Abstract
Purpose
The aim of the study was to find out whether or not there is consensus among experienced pediatric orthopaedists about the management of certain clinical scenarios in Legg-Calvé-Perthes’ disease.
Methods
A questionnaire was sent to all 297 members of the European Paediatric Orthopaedic Society (EPOS) describing four cases of Legg-Calvé-Perthes’ disease (LCPD) with two X-rays each and a short description of the clinical scenario. Two of the patients were younger and two were older than six years of age. From both age groups there was one with a good range of motion and an X-ray classified as Herring A or B, while the other patient had a poor range of motion and an X-ray classified as Herring C. EPO members were asked to choose from various treatment options or to describe any other therapy that they would advise in the clinical scenarios.
Results
One-hundred and fifty members answered the questionnaire. The participants had an average of 20 years of experience in pediatric orthopaedics. There was a consensus that no surgery should be performed in a young patient with a good range of motion and that there should be no weight relief when older with a good range of motion. Conservative containment treatment (abduction splint, Petrie cast) and arthrodiastasis was suggested in only very few centres. There was a tendency to perform
an operation when the patient is older with a poor range of motion and to perform operative treatment only when there were subluxation or head at risk signs.
pelvic osteotomies or a combination of pelvic and femoral osteotomies rather than femoral osteotomies alone. Age did not determine the indication for treatment and there was no agreement on the indications for physiotherapy. There was also no consensus on the type of pelvic osteotomy to be used.
Conclusions
The study showed that indications for the treatment of LCPD is based more on the personal experience of the surgeon rather than on scientific data.
Keywords: Legg-Calvé-Perthes disease, Multicentre study, Indication, Operative treatment, Conservative treatment
Introduction
Treatment of Legg-Calvé-Perthes disease (LCPD) is controversial. Most orthopaedic surgeons agree that not all patients with LCPD need operative treatment, but on the other hand not all patients can be treated conservatively or be left alone. The indications for operative or conservative treatment, however, is based on various principles. Some rely on radiological classification systems, others on the age of the patient, range of motion and pain or other clinical symptoms. Treatment can have various aims. The aims of conservative treatment can be: improvement of the range of motion, weight relief, improvement of containment and pain relief. The aims of operative treatment are similar and can be: improvement of the range of motion, containment and weight relief. Various other treatment modalities can reach the same objectives. Improvement of the range of motion can be attempted with physiotherapy, botox injections into the adductor muscles, or mobilisation under anesthesia. Weight relief of the hip joint can be provided by a Thomas splint, crutches, bed rest (with or without traction) or arthrodiastasis. Improvement of containment can be obtained with abduction splints, Petrie casts, trochanteric varus osteotomies, various types of pelvic osteotomies (triple osteotomies, Salter’s innominate osteotomy, Pemberton or Dega’s acetabuloplasties, shelf arthroplasty, Chiari osteotomies) or a combination of a femoral and a pelvic osteotomy. The purpose of this study was to find out among the members of the European Pediatric Orthopaedic Society in which situation what kind of treatment modalities are used and how much agreement or disagreement there is concerning indications to treat.
Materials and methods
A questionnaire was sent to all 297 members of the European Pediatric Orthopaedic Society (in 2005) by email or by mail (if no correct email address was available). The questionnaire was sent up to four times if it was not answered.
In the questionnaire four patients with LCPD (Figs. 1, 2, 3 and 4) were described with two X-rays (AP and axial views) and a short description of the clinical scenario. The principle was to have two younger patients (below six years of age) and two older patients (above age six), one of each with a good range of motion and little subluxation and the other with a poor range of motion and marked subluxation and head at risk signs.
Fig. 1.
