Abstract
Congenital vertical talus is an uncommon foot deformity that is present at birth and results in a rigid flatfoot deformity. Left untreated the deformity can result in pain and disability. Though the exact etiology of vertical talus is unknown, an increasing number of cases have been shown to have a genetic cause. Approximately 50% of all cases of vertical talus are associated with other neuromuscular abnormalities or known genetic syndromes. The remaining 50% of cases were once thought to be idiopathic in nature. However, there is increasing evidence that many of these cases are related to single gene defects. Most patients with vertical talus have been treated with major reconstructive surgeries that are fraught with complications such as wound necrosis, talar necrosis, undercorrection of the deformity, stiffness of the ankle and subtalar joint, and the eventual need for multiple operative procedures. Recently, a new approach to vertical talus that consists of serial casting and minimal surgery has resulted in excellent correction in the short-term. Longer follow-up will be necessary to ensure maintenance of correction with this new technique. A less invasive approach to the correction of vertical talus may provide more favorable long-term outcomes than more extensive surgery as has been shown to be true for clubfoot outcomes.
Keywords: Congenital vertical talus, Flatfoot, Treatment, Genetics, Etiology
Introduction
Congenital vertical talus, also known as congenital convex pes valgus, is an uncommon foot deformity that is present at birth and has an estimated incidence of 1 in 10,000 [1]. It is characterized by a fixed dorsal dislocation of the navicular on the talar head and neck [2] resulting in a rigid flatfoot deformity. It occurs as an isolated deformity (idiopathic) in approximately half of all cases and is associated with neuromuscular and genetic disorders in the remaining cases [1, 3–5]. Fifty percent of children have bilateral involvement and there is no sex predilection [1]. Left untreated a congenital vertical talus causes significant disability long-term. Ambulation is usually not delayed but the gait is usually awkward with difficulty balancing. The shoes often show abnormal wear and pain often develops in early adolescence [6]. Since the heel does not touch the ground, the patients have poor push-off and are forced to weight bear on the talar head, which develops painful callosities. An emphasis of this review will be on recent findings regarding the genetic etiology of idiopathic vertical talus as well as a new approach to treating the deformity that consists of serial manipulations, castings, and minimal surgery.
Pathogenesis
The exact etiology of vertical talus in most cases is not known. Theories include increased intrauterine pressure and resultant tendon contractures, or an arrest in fetal development occurring between the 7th and 12th week of gestation [7, 8]. Approximately one-half of all cases of vertical talus occur in association with neurologic abnormalities [2, 9] or genetic syndromes [10, 11]. Associated neurologic abnormalities can be divided into two broad categories: central nervous system defects or neuromuscular disorders. Though the remainder of vertical talus cases were once thought to be idiopathic in nature, there is increasing evidence for a genetic cause as many families demonstrate an autosomal dominant inheritance pattern [5, 12–14] (Table 1).
Table 1.
Etiologies of congenital vertical talus (additional malformations, chromosomal abnormalities and genetic syndromes)
| Central nervous system/spinal cord |
| Myelomeningocele |
| Spinal muscular atrophy |
| Diastematomyelia |
| Sacral agenesis |
| Muscle |
| Distal arthrogryposis |
| Arthrogryposis multiplex |
| Neurofibromatosis |
| Chromosomal abnormality |
| Trisomy 18 |
| Trisomy 15 |
| Trisomy 13 |
| Known genetic syndromes |
| Neurofibromatosis |
| Prune-Belly syndrome |
| Rasmussen syndrome |
| Split hand and split foot |
| Costello syndrome |
| De Barsy syndrome |
| Single gene defects |
| HOXD10 |
| CDMP1 |
Central nervous system abnormalities/neuromuscular disorders
Congenital central nervous system defects commonly seen with congenital vertical talus include myelomeningocele, sacral agenesis, and diastematomyelia. Muscle imbalance is thought to be the cause of the vertical talus deformity in these disorders resulting from relative tibialis posterior muscle deficiency [15]. In one series, 10% of children with myelomeningocele who had foot deformities had vertical talus [9]. Neuromuscular disorders associated with vertical talus include arthrogryposis, spinal muscular atrophy, and neurofibromatosis; vertical talus in these disorders is also thought to be associated with muscle imbalance. Vertical talus deformities associated with neurologic disorders tend to be more rigid and difficult to treat than idiopathic vertical talus.
Genetics
Genetic abnormalities associated with vertical talus include aneuploidy of chromosome 13, 15 and 18. A variety of syndromes have also been described in which vertical talus is a clinical manifestation. De Barsy syndrome is a rare genetic syndrome characterized by severe cutis laxa, joint hypermobility, growth retardation, mental retardation, and characteristic facies; orthopaedic manifestations include hip dislocation, scoliosis, and congenital vertical talus [16]. Prune belly syndrome is an uncommon disorder characterized by intrauterine urinary obstruction associated with oligohydramnios and resultant intrauterine crowding. The limited intrauterine space is thought to result in some of the orthopaedic manifestations of this disorder including developmental dislocation of the hip, clubfeet, metatarsus adductus, congenital muscular torticollis, and vertical talus [17]. Vertical talus has also been described with Costello syndrome, a rare condition characterized by short stature, developmental delay, characteristic facies, and redundant skin of the neck, palms, soles, and fingers [18]. Other orthopaedic manifestations of Costello syndrome include clubfoot, brachydactyly, and syndactyly, as well as multiple upper and lower extremity joint contractures. In addition, vertical talus has been described in Rasmussen syndrome (external auditory canal atresia, vertical talus, and hypertelorism) [19] and in a single individual with split hand and split foot malformation associated with a deletion of chromosome 7q21.1–q21.3 [20].
