tibial corrections and to the ankle joint line in distal tibial corrections. A standard hybrid bone-fixation technique with screws and k-wires was used in all cases. The majority of the osteotomies were performed percutaneously, as previously described by De Bastiani [1].
Specification of the type of the deformity correction
All cases included some leg lengthening. There were no cases of axial corrections without any lengthening procedure. The lengthening procedures in cases with major axial deformities were performed to allow a gradual correction of the deformity without impingement of the segments.
For a clear harmonization of all deformity corrections four types were specified:
Type I (one-dimensional deformity correction 1D) included all cases with leg lengthening procedure only, without any other axial deformity correction.
Type II (two-dimensional deformity correction 2D) included all cases with leg lengthening procedure and additional axial deformity correction in one plane (frontal, sagittal, rotational).
Type III (three-dimensional deformity correction 3D) included all cases with leg lengthening procedure and additional axial deformity correction in two planes (frontal, sagittal, rotational).
Type IV (four-dimensional deformity correction 4D) included all cases with leg lengthening procedure and additional axial deformity correction in three planes (frontal, sagittal, rotational).
Persisting deformity after removal of the frame
Our study concept aimed at exclusively investigating the fixator-related accuracy during deformity correction by excluding secondary influences after frame removal. Thus, for evaluation of the accuracy of the deformity correction the results of the corrections were graded in four groups immediately after removal of the frame:
Group I contains all cases without any persisting axial deformity after correction.
Group II contains all cases with a minor persistent deformity ≤5°.
Group III contains all cases with a moderate persistent deformity of 6–10°.
Group IV contains all cases of a severe persistent deformity >0°.
The software SPSS for Windows Release 10 (SPSS Inc, Chicago, IL, USA) was used for all statistical calculations. Each variable was tested for normal distribution using the Kolmogorov–Smirnov test. If there was a normal distribution we used the Student’s t-test with a 95% confidence interval (CI) for significance testing. We used the Wilcoxon signed rank test to evaluate variables that did not show normal distribution. Significance was set at the P < 0.05 level.
Results
Preoperatively defined aim of the deformity correction (Table 2)
Table 2.
Preoperatively defined aim of deformity correction in the IRF- and TSF-group
| Aim of correction | IRF | TSF | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | Range | n | Mean | SD | Range | |
| Lengthening | 79 | 4.9 | 2.3 | 0–10 | 129 | 2.7 | 1.9 | 0–7,8 |
| Frontal plane | 43 | 14.5° | 10.9 | 2°–53° | 108 | 11.3° | 7.9 | 2°–48° |
| Sagittal plane | 21 | 24.5° | 14.6 | 4°–50° | 23 | 13.4° | 6.2 | 5°–28° |
| Rotational plane | 2 | 15.0° | 7.1 | 10°–20° | 47 | 16.4° | 7.8 | 6°–40° |
Leg lengthening (LL) was measured in centimeter and axial deviation was measured in degrees
In 43 of 208 cases (IRF; n = 29, TSF; n = 14) the aim of the deformity correction was leg lengthening alone without any additional axial deformity. The desired mean leg lengthening was significantly (P < 0.05) larger in the IRF- than in the TSF-group. The desired frontal and sagittal plane correction was also significantly (P < 0.05) larger in the IRF- than in the TSF-group. Even though the average amount of desired rotational correction was higher in the TSF-group, there was no significant difference (P > 0.05) when comparing the two groups. There were only two cases with rotational deformities in the IRF-group, compared to 47 cases in the TSF-group.
Dimensions of gradual deformity correction (Table 3)
Table 3.
Distribution of the dimensions of deformity corrections in the different fixator groups
| Type of deformity correction | IRF | TSF | ||
|---|---|---|---|---|
| n | % | n | % | |
| Type I | 29 | 36.7 | 14 | 10.9 |
| Type II | 35 | 44.3 | 61 | 47.3 |
| Type III | 14 | 17.7 | 45 | 34.9 |
| Type IV | 1 | 1.3 | 9 | 7.0 |
| All | 79 | 100.0 | 129 | 100.0 |
Type I: one-dimensional deformity correction 1D, Type II: two-dimensional deformity correction 2D, Type III: three-dimensional deformity correction 3D, Type IV: four-dimensional deformity correction 4D
Simple axial corrections without any additional leg lengthening were not performed.
Leg lengthening procedures (Type I) were performed in a significantly (P < 0.05) higher percentage in the IRF-group (36.7%) than in the TSF-group (10.9%).