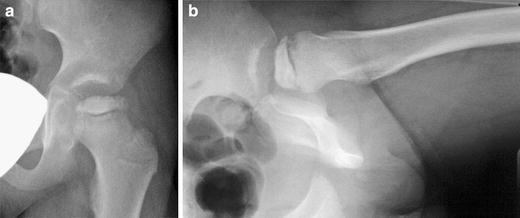
AP and axial X-rays of case 1: five-year-old girl, pain in her groin for the past two months, slight limping, abduction 30°, adduction 40°, internal rotation 20°, external rotation 40° flexion 120°, 10° flexion contracture
Fig. 2.
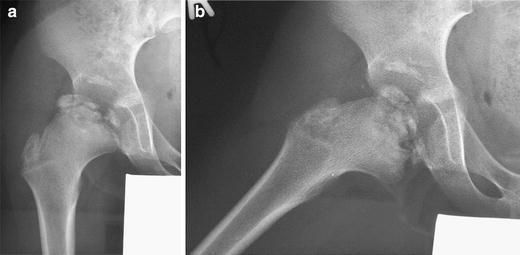
AP and axial X-rays of case 2: eight-year-old boy, no pain, minimal limping, abduction 30°, adduction 40°, internal rotation 40°, external rotation 50°, flexion 120°, no flexion contracture
Fig. 3.
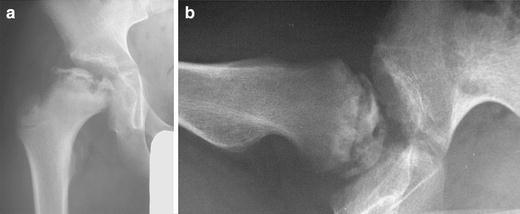
AP and axial X-rays of case 3: 10-year-old boy, pain in his groin for the past 4 months, slight limping, abduction 10°, adduction 20°, internal rotation 20°, external rotation 30°, flexion 110°, 15° flexion contracture
Fig. 4.
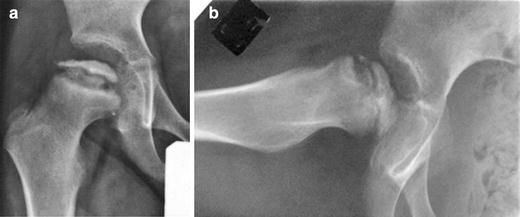
AP and axial X-rays of case 4: five-year-old boy, pain in his groin for the past 3 months, slight limping, abduction 10°, adduction 10°, internal rotation 20°, external rotation 20°, flexion 110°, 20° flexion contracture
Analysis of case 1 (Fig. 1): young patient, good range of motion, minimal subluxation, no lateral calcification, lateral pillar reduced <50% (classified as Herring B).
Analysis of case 2 (Fig. 2): older patient, good range of motion, minimal subluxation, no lateral calcification, lateral pillar intact (classified Herring A).
Analysis of case 3 (Fig. 3): older patient, poor range of motion, head at risk signs (lateral calcification, metaphyseal involvement), lateral pillar markedly reduced (classified Herring C).
Analysis of case 4 (Fig. 4): young patient, poor range of motion, head at risk signs (lateral calcification, metaphyseal involvement), lateral pillar markedly reduced (classified Herring C).
- On each case description the following conservative treatment options were suggested:
- No treatment
- Maintenance of movement (physiotherapy)
- Botox injection
- Mobilisation under anesthesia
- Thomas splint
- Crutches
- Bed rest
- Traction
- Abduction splint.
The following operative treatment options were suggested
Femoral varus osteotomy
Femoral valgus osteotomy
Pelvic triple osteotomy
.
The members of the society were asked to choose among the various treatment options or to describe their own treatment modality (in free text) for the given situation (not future developments). They were allowed to choose several options for the same patient. All members were assured that this was not a test and that there was no right or wrong answer. In addition to the name and address, each member was asked to make a statement on their number of years of experience in paediatric orthopaedics.
Statistical analysis was performed for the proportion of operative versus nonoperative treatment for each case. The distribution of the values among the cases were evaluated with the chi-square test.