There have been recent advances in understanding the genetic etiology of idiopathic vertical talus. Based on the observation of a positive family history in 12–20% of patients with idiopathic vertical talus, a genetic etiology seemed likely. In those with a positive family history of vertical talus, the deformity is inherited in an autosomal dominant manner with incomplete penetrance. [4, 5, 14] Through the study of multiple families with vertical talus, a mutation in the HOXD10 gene was recently found to be responsible for vertical talus in one of these families consisting of six individuals with isolated congenital vertical talus [14]. HOX genes are a large group of highly conserved transcription factors that control development along the body axis. Mutations in several of the HOX genes have been shown to result in a variety of both upper and lower extremity abnormalities including synpolydactyly [21], radioulnar synostosis and amegakaryocytic thrombocytopenia [22], and hand–foot–genital syndrome[23].
Earlier, this same mutation in HOXD10 had been described in a single family in which both congenital vertical talus and a Charcot–Marie–tooth-like foot deformity segregated [24]. This gene was then studied in 16 patients with idiopathic vertical talus and no family history of the disorder to see if the same gene was responsible for sporadic vertical talus. However, mutations in this same gene were not identified in this patient group, suggesting that all idiopathic vertical talus deformities cannot be explained by one gene defect [25]. This has led to the investigation of other candidate genes for vertical talus, with one other interesting finding to date. A mutation in the cartilage-derived morphogenetic protein-1 (CDMP-1) gene has been identified in a large family with variable hand and foot abnormalities, including a child with isolated vertical talus. Mutations in CDMP-1 have been previously described in Grebe and Hunter-Thompson forms of acromelic skeletal dysplasia as well as in DuPan syndrome [26–28]; these disorders present with severe limb abnormalities. Mutations in CDMP-1 have also been described in patients with brachydactyly type C, a condition that is characterized by short middle phalanges and first metacarpals [29].
Pathoanatomy
Both autopsy and surgical findings have contributed to the understanding of the pathologic anatomy of vertical talus [15, 30–32]. Contractures of the tibialis anterior, extensor hallucis brevis, peroneus tertius, peroneus longus, peroneus brevis, and the Achilles tendon are present. The talonavicular joint capsule is dorsally contracted. The navicular is displaced both dorsally and laterally with respect to the head and neck of the talus. Due to lack of appropriate articulation with the talus, the navicular is hypolastic and wedge shaped. The talar head and neck are flattened and medially deviated. The extreme plantar flexed position of the talus results in attenuation of the calcaneonavicular, or spring ligament. The calcaneus is plantar flexed and externally rotated. The angle between the axes of the talus and calcaneus is increased. The middle and anterior subtalar joint facets are hypoplastic and absent in severe cases. In severe deformities, the cuboid is laterally displaced resulting in dorslateral subluxation or dislocation of the calcaneocuboid joint. The posterior tibial tendon is often subluxed anteriorly over the medial malleolus while the peroneus longus and peroneus brevis may be subluxed over the lateral malleolus; the subluxed tendons may function as dorsiflexors rather than plantar flexors.
Clinical features
Congenital vertical talus is characterized by hindfoot equinus, hindfoot valgus, forefoot abduction, and forefoot dorsiflexion at the midtarsal joint. This is usually recognized in the newborn period by the rigidity of the deformities, but it must be differentiated from the more common calcaneovalgus foot, posterior medial bowing of the tibia, and flexible flatfoot. In congenital vertical talus, the plantar surface of the foot is convex creating a rocker-bottom appearance (Fig. 1a). There are deep creases on the dorsolateral aspect of the foot anterior and inferior to the lateral malleolus (Fig. 1b). The peroneal and anterior tibialis tendons are contracted, and the foot is everted into a valgus, externally rotated, position. The head of the talus is palpable on the plantar medial aspect of the midfoot. The Achilles tendon is contracted and the calcaneus is in equinus. The forefoot is dorsiflexed at the midtarsal joints creating a palpable gap dorsally between the navicular and where the talar neck should normally be located. This gap can be helpful in distinguishing congenital vertical talus from the more common calcaneovalgus foot [33]. Upon plantar flexing the congenital vertical talus foot the gap remains and, in a calcaneovalgus foot, the gap disappears as the talonavicular joint reduces in plantar flexion. Left untreated, the foot deformities seen with vertical talus become more rigid and adaptive changes occur in the tarsal bones. With weight-bearing, callosities develop along the medial border of the foot around the head of the talus. The forefoot becomes rigidly abducted and the heel does not touch the ground. Shoewear becomes difficult and pain is inevitable. Because of the high incidence of associated neurologic abnormalities in patients with congenital vertical talus, the neuroaxis should be evaluated in all patients to rule out abnormalities [15].
Fig. 1.
Clinical photographs demonstrating the features of congenital vertical talus. a Bilateral congenital vertical talus deformities in a 6-week-old infant demonstrating the convex plantar surface of the feet. b Deep creases are present on the dorsolateral aspect of the foot in an 8-week-old infant with bilateral congenital vertical talus
There has been several classification schemes proposed for vertical talus based either on anatomical abnormalities or associated diagnoses. Coleman proposed two types of vertical talus, the first with isolated talonavicular dislocation and the second with both talonavicular and calcaneocuboid joint dislocations [34]. Ogata and Schoenecker [5] divided vertical talus into three groups. In group one, which is defined as idiopathic, there are no other associated diagnoses. Group two consists of those vertical talus patients with other congenital anomalies but no neurologic deficits. Group three includes those patients with vertical talus and associated neurologic disorders. Finally, Hamanishi [4] classified vertical talus into five groups based on association with: (1) neural tube defects or spinal anomalies, (2) neuromuscular disorders, (3) malformation syndromes, (4) chromosomal aberrations, and (5) idiopathic. It is likely that a new genetic classification for vertical talus will emerge as our understanding of this disorder evolves.
