Abstract
Purpose
Unstable slipped capital femoral epiphysis is rare, but is frequently associated with avascular necrosis. The rapid and complete reduction of the epiphysis displacement was shown to be responsible for this complication. We present the preliminary results of a progressive reduction technique of epiphysis displacement.
Methods
A total of 11 patients treated using progressive traction and internal fixation were reviewed retrospectively. Only children who underwent clinical and radiological follow-up for at least 18 months were included in this study to detect avascular necrosis.
Results
The mean posterior displacement of the femoral head was 67° and mean traction duration was 13 days. Of the patients, 2 had cutaneous problems requiring traction interruption, one on day 5 and the other on day 9. The mean residual slip was 16° and 3 patients had complete or partial avascular necrosis well tolerated at the final follow-up.
Conclusion
Our experience showed that if traction is supported for more than 2 weeks, a good correction of the epiphysis displacement can be obtained. Our short series does not allow affirmation of the superiority of our therapeutic strategy, especially with regards to avascular necrosis of the femoral head.
Keywords: Unstable slipped capital femoral epiphysis, Progressive reduction, Traction, Avascular necrosis
Introduction
Slipped capital femoral epiphysis (SCFE) is the most common disorder of the hip in early adolescence. The mean age of patients in whom SCFE occurs is 12 years old for girls and 14 years old for boys. This pathology is characterized, most often, by a progressive posterior displacement of capital femoral epiphysis from the femoral neck [1]. The femoral head remains trapped in the acetabulum. This epiphysis slip leads to a deformation and retroversion of the upper femoral end. The incidence of SCFE is approximately 2 per 100,000 in the general population [2]. Various forms of SCFE have been described. Stable forms occur in 80% of the cases. The symptoms are often moderated and evolve over several weeks or even months. In contrast, there are the "unstable" slips [3], which can occur on previously unknown stable slips. The proof of this pre-existent slip is radiological, showing a remodelling and new bone formation at the epiphyso–metaphyseal junction. Thus, hip or knee pain precedes the brutal episode that reveals the epiphysis slip. The displacement involves a violent and sudden pain of the hip and a total impossibility to walk without crutches. Thus, unstable SCFE is considered as a “femoral neck fracture” without violent traumatism. Two devastating complications are most frequently associated with unstable SCFE: avascular necrosis (AVN) and chondrolysis [4]. Whereas chondrolysis can occur spontaneously, rapid and complete reduction of epiphysis displacement has been shown to be responsible for AVN [5–7].
The purpose of this work was to present the preliminary results of a progressive reduction technique of epiphysis displacement. Technical details of the technique are presented. The advantages and disadvantages of our technique are discussed.
Materials and methods
Previously used technique
At our department, until 1997, we reduced the displacement of the unstable SCFE in emergency under general anaesthesia by moderate traction with or without progressive medial rotation applied on an orthopaedic table. Plain frontal and lateral radiographs proved epiphysis reduction before surgical metaphyso–epiphyseal fixation. One or two screws were percutaneously used for internal fixation. No attempt was ever made to evacuate articular effusion. The significant rate (30–50%) of AVN reported in the literature [4–14] in response to manipulative reduction of unstable SCFE under general anaesthesia led us to change our method, taking into account that intempestive manoeuvres under general anaesthesia could be dangerous for femoral head vessels.
The progressive slip reduction by axial traction
Since 1997, we have reduced epiphysis displacement by progressive traction without general anaesthesia. Thus, patients underwent permanent longitudinal traction of both lower limbs with sticking bands. Sticking bands were placed longitudinally from the upper part of the tight down to the ankle. Circular bands were then applied, avoiding excessive tension. Skin tolerance was checked every day, after removing and replacing circular bands. Slipped epiphysis limb received a progressive traction in order to reach up to 50% of the body weight (sometimes up to 25 kg in overweight children). The other lower limb received a mid-weighted traction. The period of traction was divided into three successive steps:
During the first week, the traction was progressively increased, keeping the lower limb in the body’s axis. Radiographs of frontal hips were repeated every 2–3 days until an epiphyseal ascension was observed.