Results
Of the 297 email or mail addresses, 57 turned out to be wrong (mails or emails returned). In 16 cases the correct address could be found, so that 256 questionnaires probably reached the EPOS members. Of these, 151 (59%) answered the questionnaire by email or mail. Table 1 shows the number of active participants in the study per country in alphabetical order. The largest numbers of answers (>10) were given from France, USA, Germany, Italy, and Israel.
Table 1.
Number of participants per country (in alphabetical order)
| Argentina | 1 |
| Austria | 3 |
| Belgium | 5 |
| Brazil | 2 |
| Bulgaria | 1 |
| Croatia | 1 |
| Czech Republic | 1 |
| Denmark | 3 |
| Egypt | 4 |
| Finland | 5 |
| France | 16 |
| Germany | 13 |
| Great Britain | 6 |
| Greece | 3 |
| Ireland | 2 |
| Israel | 10 |
| Italy | 13 |
| Japan | 2 |
| Kosovo | 1 |
| Lebanon | 1 |
| Macedonia | 2 |
| Netherlands | 5 |
| Poland | 3 |
| Romania | 1 |
| Serbia | 1 |
| Slovakia | 1 |
| Slovenia | 1 |
| Spain | 9 |
| Sweden | 4 |
| Switzerland | 8 |
| Turkey | 8 |
| USA | 14 |
142 responses (94%) gave information on the number of years of experience in paediatric orthopaedics. It averaged 19.25 years (5–43 years) and gave a total of 2,734 years.
In addition to the tabulated treatment options several participants added the additional options: Conservative—wheelchair; petrie cast; Operative—soft-tissue procedures (adductor tenotomies); arthrodiastasis; femoral varus osteotomy; femoral valgus osteotomy; triple osteotomy; Salter osteotomy; acetabuloplasty (Dega, Pemberton); shelf osteotomy; Chiari osteotomy.
In order to clarify and simplify the evaluation, the treatment options were grouped together in the following way:
Conservative
No treatment
Improvement of the range of motion (physiotherapy, botox injection, mobilisation under anesthesia)
Weight relief (Thomas splint, wheelchair, crutches, bed rest, traction)
Containment treatment (abduction splint, Petrie cast).
Operative
Improvement of the range of motion (soft-tissue procedures = adductor tenotomies)
Weight relief (arthrodiastasis)
- Containment treatment
- Femoral (trochanteric valgus or varus osteotomies)
- Pelvic (triple, Salter, shelf, Chiari osteotomies and Pemberton or Dega acetabuloplasties)
- A combination of femoral and pelvic osteotomies.
The results of case 1 are shown in Fig. 5. The majority opted for conservative treatment, one-third did not see the need for treatment and a small minority preferred surgery.
Fig. 5.
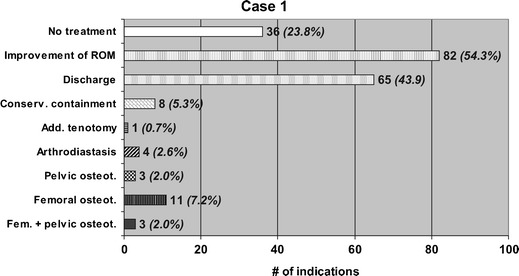
Treatment of case 1 as suggested by the members of the society
Figure 6 shows the proposed treatments in case 2. Almost half of the participants indicated no treatment, slightly more than half proposed surgery.
Fig. 6.
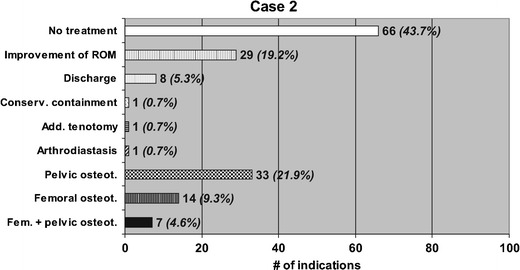
Treatment of case 2 as suggested by the members of the society
The results of the inquiry on case 3 are shown in Fig. 7. Three quarters of the participants proposed an operation with a large variety of procedures.