A less severe variant of vertical talus has been termed the oblique talus. This variant is characterized by the same clinical deformities as seen in vertical talus, but the deformities are less rigid. In particular, the navicular will reduce in plantar flexion in patients with an oblique talus [35, 36], whereas the navicular is rigidly dislocated in patients with vertical talus. This has been an important distinction because the oblique talus can be treated conservatively with observation and/or casting alone.
Radiographic features
Anteroposterior and lateral radiographs of the foot should be taken in the neutral position for infants and standing for those children old enough. The lack of ossification of many of the bones in the foot at birth can make the diagnosis of congenital vertical talus challenging on plain radiographs [37]. The talus, tibia, calcaneus, and metatarsals are ossified at birth. The cuboid ossifies in the first month of life while the cuneiforms and navicular usually ossify around the ages of 2 and 3 years, respectively. Since most children with vertical talus are seen in the newborn period, the radiographic evaluation is focused on the relationships of the ossified talus and calcaneus to the tibia as well as the relationship of the metatarsals to the hindfoot. Measurements that can be obtained on the lateral radiograph include the talocalcaneal, tibiocalcaneal, tibiotalar, and talar axis-first metatarsal base angles. Typical radiographic findings demonstrate the long axis of the talus to be vertical and lying parallel with the longitudinal axis of the tibia on the lateral radiograph. The calcaneus is in significant equinus, and the talocalcaneal angle is increased (Fig. 2). Forced plantar flexion and forced dorsiflexion lateral radiographs are necessary to confirm the diagnosis of vertical talus and rule out the oblique talus and calcaneovalgus foot as diagnoses. The forced plantar flexion lateral radiograph in a vertical talus foot shows persistent malalignment of the long axis of the talus and the first metatarsal while the forced dorsiflexion lateral radiograph demonstrates a persistently decreased tibiocalcaneal angle indicating fixed hindfoot equinus (Fig. 3a, b). In contrast, a forced plantar flexion lateral radiograph of an oblique talus will demonstrate restoration of a normal relationship between the long axis of the talus and the first metatarsal (Fig. 4a, b).
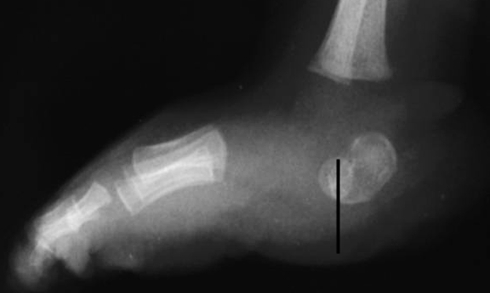
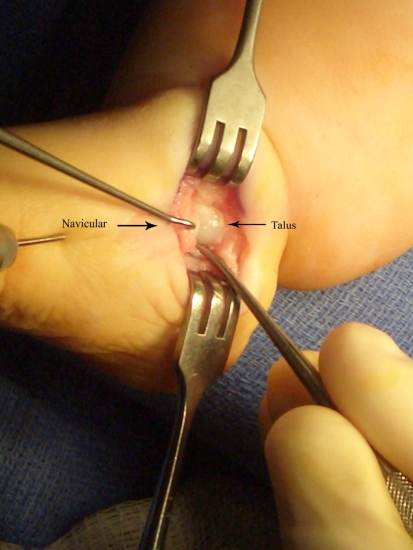
Fig. 2.
Lateral radiograph of the right foot of a 6-week-old boy with congenital vertical talus, showing plantar flexion of both the talus and calcaneus
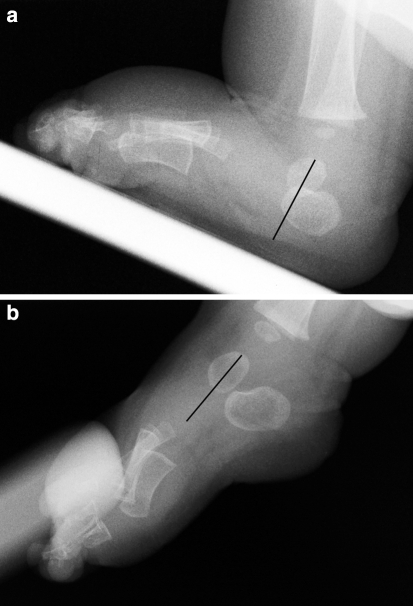
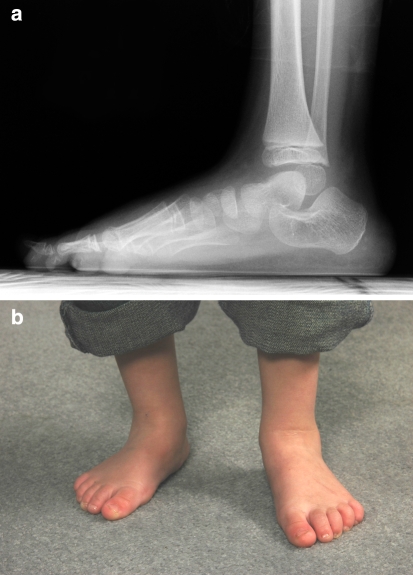
Fig. 3.
a Plantar flexion lateral radiograph of the right foot of a 12-week-old male with congenital vertical talus, showing persistent dorsal translation of the forefoot on the hindfoot. b Lateral dorsiflexion radiograph of the same foot, showing persistent plantar flexion of the talus and calcaneus
Fig. 4.
a Lateral radiograph of a 7-week-old male with an oblique talus, demonstrating vertical position of the talus. b Lateral plantar flexion radiograph, demonstrating restoration of the normal relationship between the longitudinal axis of the talus and the first metatarsal
Differential diagnosis
In the newborn period, a positional calcaneovalgus foot deformity can by commonly mistaken for a vertical talus. In a calcaneovalgus deformity the foot is dorsiflexed to such a degree that the dorsal surface of the foot is touching the anterior surface of the lower leg. There is no equinus contracture of the calcanceus as in a vertical talus deformity and the foot is much more flexible than a vertical talus. In cases in which there is confusion between a vertical talus and a calcaneovalgus foot deformity, a plantar flexion lateral radiograph of the foot is taken to confirm the diagnosis.