During the second week, after epiphyseal ascension was obtained, a progressive abduction was applied, in order to improve the reduction of the epiphysis slip. Frontal-hip radiographs were also repeated every 2–3 days to control the reduction.
During the third week, abduction was completed and femoral internal rotation was obtained using a “derotation” band surrounding the tight. Internal rotation of the limb had to be carried out very carefully because, if the epiphysis was insufficiently reduced, it could be dangerous for the epiphyseal vessels. In this case, femoral internal rotation could be responsible for a periosteum and vascular twist at the posterior and inferior part of the metaphyso–epiphyseal junction (Fig. 1). Frontal-hip radiographs were used to assess epiphysis reduction at the end of the third week. Once the correction was considered optimal, bilateral epiphysis fixation using percutaneous screws was performed. The unstable side was always operated on first to avoid intempestive displacement due to the patient's positioning under general anaesthesia. This placement of the patient was carried out carefully to avoid a brutal additional epiphysis displacement, which could generate a lesion of the epiphysis vessels.
Fig. 1.
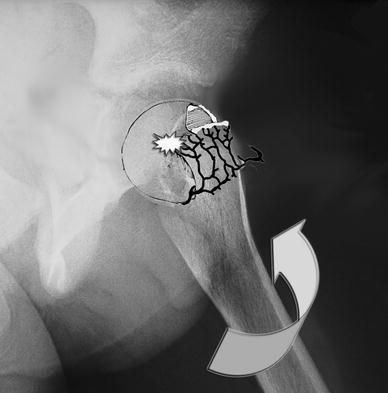
Excessive femoral internal rotation could be responsible for a periosteum and vascular twist at the posterior and inferior part of the metaphyso–epiphyseal junction
After surgery, the patient had to stand up using crutches within few days. Weight bearing on the unstable side was not authorized before 6 weeks. A technetium 99* bone scan was performed at the end of the first month to confirm the vitality of the femoral head before walking without crutches. Clinical and radiological follow-up was carried out every 6 months. Our protocol of progressive reduction by traction is summarized in Fig. 2.
Fig. 2.
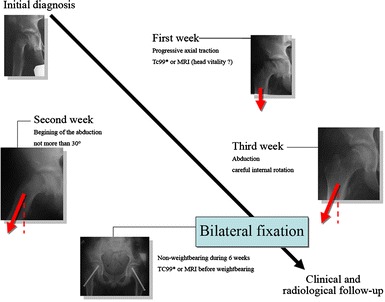
The three successive steps of the epiphysis reduction using the progressive axial traction technique
Results
Between 1997 and 2004, 11 children—five boys and six girls—were treated using this technique. Only those who underwent clinical and radiological follow-up for at least 18 months were included in our study for detection of AVN. Mean age was 11 years and 10 months old (10- to 14-year old). The mean body mass index was 24.09 kg/m2, which corresponds to a moderate obesity. Mean follow-up was 3 years 2 months (18 months to 5 years).
Unstable displacement was due to minor trauma (fall from patient's height) in 8 cases. Of the children, 5 experienced moderate pain of the hip or knee for several weeks, which suggested the presence of a preexisting stable epiphysis.
In all cases, following the unstable displacement, the walk was impossible without crutches. Frontal and lateral radiographs of the hip showed unstable displacement of capital femoral epiphysis. Mean lateral (posterior) displacement was 75° (60–85°).
Mean traction duration was 13 days. Of the patients, 2 had cutaneous problems requiring traction interruption, one on day 5 and the other on day 9. At the end of the traction period, the mean residual posterior displacement of the femoral head was 16°. The correction of the slip angle was from 15° to 80°. The details of the traction procedure are summarized in Table 1.