The vast majority of the cases consisted of Type II-deformity corrections, with comparable percentages in the IRF- and the TSF-group (IRF: 44.3%, TSF: 47.3%). In the IRF-group there were 28 cases of frontal plane and seven cases of sagittal plane malalignment corrections in addition to leg lengthening. In the TSF-group there were 57 cases of frontal plane, one case of sagittal plane and three cases of rotational malalignment corrections in addition to leg lengthening.
In the group of Type III-deformity corrections, a significantly (P < 0.05) higher percentage of cases was treated with the TSF (34.9%) than with the IRF (17.7%). In the IRF-group there were 13 cases of combined frontal-sagittal plane and one case of frontal-rotational plane malalignment corrections in addition to leg lengthening. In the TSF-group there were ten cases of frontal-sagittal plane, 32 cases of frontal-rotational plane and three cases of sagittal-rotational malalignment corrections in addition to leg lengthening.
In the group of Type IV-deformity corrections, there was again a significantly (P < 0.05) higher percentage of the cases treated with the TSF (7.0%) than with the IRF (1.3%). In the TSF-group there were nine cases of frontal-sagittal-rotational plane malalignment corrections in addition to leg lengthening. In the IRF-group there was one such case.
Persistent axial deformity in the IRF- and TSF-group (Table 4)
Table 4.
Persisting axial deformity after frame removal in connection with the dimensionality of deformity correction
| Deformity | 1D | 2D | 3D | 4D | All | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |
| IRF | ||||||||||
| 0° | 23 | 79.3 | 17 | 48.6 | 4 | 28.6 | 0 | 0.0 | 44 | 55.7 |
| ≤5° | 3 | 10.3 | 7 | 20.0 | 1 | 7.1 | 0 | 0.0 | 11 | 13.9 |
| 6°–10° | 3 | 10.3 | 6 | 17.1 | 6 | 42.9 | 1 | 100.0 | 16 | 20.3 |
| >10° | 0 | 0.0 | 5 | 14.3 | 3 | 21.4 | 0 | 0.0 | 8 | 10.1 |
| Average | 6 | 6.0° | 18 | 7.7° | 10 | 13.1° | 1 | 8.0° | 35 | 44.3 |
| TSF | ||||||||||
| 0° | 14 | 100.0 | 56 | 91.8 | 41 | 91.1 | 6 | 66.7 | 117 | 90.7 |
| ≤5° | 0 | 0.0 | 3 | 4.9 | 2 | 4.4 | 2 | 22.2 | 7 | 5.4 |
| 6°–10° | 0 | 0.0 | 0 | 0.0 | 1 | 2.2 | 0 | 0.0 | 1 | 0.8 |
| >10° | 0 | 0.0 | 2 | 3.3 | 1 | 2.2 | 1 | 11.1 | 4 | 3.1 |
| Average | 0 | 0° | 5 | 8.8° | 4 | 6.8° | 3 | 9.7° | 12 | 9.3 |
Type I: one-dimensional deformity correction 1D, Type II: two-dimensional deformity correction 2D, Type III: three-dimensional deformity correction 3D, Type IV: four-dimensional deformity correction 4D
Of the 79 cases treated with the IRF, the aim of the deformity correction was achieved in a total of 44 cases (55.7%). In the remaining 35 (44.3%) cases, a persisting axial deformity was evident in the final radiographs after removal of the device.
A minor deformity (≤5°) was evident in 11 cases (13.9%), a moderate deformity (6°–10°) was evident in 16 cases (20.3%) and a severe persisting deformity (>10°) was found in eight cases (10.1%).
Of the 129 cases treated with the TSF device, the aim of the deformity correction was achieved in 117 cases (90.7%). In the remaining 12 (9.3%) cases, a persisting axial deformity was measured in the final radiographs after removal of the device.
A minor deformity (≤5°) was evident in seven cases (5.4%), a moderate deformity (6°–10°) was evident in one case (0.8 %) and a severe persisting deformity (>10°) was found in four cases (3.1%).
Persisting axial deformity in connection with the dimensionality of the deformity correction (Table 4)
The results in both the IRF-group and in the TSF-group showed interdependency with the type of the dimension of the axial correction. With rising dimensions of axial corrections, there was an increasing percentage of cases with persisting axial deformities.
The aim of the treatment in Type I-deformity corrections was achieved in 79% of cases in the IRF-group, whilst it was achieved in all cases in the TSF-group (P < 0.05). During lengthening, an additional deformity developed in the IRF-group in six cases, with a mean persisting deformity of 6°.