Posteromedial bow of the tibia is also seen in the newborn period and presents with a calcaneovalgus foot deformity and a shortened and bowed tibia. This can be differentiated from a vertical talus by careful physical examination and radiographs if necessary. The last condition in infancy that can be confused with a vertical talus is the oblique talus which has been discussed above. A plantar flexion lateral radiograph is often necessary to make the distinction.
Treatment
The goals of treatment are to restore the normal anatomic relationships between the talus, the navicular, and the calcaneus, in order to provide a normal weight distribution through the foot. Treatment of congenital vertical talus, as with clubfoot, begins with serial manipulations and casts. However, unlike casting for clubfoot [38], serial casting for congenital vertical talus has not been used until recently as a method of achieving definitive correction [39]. Instead, cast treatment for congenital vertical talus has been traditionally used as a method of improving the deformity and thereby decreasing the complexity of an inevitable extensive soft-tissue release operation [1, 5, 31, 40].
Traditional surgical treatment
There are multiple surgeries described for the treatment of vertical talus. The type of procedure used for an individual patient is based on the age of the patient, severity of the deformity, and the preference of the surgeon. Children up to the age of 3 years are usually offered an open reduction of the talonavicular joint, which can be performed through either a one-stage or two-stage operation. If a two-stage procedure is chosen, the first stage consists of lengthening the extensor tendons, the tibialis anterior tendon and reduction of the talonavicular joint. The second stage consists of lengthening the peroneal tendons and correcting the equinus contracture through an Achilles tendon lengthening and posterior ankle and subtalar release.
Most surgeons now prefer a one-stage procedure [5, 34, 40–45] because of fewer complications like avascular necrosis of the talus seen with the two-stage procedure [5]. The one-stage correction can be done through a dorsal approach or a posterior approach. Though both approaches have been used with good short-term success, there is some data to link the dorsal approach with shorter operative time, better clinical scores, and fewer complications than the posterior approach [46]. There are three basic components to the one-stage correction. The first step is the reduction of the talonavicular joint which is aided by release of the anterior tibialis tendon and the tibionavicular and talonavicular ligaments. The reduction is held by a Kirschner wire placed across the talonavicular joint (Fig. 5). The second step is lengthening of the toe extensors and peroneals which aids in improving ankle plantar flexion and forefoot adduction. The calcaneocuboid joint is also reduced if necessary. The third step is correction of the ankle equinus contracture which is done by lengthening the Achilles tendon and releasing the ankle and subtalar joint capsules (Fig. 6). Some authors have recommended the addition of a tibialis anterior tendon transfer to the head or neck of the talus at the time of open reduction to add a dynamic corrective force [40–42, 47, 48]. Correction of vertical talus through an open reduction can be associated with significant short-term complications, including wound necrosis [1], undercorrection of the deformity [34], stiffness of the ankle and subtalar joint [49], and the eventual need for multiple operative procedures such as subtalar and triple arthrodesis [47]. Long-term outcomes are likely to be complicated by a significant amount of degenerative arthritis as is seen in many patients with clubfoot treated with extensive soft-tissue releases [50].
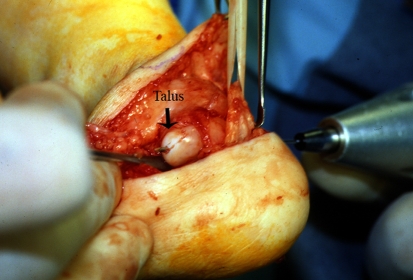
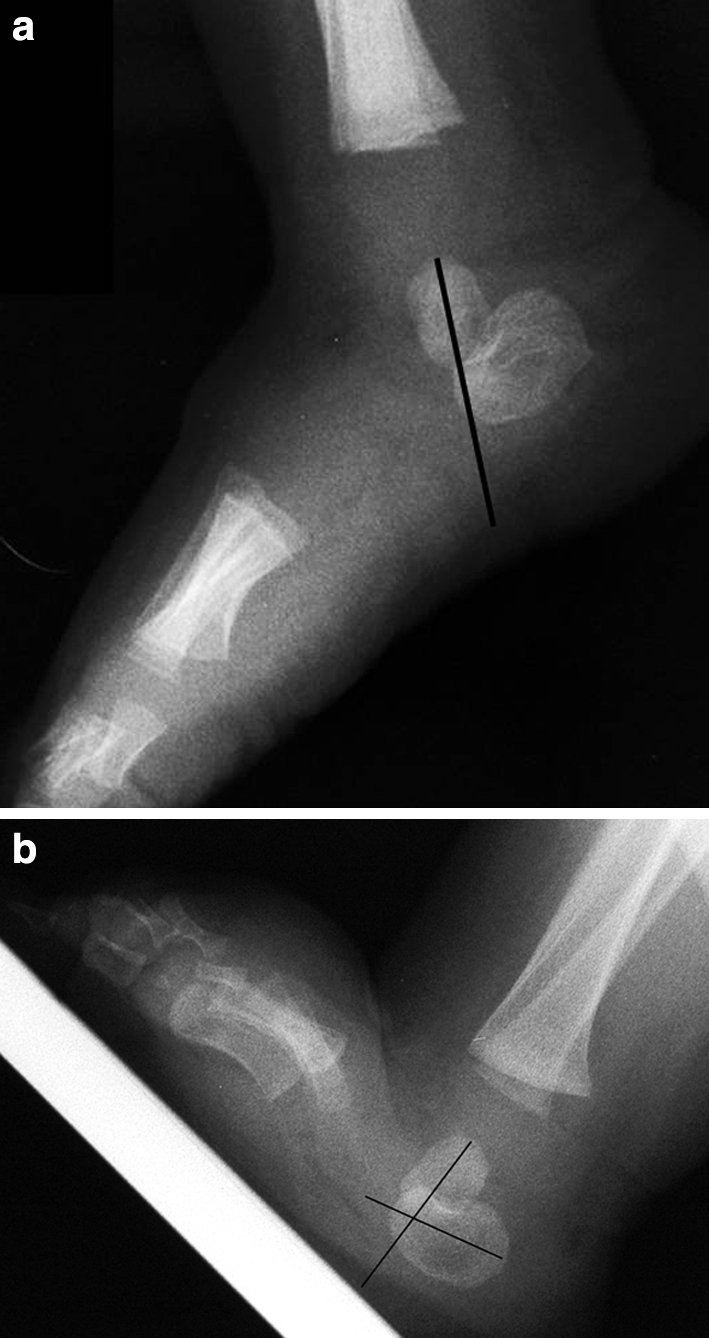
Fig. 5.