Table 1.
Details of corrections using the progressive axial traction technique
| Patient | Initial slip (degree) | Traction duration (days) | Traction weight (kg) | Final slip (degree) | Gain (degree) |
|---|---|---|---|---|---|
| 1 | 40 | 9 | 12 | 15 | 25 |
| 2 | 50 | 16 | 14 | 0 | 50 |
| 3 | 60 | 5 | 10 | 45 | 15 |
| 4 | 60 | 16 | 12 | 40 | 20 |
| 5 | 75 | 12 | 12 | 15 | 60 |
| 6 | 80 | 28 | 11 | 0 | 80 |
| 7 | 80 | 13 | 18 | 10 | 70 |
| 8 | 85 | 11 | 21 | 15 | 70 |
| 9 | 85 | 10 | 11 | 10 | 75 |
| 10 | 75 | 22 | 13 | 20 | 55 |
| 11 | 65 | 20 | 14 | 15 | 50 |
Both capital epiphyses were fixed percutaneously in all patients (Fig. 3). The post-operative course was uneventful for all patients.
Fig. 3.

Example of a bilateral percutaneous fixation after epiphyseal reduction during a 3-week period in patient 10
At final follow-up, 8 children had satisfactory clinical and radiological results. In all 8, the femoral head was free from any sign of AVN, with no modification of the residual posterior displacement. A complete AVN was observed in 2 patients. At the 4-year follow-up, hip function remained satisfactory, despite articular progressive destruction (Fig. 4). These 2 children had no pain during the first 4 years of follow-up. A third patient had a limited peri-foveal AVN. This child remains completely asymptomatic 2 years after the surgery.
Fig. 4.

A case of complete avascular necrosis in patient 7. Four years after surgery, this state remains well tolerated
Discussion
The unstable forms of SCFE are rare but can have disastrous consequences on the anatomy and the function of the hip [4, 8, 11]. Their treatment remains a current problem for many surgeons [4]. On the one hand, fixing the epiphysis without reduction has been proposed by several authors [15]. This manner of treatment ought to be proposed only in cases of small slip, because epiphysis displacement leads to a coxa retrorsa with vicious attitude in external rotation of the lower limb, limited internal rotation of the hip and a risk of mid-term osteoarthosis. On the other hand, correcting epiphyseal displacement increases the risk of AVN and rapid destruction of the hip [6, 9].
The origins of chondrolysis, which can also be responsible for early osteoarthosis, remain debatable. Some authors [16, 17] argue that intra-articular hip effusion, constant in unstable SFCE, is responsible for articular cartilage necrosis. This is the reason that a systematic evacuation of the intra-articular effusion during surgical treatment was proposed. Other authors suggest that chondrolysis could be secondary to technical problems, such as joint space effraction during pin or screw placement. For Sternlicht and Aronsson [8, 18], chondrolysis is the consequence of the osteosynthesis device protrusion in the articular space due to femoral head collapse secondary to AVN.
Few studies [4–6, 8–14] concern the treatment of unstable cases of SCFE. The results of these studies are sometimes biased by the fact that the “unstable” type of SFCE is not precisely defined in patients’ inclusion criteria. In a study by Peterson that included 91 “unstable” SCFEs [14], posterior epiphyseal displacement was often moderated; this was not very evocative of unstable SCFE cases. However, this study did show the interest of a fast reduction of capital slip under general anaesthesia.