Fig. 7.
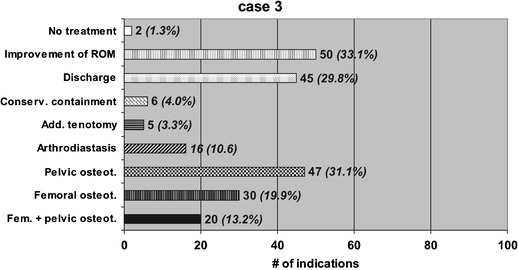
Treatment of case 3 as suggested by the members of the society
The suggestions for case 4 are shown in Fig. 8. Just under 50% proposed surgery, with a large variety of procedures. Most of the other preferred conservative treatment and only a small minority no treatment at all.
Fig. 8.
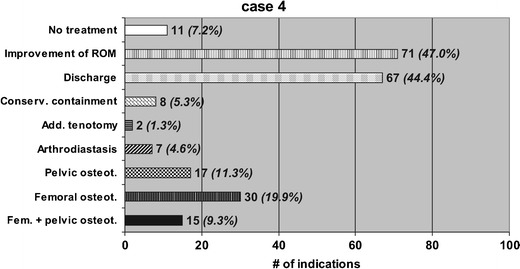
Treatment of case 4 as suggested by the members of the society
The proportion of suggested operative versus nonoperative treatment was statistically significantly different among the cases (P < 0.001) except cases 2 and 4.
Table 2 shows the various types of pelvic osteotomies that were suggested, differentiated between the two younger and the two older patients. Triple osteotomies were most commonly proposed in both age groups.
Table 2.
Types of pelvic osteotomies
| All four patients | Percent % | Young patients (cases 1 and 4) | Percent % | Older patients (cases 2 and 3) | Percent % | |
|---|---|---|---|---|---|---|
| Triple osteotomy | 83 | 54.6 | 20 | 51.3 | 63 | 55.8 |
| Shelf procedure | 35 | 23.0 | 1 | 2.6 | 34 | 30.1 |
| Salter (innominate) osteotomy | 20 | 13.2 | 12 | 30.8 | 8 | 7.1 |
| Acetabuloplasty (Dega, Pemberton) | 13 | 8.6 | 6 | 15.4 | 7 | 6.2 |
| Chiari-osteotomy | 1 | 0.7 | 0.0 | 1 | 0.9 | |
| Total | 152 | 100.0 | 39 | 100.0 | 113 | 100.0 |
Discussion
The results of the study show that there is a lot of disagreement in assessing Perthes disease and its treatment. We provided four cases with a relatively clear clinical scenario, two cases with a good prognosis (with good range of motion, no head at risk signs, Herring type A or B), one of them rather young (5 years, case 1), the other in an older age group (nine-year-old, case 2). The other two cases clearly presented a worse prognosis, having a poor range of motion, marked head at risk signs, and both being classified as Herring C. Again, one is young (five years, case 4) and one is in an older age group (10 years, case 3).
We looked at the results of this inquiry and tried to identify factors that may play a role in consensus (good agreement), only a trend or no agreement, respectively. We defined consensus as agreement in >80% of replies. Statements with between 50 and 80% agreement were defined a tendency. Disagreement was defined by less than 50% agreement.
There was consensus on following statements:
No operation when young and good range of motion
No weight relief when older and good range of motion
No conservative containment treatment (abduction splint, Petrie cast)
Arthrodiastasis is used in only very few centers
We observed a tendency concerning the following statements:
Operation when older and poor range of motion
No weight relief
Operation only when subluxation or head at risk signs
Pelvic osteotomies or a combination of pelvic and femoral osteotomies rather than femoral osteotomies alone
At the pelvis mainly triple osteotomies
There was disagreement on the following statements:
Age determines indication to treatment
Physiotherapy only when poor mobility
There was also no agreement on the type of pelvic osteotomy to be used.