Intraoperative photograph illustrating Kirschner wire placed antegrade through the talus to aid in reduction of the talonavicular joint during a one-stage reduction procedure (Courtesy of Perry L. Schoenecker)
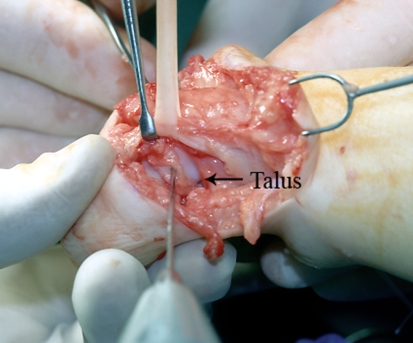
Fig. 6.
Intraoperative photograph illustrating a posterior ankle and subtalar release performed on the same patient in Fig. 5 during a one-stage reduction of a vertical talus (Courtesy of Perry L. Schoenecker)
The exact upper age limit for a successful open reduction is not known. Some children after the age of 3 years require excision of the navicular at the time of open reduction [51, 52]. There is also concern that, after the age of 3 years, an untreated vertical talus results in permanent deformity in the anterior and middle subtalar facets. If there is not sufficient remodeling potential of the articular surfaces present after an open reduction of the talonavicular joint then a medial column shortening and lateral column lengthening procedure may be necessary. Children between the ages of 4 and 8 years with either a primary or a recurrent deformity can be treated with open reduction combined with extraarticular arthrodesis [34, 47]. Those patients that are older than 8 years often require a triple arthrodesis [48]. However, arthrodesis does result in painful degenerative arthritis of the ankle and midtarsal joints when the patients are followed long-term [53–60].
Serial casting and minimal surgical intervention
The use of serial manipulation and plaster cast treatment followed by minimal surgical interventions has provided good early results in the treatment of idiopathic congenital vertical talus [39]. This method can also be applied to vertical talus associated with genetic syndromes and neuromuscular conditions with similar success. The method of cast correction of a vertical talus is based on a specific way of manipulating the foot so as to gradually reduce the talonavicular joint. The principles are similar to those used in the Ponseti method of clubfoot correction [61]. The concept of this method is simple, but attention to detail is critical during casting, surgery, and bracing periods to ensure a complete reduction of the talonavicular joint is both achieved and maintained.
Treatment is initiated if possible in the first few weeks of life. As with the Ponseti method of clubfoot correction [61], treatment begins with weekly manipulations and casts, but with the forces applied in the opposite direction. The casting is performed in the outpatient clinic. All components of the deformity are corrected simultaneously with the exception of the hindfoot equinus, which is corrected last. The manipulation consists of stretching the foot into plantar flexion and inversion with one hand while counterpressure is applied with the thumb of the opposite hand to the medial aspect of the head of the talus (Fig. 7a, b). After a few minutes of gentle manipulations a long-leg plaster cast is applied to hold the foot in the desired amount of correction. The cast is applied in two sections to allow the orthopaedic surgeon to focus attention on the molding of the foot and ankle. The details of the plaster cast application are reviewed in a published manuscript [62]. In brief, the first section applied is the short-leg cast which extends from the tip of the toes to just below the knee. Care is taken to mold underneath the head of the talus and around the malleoli. The foot should be held in the desired position as the cast is applied and not manipulated after the plaster is rolled. This avoids pressure sores and a poor-fitting cast. Once the plaster has set, the cast is extended above the knee, with the knee in 90° of flexion. Four to six plaster casts changed weekly is usually enough to achieve reduction of the talonavicular joint. The position of the foot in the final cast used to achieve reduction of the talonavicular joint should be in maximum plantar flexion and inversion to ensure adequate stretching of the contracted dorsolateral tendons and soft tissues. The foot in this extreme position simulates the position of a clubfoot. A lateral foot radiograph should be taken in this cast to ensure reduction of the talonavicular joint. Since the navicular is not ossified in infants, reduction is confirmed indirectly by the talar axis-first metatarsal base angle as measured on the lateral foot radiograph.
Fig. 7.