AVN is a devastating complication of unstable SCFE, secondary to the interruption of epiphyseal vessels. AVN incidence varies between 25% and 50% of cases [4] and seems to increase when a reduction of the displacement is performed under general anaesthesia. The vascular anatomy of the proximal femur has been well described by Trueta [19–22]. Although variations among gender and race have been reported, a fairly consistent vascular pattern persists throughout life [23]. The posterior-superior retinacular vessels provide the major blood supply to the epiphysis. These vessels lie loosely under the synovial membrane along the postero-superior aspect of the femoral neck. The postero-superior retinacular vessels can be disrupted in traumatic circumstances, as in unstable SCFE (Fig. 5). Under this pathological condition, the epiphyseal vascularization is made by rare anastomotic vessels between the antero-inferior retinacular vessels and the round ligament artery. It is likely that the ischaemia of the femoral head in unstable SCFE occurs at the time of the unstable episode. The evaluation of epiphysis ischaemia is difficult during this phase. Sometimes, we performed an early technetium 99* bone scan, the analysis of which was difficult because the epiphyseal displacement hid the tracer fixation. In our opinion, early MRI needs to be taken into account, which we now do in our department.
Fig. 5.
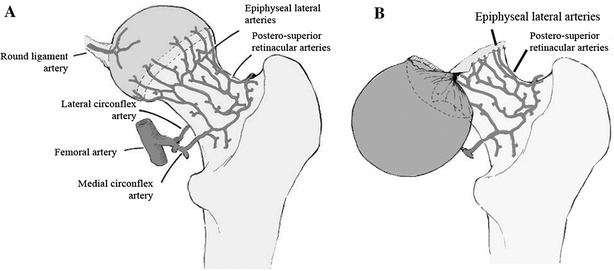
Under normal conditions, the posterior-superior retinacular vessels provide the major blood supply to the epiphysis (a). The postero-superior retinacular vessels can be disrupted under traumatic circumstances, such as during unstable SCFE (b)
We propose that, even in the case of supposed initial ischaemia of the femoral head, a progressive reduction by traction must be performed. Due to the very high weight needed for reduction, skeletal traction could be proposed. In our experience, with a precise and careful technique and monitoring, skin traction is an effective and less invasive technique even if the duration of traction could be responsible for skin problems, as in two cases of the current series. The reduction in emergency of unstable SCFE does not solve the problem of postero-superior retinacular vessel disruption and can be responsible for a worsening of the epiphyseal ischaemia by inducing a rupture or a vasospasm of the remaining intact vessels. We had to deplore three AVN in our short series of patients. Because of these complications and our limited experience and cohort, we cannot affirm the superiority of our therapeutic strategy, especially with regards to AVN incidence. The exhaustive results of this procedure need to be assessed with a larger cohort of patients. Nevertheless, the progressive traction technique provided satisfactory reductions of epiphyseal displacements, making the performance of epiphyseal fixations with favorable mechanical conditions possible.
Acknowledgments
The authors gratefully acknowledge the assistance provided by Dr. Carl Stanitski and Dr. Henri Bensahel in the preparation of this manuscript.
References
- 1.Boero S, Brunenghi GM, Carbone M, Stella G, Calevo MG. Pinning in slipped capital femoral epiphysis: long-term follow-up study. J Pediatr Orthop B. 2003;12:372–379. doi: 10.1097/01.bpb.0000079202.23239.64. [DOI] [PubMed] [Google Scholar]
- 2.Cooperman DR, Charles LM, Pathria M, Latimer B, Thompson GH. Post-mortem description of slipped capital femoral epiphysis. J Bone Joint Surg Br. 1992;74:595–599. doi: 10.1302/0301-620X.74B4.1624523. [DOI] [PubMed] [Google Scholar]
- 3.Rostoucher P, Bensahel H, Pennecot GF, Kaewpornsawan K, Mazda K. Slipped capital femoral epiphysis: evaluation of different modes of treatment. J Pediatr Orthop B. 1996;5:96–101. doi: 10.1097/01202412-199605020-00008. [DOI] [PubMed] [Google Scholar]