The aim of the treatment in Type II-deformity corrections was achieved in 48.6% of cases in the IRF-group compared to 91.8% in the TSF-group (P < 0.05). There was no significant (P < 0.05) average remaining deformity in the TSF-group (8.8°) compared to the IRF-group (7.7°).
The aim of the treatment in Type III-deformity corrections was achieved in 28.6% of cases in the IRF-group compared to 91.1% in the TSF-group. The average remaining deformity was significantly higher (P < 0.05) in the IRF-group (13.1°) compared to the TSF-group (6.8°).
The aim of the treatment in Type IV-deformity corrections was not achieved in the single case in the IRF-group but in 66.7% in the TSF-group, with a remaining deformity of 8.0° in the IRF-group and 9.7° on average in the TSF-group.
Discussion
The study concept aimed to investigate the accuracy of deformity corrections performed either with the IRF or the TSF.
The main striking finding of the study was that the TSF allowed for much higher precision in deformity corrections compared to the IRF. In multidimensional deformity corrections in particular, the TSF showed clear advantages compared to the IRF. Whilst the IRF showed increasingly inaccurate results in two-, three-, and four-dimensional deformity corrections, the TSF still allowed for excellent results in these cases in a high percentage of cases.
In particular, multidimensional deformity corrections performed with the IRF deserve an experienced Ilizarov surgeon, but even then complex deformities may limit the exact use of the IRF and its hinge system. The surgeons who performed the corrections in this study are all well trained in both the Ilizarov and the TSF procedure, although the devices were not implanted in the same period of time. Whilst the IRF was used mainly from 1985 to 1998, the TSF was used from the beginning of 1999 to 2004. Thus the IRF may have been disadvantaged because of the learning curve with external fixation in the beginning, whilst the TSF may have allowed for good results from the start because of pre-existing larger experience with external fixation and deformity correction. Very few of the cases in the IRF group were treated prior to the published introduction of the Paley criteria [13]. These cases were mainly simple leg lengthening procedures, which to our knowledge did not deteriorate the outcome of this study.
Nevertheless, the results obtained with the TSF were not satisfactory in all cases. This may be related to a learning curve in the beginning of the use of the TSF, and especially to the correct definition of the origin and the handling of the computer software.
To our knowledge, a comparison between deformity corrections performed with the IRF and the TSF has not yet been reported. Nevertheless, the results of corrections performed with both devices, the IRF and the TSF, have been reported as favourable in many previous studies [5–11, 14–18]. As with us, most of the previous authors used the system of Paley et al. [13] for evaluation of the deformities, and graded their results according to the obtained physiological angles in the lower limb. We found it difficult to include cases with intended over- or undercorrections in these outcome measurements, and therefore compared the final result of the correction with the preoperatively defined aim of the correction. Additionally, we found it hard to compare and to summarize the myriad of the performed deformity corrections in multidirectional deformities. Therefore—and with the intention to make the outcome clearer in multidimensional deformity corrections—we graded the cases according to the number of the dimensions which were treated.
Previous reports on the use of the TSF have been on relatively small groups of patients or case series [7–11]. All authors underlined the uncomplicated handling of the TSF, and emphasized the possibility of simultaneous multidimensional deformity correction. In addition, the stable ring fixator supported by the internet-based software was felt to provide accurate and precise deformity corrections in various limb deformities, with several advantages over previously used devices.
Rodl et al. [12] investigated the workspace of a standard IRF construct compared to a standard TSF construct. According to the results of this experimental study, the TSF provides advantages in the correction of rotational and translational deformities, but may be limited by its workspace. Nevertheless, the authors investigated the standard hexapod frame (ring diameter: 155 mm and standard struts) without evaluating the available smaller ring diameters and different strut lengths.
Seide et al. [18] reported on 16 cases treated with the Hexapod Ilizarov Fixator (LITOS), and stressed the easy use of this fixator compared to the IRF when dealing with multidimensional deformity corrections. They found it favourable to use the Hexapod to avoid difficult and time-consuming alterations of the IRF construct, as sometimes necessary when dealing with rotational deformities and secondary deformities during the lengthening procedure.