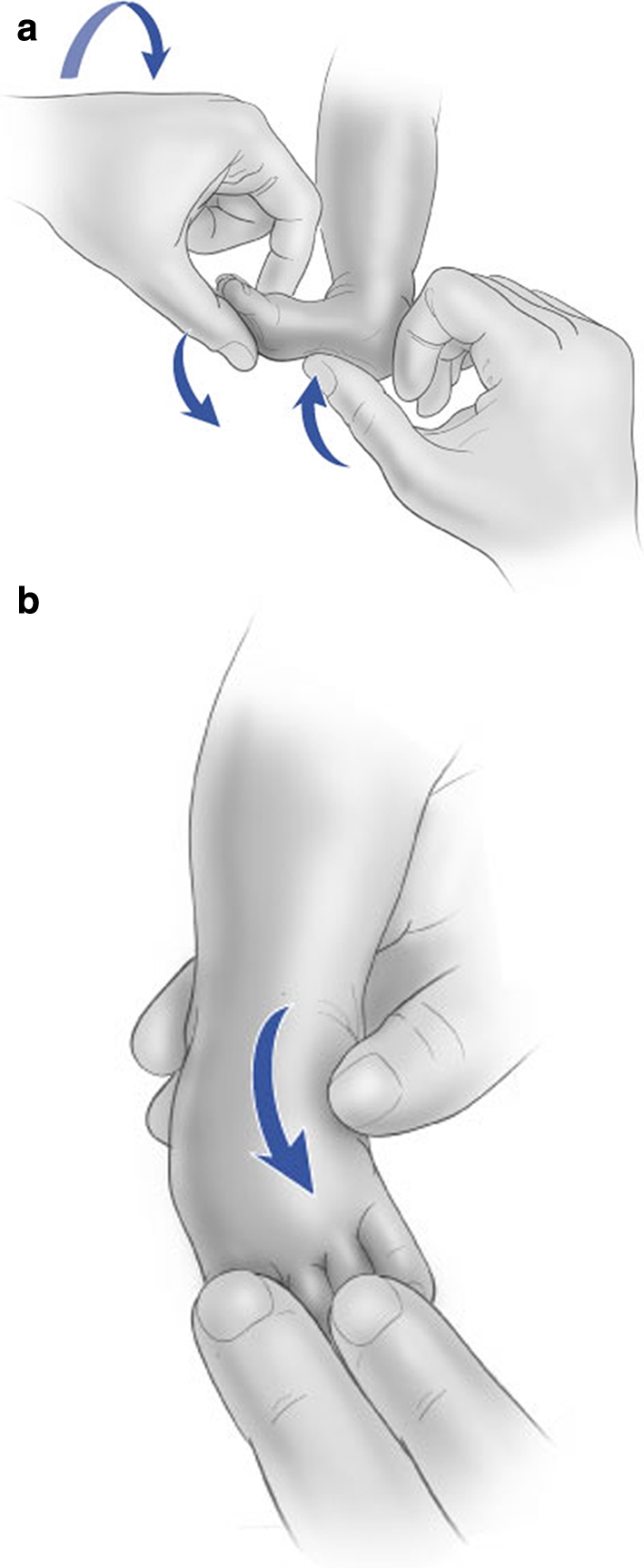
Illustrations of the direction of the forces applied to reduce a vertical talus deformity. The foot is stretched into plantar flexion and inversion while counterpressure is applied with the thumb to the medial aspect of the head of the talus. Reprinted with permission from The Journal of Bone and Joint Surger, Inc (J Bone Joint Surg Am. (2007) 89:Pt 1 Suppl 2:111–121)
If the talonavicular joint is reduced on the lateral foot radiograph the patient is then scheduled for surgery for percutaneous fixation of the talonavicular joint and a percutaneous Achilles tendon tenotomy. In the operating room, the foot is held in plantarflexion and inversion to keep the talonavicular joint reduced and a Kirschner wire is placed retrograde from the navicular into the talus. The wire is cut and left buried underneath the skin to prevent the wire from backing out. The ability to successfully place the Kirschner wire is based on the surgeon’s skill at palpating the talus and navicular. Radiographs can serve as an aid in assessing the reduction of the talonavicular joint indirectly but cannot be used to visualize the navicular itself.
If the talonavicular joint is not reduced completely with casting then a small, 2-cm medial incision is made over the talonavicular joint in the operating room (Fig. 8). The talonavicular joint capsule is open as well as the medial subtalar joint. An elevator is then used to gently lift the talus completing the reduction (Fig. 9). With the talus held in the reduced position, a Kirschner wire is then placed in a retrograde manner across the talonavicular joint (Fig. 10). For patients who are older than 2 years at the time of open reduction of the talonavicular joint, the tibialis anterior tendon is also transferred to the dorsal aspect of the neck of the talus to provide a dynamic corrective force.
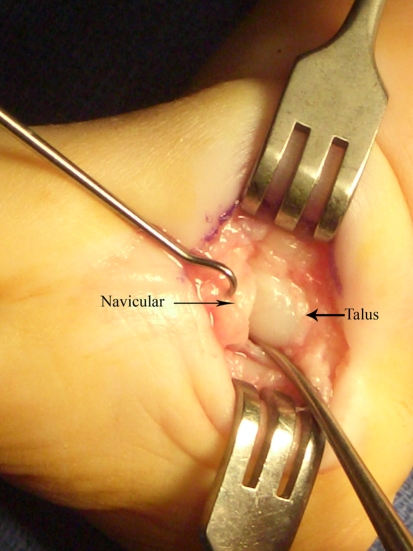
Fig. 8.
Clinical photograph demonstrating the location of the incision over the medial aspect of the talonavicular joint, used for open reduction of the talonavicular joint
Fig. 9.