In our view, it is quite astonishing how much disagreement there is on the various treatment options in the four cases. There may be two reasons. Either the situation is assessed in a different way, or—when there is no difference in the assessment—different treatment options are preferred. Most of the participants would probably agree that the assumed prognosis at a given period of time should determine the need for therapy.
Many reports of long-term follow-up studies make statements on prognostic factors. One of them is age [1, 2, 3, 4, 5]. Most authors agree that the younger the patients are at the onset of the disease, the better the prognosis. There seems to be a magic age limit at six years. Many authors state that below this age, the prognosis is good, irrespective of other prognostic factors.
Relatively sound prognostic factors seem to be the appearance of lateral calcification, extrusion, subluxation and containment. Catterall [6] advocated in 1971 the significance of these factors and this was confirmed in many other studies [2, 7, 3, 4, 5]. Lateral calcification and subluxation are both signs of deterioration of containment. This situation carries the risk of a continuing deformation of the femoral head. An aspherical head is more at risk for osteoarthritis than a spherical one [8]. Other factors that Catterall called risk factors like the metaphyseal involvement or the gage sign have proven to be of minor importance [2, 4, 5].
The range of motion also has a significance for prognosis, although only very few authors addressed this factor [9]. Patients with a poor range of motion often have shortening of the adductor muscles, which increases the tendency to subluxation of the femoral head.
The proportion of the necrotic area within the femoral head also has some prognostic value, but seems to be less critical than initially assumed. Both the Catterall classification and the Salter–Thompson classification consider the extension of the necrosis in the grouping. There is agreement that patients with a limited extent of necrosis (Catterall group I = only the anterolateral part is involved) or Salter–Thompson A (magnitude of the subchondral fracture <50%) have a good prognosis. Prognosis of cases in Catterall groups II–IV or Salter–Thompson B are more reserved [10], but no statement can be made to distinguish among these groups. Some long-term follow-up studies even showed that patients with total head involvement (Catterall group IV) have a slightly better prognosis than patients with partial head involvement (Catterall group II and especially III), because at the end stage the head is less aspherical [9, 11].
Herrings lateral pillar classification [1] does not take the total amount of necrosis into consideration, but it reflects the relative height of the lateral pillar. This has significant implications for containment. The prognostic value of this classification seems to be better than of the other two [12, 13], even if in many cases the grouping has to be changed in the course of the disease [14].
Gender also seems to have an influence on prognosis. The disease is four times more common in boys, but the average outcome is worse in girls than boys [4].
In a recent article a prognostic formula was calculated. It cumulates an age score, an involvement score and a subluxation score. The formula seems to have a good predictive value. In another article [15] Herring’s lateral pillar classification is combined into a new score with the posterior pillar classification.
A recently published prospective multicentre study [16] of 438 patients with 451 affected hips made clear statements concerning the outcome of treatment. The lateral pillar classification and age at the time of onset of the disease are strongly correlated with outcome. Patients who were over the age of eight years at the time of onset and had a hip in the lateral pillar B group or B/C border group had a better outcome with surgical treatment than they did with nonoperative treatment. Group B hips in children who were less than eight years of age at the time of onset had very favorable outcomes unrelated to treatment, whereas group C hips in children of all ages frequently had poor outcomes, which also appears to be unrelated to treatment.
According to the present study, cases 1 and 2 (both younger than eight years at the onset of the disease and Herring group A or B) do not need any treatment and cases 3 and 4 (both Herring group C) will have a poor outcome, irrespective of the treatment.
This study raises some important questions about core knowledge of Perthes disease in the paediatric orthopaedic community. In view of the major disagreements found further prospective studies are needed to deepen our knowledge on the treatment outcome in greater detail. There is also a need for guidelines to make sure that the recommendations based on the findings of such studies are respected in clinical practice.