We believe that the highly favourable results of the TSF in multidimensional deformities depended on the possibility of simultaneous multidimensional deformity corrections, which are enabled by the Internet-based software program in combination with a rigid hexapod construction. Deformity correction with the TSF is based on the Origin-method. The origin is best circumscribed by a so-called virtual hinge. This is the place where the mechanical hinges would be positioned at the site of the CORA (centre of rotation and angulation) when dealing with the IRF. The position of the origin to the reference ring of the TSF may be defined on X-rays intra- or postoperatively and furthermore, if desired, its position may easily be re-defined during deformity correction and inserted into the computer software without changing of the frame construct.
When using the IRF and its hinge system, it may sometimes become difficult or even impossible to place the hinges in the desired position, due to the frame construct itself. Even though the construct of the Ilizarov device theoretically may allow for axial corrections in every possible dimension, treatment of multidimensional deformities may practically only partially be possible and mostly affords a step-by-step treatment of all deformities. This may lengthen the procedure, and is prone to lead to further deformities.
In our opinion, the distinct advantages of the TSF result from the reduced necessity to build a patient-customized frame construct, from its potential for simultaneous multidimensional deformity correction and from the support of a precisely working Internet-based software. Thus, the less complicated correction of multidirectional deformities and the easily performed correction of any residual deformities may lead to an enhanced motivation of the treating medical staff, which then again may lead to favourable results for the TSF.
References
- 1.De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G (1987) Limb lengthening by callus distraction (callotasis). J Pediatr Orthop 7:129–134 [DOI] [PubMed]
- 2.Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissues: part I. Clin Orthop 238:249–281 [PubMed]
- 3.Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissues: part II. Clin Orthop 239:263–285 [PubMed]
- 4.Paley D (1988) Current techniques of limb lengthening (review). J Pediatr Orthop 8(1):73–92 [DOI] [PubMed]
- 5.Cattaneo R, Catagni M, Johnson EE (1992) The treatment of infected nonunions and segmental defects of the tibia by the methods of Ilizarov. Clin Orthop 280:143–152 [PubMed]
- 6.Tetsworth KD, Paley D (1994) Accuracy of correction of complex lower extremity deformities by the Ilizarov method. Clin Orthop 301:102–110 [PubMed]
- 7.Fadel M, Hosny G (2005) The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop 29(2):125–129 (Epub February 10, 2005) [DOI] [PMC free article] [PubMed]
- 8.Sluga M, Pfeiffer M, Kotz R, Nehrer S (2003) Lower limb deformities in children: two-stage correction using the Taylor Spatial Frame. J Pediatr Orthop B 12:123–128 [DOI] [PubMed]
- 9.Feldman DS, Madan SS, Koval KJ, van Bosse HJP, Bazzi J, Lehman WB (2003) Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop 23:387–391 [DOI] [PubMed]
- 10.Feldman DS, Shin SS, Madan SS, Koval KJ (2003) Correction of tibial malunion and non-union with six-axis analysis deformity correction using the Taylor Spatial Frame. J Orthop Trauma 17:549–554 [DOI] [PubMed]
- 11.Rozbruch RS, Helfet DL, Blyakher A (2002) Distraction of hypertrophic non-union of tibia with deformity using Ilizarov/Taylor Spatial Frame: report of two cases. Arch Orthop Trauma Surg 122:295–298 [DOI] [PubMed]
- 12.Rodl R, Leidinger B, Bohm A, Winkelmann W (2003) Correction of deformities with conventional and hexapod frames–comparison of methods (German). Z Orthop Ihre Grenzgeb 141(1):92–98 [DOI] [PubMed]
- 13.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 3:425–465 [PubMed]
- 14.Bell D, Boyer M, Armstrong P (1992) The use of the Ilizarovtechnique in the correction of limb deformities associated with skeletal dysplasia. J Pediatr Orthop 12:283–290 [DOI] [PubMed]
- 15.Shtarker H, Volpin G, Stolero J, Kaushansky A, Samchukov M (2002) Correction of combined angular and rotational deformities by the Ilizarov method. Clin Orthop 402:184–195 [DOI] [PubMed]
- 16.Stanitski DF, Bullard M, Armstrong P, Stanitski CL (1995) Results of femoral lengthening using the Ilizarov technique. J Pediatr Orthop 15:224–231 [PubMed]
- 17.Stanitski DF, Shahcheraghi H, Nicker DA, Armstrong PF (1996) Results of tibial lengthening with the Ilizarov technique. J Pediatr Orthop 16:168–172 [DOI] [PubMed]
- 18.Seide K, Wolter D, Kortmann HR (1999) Fracture reduction and deformity correction with the Hexapod Ilizarov Fixator. Clin Orthop 363:186–195 [PubMed]