Intraoperative photograph demonstrating a single-prong skin hook placed on the navicular and a Freer elevator in the medial subtalar joint being used to reduce the talus to a horizontal position in relation to the navicular
Fig. 10.
Intraoperative photograph demonstrating Kirschner wire fixation of the reduced talonavicular joint
Once the talonavicular joint is reduced and stabilized with the Kirschner wire, a percutaneous tenotomy of the Achilles tendon is used to correct the residual equinus deformity. This is a complete release of the tendon and is done 1 cm proximal to the Achilles tendon insertion into the calcaneus. An assessment is made of the ankle plantar flexion and forefoot passive adduction at this point. If plantar flexion is limited to <25°, a fractional lengthening of the extensor digitorum communis is done at the level of the musculotendinous junction. If passive forefoot adduction is <10°, fractional lengthening of the peroneal brevis tendon is performed at the musculotendinous junction. Lengthening of the peroneal brevis and extensor digitorum communis is not often needed since the preoperative casting usually stretches these structures enough. A long leg cast is applied with the foot in neutral and the ankle in 5° of dorsiflexion. The cast is changed in the clinic in 2 weeks, at which time a mold is made for a night-time brace that has been described for the use in clubfoot treatment after cast correction with the Ponseti method [63]. The brace consists of an articulating bar that allows for independent leg movement. Attached to the bar are custom-molded orthoses that are placed in neutral position as opposed to external rotation when treating clubfeet. This allows for an adduction stretch on the foot while in the brace. A new long leg cast is then applied with the ankle in 10°–15° of dorsiflexion and is worn for 3 weeks. The cast is once again changed in the clinic to a new long leg cast with the ankle in neutral that is worn for an additional 3 weeks. This final cast is removed in the operating room to allow for Kirschner pin removal as well.
The patients then initiate the night-time brace wear, and the parents are instructed on range-of-motion exercises for the ankle and foot to prevent recurrence. The exercises emphasize ankle plantar flexion and foot inversion. The patients are seen every 3 months after initiating brace wear until the age of 2 years and then every 6 months–1 year until the age of 7 years (Fig. 10). After the age of 7 years, the patients are seen once every 2 years until skeletal maturity is reached. The authors are hopeful that this approach of less invasive surgery to correct the vertical talus will lead to a more flexible and less painful foot long-term as has been seen with Ponseti method of clubfoot correction [64].
Fig. 11.
Lateral radiograph and clinical picture of the same child illustrated in Fig. 3a, b at the age of 5 years after treatment with cast correction, percutaneous Kirschner wire fixation, and percutaneous Achilles tendon tenotomy for congenital vertical talus of the right foot
Acknowledgments
M.B.D. is supported by a grant from the Shriners Hospital for Children and the Saint Louis Children’s Hospital Foundation.
References
- 1.Jacobsen ST, Crawford AH (1983) Congenital vertical talus. J Pediatr Orthop 3:306–310 [DOI] [PubMed]
- 2.Lamy L, Weissman L (1939) Congenital convex pes valgus. J Bone Joint Surg Am 21:79
- 3.Dodge LD, Ashley RK, Gilbert RJ (1987) Treatment of the congenital vertical talus: a retrospective review of 36 feet with long-term follow-up. Foot Ankle 7:326–332 [DOI] [PubMed]
- 4.Hamanishi C (1984) Congenital vertical talus: classification with 69 cases and new measurement system. J Pediatr Orthop 4:318–326 [PubMed]
- 5.Ogata K, Schoenecker PL, Sheridan J (1979) Congenital vertical talus and its familial occurrence: an analysis of 36 patients. Clin Orthop 139:128–132 [PubMed]
- 6.Lloyd-Roberts GC, Spence AJ (1958) Congenital vertical talus. J Bone Joint Surg Br 40-B:33–41 [DOI] [PubMed]
- 7.da Paz AC Jr, de Souza V, de Souza DC (1978) Congenital convex pes valgus. Orthop Clin N Am 9:207–218 [PubMed]
- 8.Wirth T, Schuler P, Griss P (1994) Early surgical treatment for congenital vertical talus. Arch Orthop Trauma Surg 113:248–253 [DOI] [PubMed]
- 9.Sharrard WJ, Grosfield I (1968) The management of deformity and paralysis of the foot in myelomeningocele. J Bone Joint Surg Br 50:456–465 [PubMed]
- 10.Townes PL, Dehart GK Jr, Hecht F, Manning JA (1962) Trisomy 13–15 in a male infant. J Pediatr 60:528–532 [DOI] [PubMed]
- 11.Uchida IA, Lewis AJ, Bowman JM, Wang HC (1962) A case of double trisomy:trisomy no. 18 and triplo-X. J Pediatr 60:498–502 [DOI] [PubMed]
- 12.Stern HJ, Clark RD, Stroberg AJ, Shohat M (1989) Autosomal dominant transmission of isolated congenital vertical talus. Clin Genet 36:427–430 [PubMed]