- 4.Stanitski CL. Acute slipped capital femoral epiphysis: treatment alternatives. J Am Acad Orthop Surg. 1994;2:96–106. doi: 10.5435/00124635-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Gordon JE, Abrahams MS, Dobbs MB, Luhmann SJ, Schoenecker PL. Early reduction, arthrotomy, and cannulated screw fixation in unstable slipped capital femoral epiphysis treatment. J Pediatr Orthop. 2002;22:352–358. [PubMed] [Google Scholar]
- 6.Dietz F (1997) How best to treat acute or unstable slipped capital femoral epiphysis with great interest. Clin Orthop Relat Res 281–283 [PubMed]
- 7.Casey BH, Hamilton HW, Bobechko WP (1972) Reduction of acutely slipped upper femoral epiphysis. J Bone Joint Surg Br 54:607–614 [PubMed]
- 8.Aronsson DD, Loder RT (1996) Treatment of the unstable (acute) slipped capital femoral epiphysis. Clin Orthop Relat Res 99–110 [PubMed]
- 9.Dietz FR (1994) Traction reduction of acute and acute-on-chronic slipped capital femoral epiphysis. Clin Orthop Relat Res 101–110 [PubMed]
- 10.Fahey JJ, O’Brien ET (1965) Acute slipped capital femoral epiphysis: review of the literature and report of ten cases. J Bone Joint Surg Am 47:1105–1127 [PubMed]
- 11.Loder RT (2001) Unstable slipped capital femoral epiphysis. J Pediatr Orthop 21:694–699 [PubMed]
- 12.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75:1134–1140. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen HO. Acute slipped capital femoral epiphysis. Treatment in eight cases. Acta Orthop Scand. 1975;46:987–995. doi: 10.3109/17453677508989288. [DOI] [PubMed] [Google Scholar]
- 14.Peterson MD, Weiner DS, Green NE, Terry CL. Acute slipped capital femoral epiphysis: the value and safety of urgent manipulative reduction. J Pediatr Orthop. 1997;17:648–654. doi: 10.1097/01241398-199709000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Seller K, Wild A, Westhoff B, Raab P, Krauspe R (2006) Clinical outcome after transfixation of the epiphysis with Kirschner wires in unstable slipped capital femoral epiphysis. Int Orthop 30:342–347 [DOI] [PMC free article] [PubMed]
- 16.Jofe MH, Lehman W, Ehrlich MG. Chondrolysis following slipped capital femoral epiphysis. J Pediatr Orthop B. 2004;13:29–31. doi: 10.1097/00009957-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Vrettos BC, Hoffman EB. Chondrolysis in slipped upper femoral epiphysis. Long-term study of the aetiology and natural history. J Bone Joint Surg Br. 1993;75:956–961. doi: 10.1302/0301-620X.75B6.8245091. [DOI] [PubMed] [Google Scholar]
- 18.Sternlicht AL, Ehrlich MG, Armstrong AL, Zaleske DJ. Role of pin protrusion in the etiology of chondrolysis: a surgical model with radiographic, histologic, and biochemical analysis. J Pediatr Orthop. 1992;12:428–433. doi: 10.1097/01241398-199207000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Trueta J, Harrison MH. The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br. 1953;35:442–461. doi: 10.1302/0301-620X.35B3.442. [DOI] [PubMed] [Google Scholar]
- 20.Trueta J. The normal vascular anatomy of the human femoral head during growth. J Bone Joint Surg Br. 1957;39:358–394. doi: 10.1302/0301-620X.39B2.358. [DOI] [PubMed] [Google Scholar]
- 21.Trueta J. Appraisal of the vascular factor in the healing of fractures of the femoral neck. J Bone Joint Surg Br. 1957;39:3–5. doi: 10.1302/0301-620X.39B1.3. [DOI] [PubMed] [Google Scholar]
- 22.Trueta J (1997) The normal vascular anatomy of the femoral head in adult man. 1953. Clin Orthop Relat Res (334):6–14 [PubMed]
- 23.Brodetti A. Blood supply to the femoral neck in relation to the damaging effects of nails and screws. J Bone Joint Surg Br. 1960;42:794–801. [Google Scholar]