References
- 1.Herring JA, Kim HT, Browne R. Legg-Calvé-Perthes’ disease. Part II: prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg (Am) 2004;86:2121–2134. [PubMed] [Google Scholar]
- 2.Ippolito E, Tudisco C, Farsetti P. The long term prognosis of unilateral Perthes’ disease. J Bone Joint Surg (Br) 1987;69:243–250. doi: 10.1302/0301-620X.69B2.3818755. [DOI] [PubMed] [Google Scholar]
- 3.McAndrew MP, Weinstein SL. A long-term follow-up of Legg-Calvé-Perthes’ diasease. J Bone Joint Surg (Am) 1984;66:860–869. doi: 10.2106/00004623-198466060-00006. [DOI] [PubMed] [Google Scholar]
- 4.Mukherjee A, Fabry G. Evaluation of the prognostic indices in Legg-Calvé-Perthes’ disease: Statistical analysis of 116 hips. J Pediatr Orthop. 1991;11:153–158. [PubMed] [Google Scholar]
- 5.Yrjonen T. Prognosis in Perthes’ disease after noncontainment treatment. 106 hips followed for 28–47 years. Acta Orthop Scand. 1992;63:523–526. doi: 10.3109/17453679209154728. [DOI] [PubMed] [Google Scholar]
- 6.Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg (Br) 1971;53:37–53. [PubMed] [Google Scholar]
- 7.Kamegaya M, Saisu T, Miura Y, Moriya H. A proposed prognostic formula for Perthes’ disease. Clin Orthop Relat Res. 2005;440:205–208. doi: 10.1097/01.blo.0000180601.23357.d9. [DOI] [PubMed] [Google Scholar]
- 8.Stevens D, Tao S, Glueck C. Recurrent Legg-Calvé-Perthes’ disease: case report and long-term followup. Clin Orthop. 2001;385:124–129. doi: 10.1097/00003086-200104000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Stulberg SD, Cooperman DR, Wallenstein R. The natural history of Legg-Calvé-Perthes’ disease. J Bone Joint Surg (Am) 1981;63:1095–1108. [PubMed] [Google Scholar]
- 10.Wiig O, Svenningsen S, Terjesen T. Evaluation of the subchondral fracture in predicting the extent of femoral head necrosis in Perthes disease: a prospective study of 92 patients. J Pediatr Orthop B. 2004;13:293–298. doi: 10.1097/01202412-200409000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Lecuire F. The long-term outcome of primary osteochondritis of the hip (Legg-Calvé-Perthes’ disease) J Bone Joint Surg (Br) 2002;84:636–640. doi: 10.1302/0301-620X.84B5.12124. [DOI] [PubMed] [Google Scholar]
- 12.Farsetti P, Tudisco C, Caterini R, Potenza V, Ippolito E. The Herring lateral pillar classification for prognosis in Perthes’ disease. J Bone Joint Surg (Br) 1995;77:739–742. [PubMed] [Google Scholar]
- 13.Ritterbusch JF, Shantharam SS, Gelinas C. Comparison of lateral pillar classification and Catterall classification of Legg-Calvé-Perthes’ disease. J Pediatr Orthop. 1993;13:200–202. [PubMed] [Google Scholar]
- 14.Lappin K, Kealey D, Cosgrove A. Herring classification: how useful is the initial radiograph? J Pediatr Orthop. 2002;22:479–482. [PubMed] [Google Scholar]
- 15.Sugimoto Y, Akazawa H, Miyake Y, Mitani S, Asaumi K, Aoki K, Inoue H. A new scoring system for Perthes’ disease based on combined lateral and posterior pillar classifications. J Bone Joint Surg (Br) 2004;86:887–891. doi: 10.1302/0301-620X.86B6.14622. [DOI] [PubMed] [Google Scholar]
- 16.Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calvé-Perthes’ disease. J Pediatr Orthop. 1992;12:143–150. doi: 10.1097/01241398-199203000-00001. [DOI] [PubMed] [Google Scholar]