- 13.Dobbs MB, Schoenecker PL, Gordon JE (2002) Autosomal dominant transmission of isolated congenital vertical talus. Iowa Orthop J 22:25–27 [PMC free article] [PubMed]
- 14.Dobbs MB, Gurnett CA, Pierce B, Exner GU, Robarge J, Morcuende JA, Cole WG, Templeton PA, Foster B, Bowcock AM (2006) HOXD10 M319K mutation in a family with isolated congenital vertical talus. J Orthop Res 24:448–453 [DOI] [PubMed]
- 15.Drennan JC, Sharrard WJ (1971) The pathological anatomy of convex pes valgus. J Bone Joint Surg Br 53:455–461 [PubMed]
- 16.Stanton RP, Rao N, Scott CI Jr (1994) Orthopaedic manifestations in de Barsy syndrome. J Pediatr Orthop 14:60–62 [DOI] [PubMed]
- 17.Green NE, Lowery ER, Thomas R (1993) Orthopaedic aspects of prune belly syndrome. J Pediatr Orthop 13:496–501 [DOI] [PubMed]
- 18.Yassir WK, Grottkau BE, Goldberg MJ (2003) Costello syndrome: orthopaedic manifestations and functional health. J Pediatr Orthop 23:94–98 [DOI] [PubMed]
- 19.Julia S, Pedespan JM, Boudard P, Barbier R, Gavilan-Cellie I, Chateil JF, Lacombe D (2002) Association of external auditory canal atresia, vertical talus, and hypertelorism: confirmation of Rasmussen syndrome. Am J Med Genet 110:179–181 [DOI] [PubMed]
- 20.Haberlandt E, Loffler J, Hirst-Stadlmann A, Stockl B, Judmaier W, Fischer H, Heinz-Erian P, Muller T, Utermann G, Smith RJ, Janecke AR (2001) Split hand/split foot malformation associated with sensorineural deafness, inner and middle ear malformation, hypodontia, congenital vertical talus, and deletion of eight microsatellite markers in 7q21.1–q21.3. J Med Genet 38:405–409 [DOI] [PMC free article] [PubMed]
- 21.Muragaki Y, Mundlos S, Upton J, Olsen BR (1996) Altered growth and branching patterns in synpolydactyly caused by mutations in HOXD13. Science 272:548–551 [DOI] [PubMed]
- 22.Thompson AA, Nguyen LT (2000) Amegakaryocytic thrombocytopenia and radio-ulnar synostosis are associated with HOXA11 mutation. Nat Genet 26:397–398 [DOI] [PubMed]
- 23.Mortlock DP, Innis JW (1997) Mutation of HOXA13 in hand–foot–genital syndrome. Nat Genet 15:179–180 [DOI] [PubMed]
- 24.Shrimpton AE, Levinsohn EM, Yozawitz JM, Packard DS Jr, Cady RB, Middleton FA, Persico AM, Hootnick DR (2004) A HOX gene mutation in a family with isolated congenital vertical talus and Charcot–Marie-tooth disease. Am J Hum Genet 75:92–96 [DOI] [PMC free article] [PubMed]
- 25.Gurnett CA, Keppel C, Bick J, Bowcock AM, Dobbs MB (2007) Absence of HOXD10 mutations in idiopathic clubfoot and sporadic vertical talus. Clin Orthop Relat Res (in press) [DOI] [PubMed]
- 26.Faiyaz-Ul-Haque M, Ahmad W, Wahab A, Haque S, Azim AC, Zaidi SH, Teebi AS, Ahmad M, Cohn DH, Siddique T, Tsui LC (2002) Frameshift mutation in the cartilage-derived morphogenetic protein 1 (CDMP1) gene and severe acromesomelic chondrodysplasia resembling Grebe-type chondrodysplasia. Am J Med Genet 111:31–37 [DOI] [PubMed]
- 27.Faiyaz-Ul-Haque M, Ahmad W, Zaidi SH, Haque S, Teebi AS, Ahmad M, Cohn DH, Tsui LC (2002) Mutation in the cartilage-derived morphogenetic protein-1 (CDMP1) gene in a kindred affected with fibular hypoplasia and complex brachydactyly (DuPan syndrome). Clin Genet 61:454–458 [DOI] [PubMed]
- 28.Thomas JT, Kilpatrick MW, Lin K, Erlacher L, Lembessis P, Costa T, Tsipouras P, Luyten FP (1997) Disruption of human limb morphogenesis by a dominant negative mutation in CDMP1. Nat Genet 17:58–64 [DOI] [PubMed]
- 29.Polinkovsky A, Robin NH, Thomas JT, Irons M, Lynn A, Goodman FR, Reardon W, Kant SG, Brunner HG, van der Burgt I, Chitayat D, McGaughran J, Donnai D, Luyten FP, Warman ML (1997) Mutations in CDMP1 cause autosomal dominant brachydactyly type C. Nat Genet 17:18–19 [DOI] [PubMed]
- 30.Patterson WR, Fitz DA, Smith WS (1968) The pathologic anatomy of congenital convex pes valgus. Post mortem study of a newborn infant with bilateral involvement. J Bone Joint Surg Am 50:458–466 [DOI] [PubMed]
- 31.Seimon LP (1987) Surgical correction of congenital vertical talus under the age of 2 years. J Pediatr Orthop 7:405–411 [DOI] [PubMed]
- 32.Specht EE (1975) Congenital paralytic vertical talus. An anatomical study. J Bone Joint Surg Am 57:842–847 [PubMed]
- 33.Harrold AJ (1967) Congenital vertical talus in infancy. J Bone Joint Surg Br 49:634–643 [PubMed]
- 34.Coleman SS, Stelling FH 3rd, Jarrett J (1970) Pathomechanics and treatment of congenital vertical talus. Clin Orthop 70:62–72 [PubMed]
- 35.Gould N, Moreland M, Alvarez R, Trevino S, Fenwick J (1989) Development of the child’s arch. Foot Ankle 9:241–245 [DOI] [PubMed]
- 36.Kumar SJ, Cowell HR, Ramsey PL (1982) Vertical and oblique talus. Instr Course Lect 31:235–251 [PubMed]
- 37.Shapiro F, Glimcher MJ (1979) Gross and histological abnormalities of the talus in congenital club foot. J Bone Joint Surg Am 61:522–530 [PubMed]
- 38.Ponseti IV (1992) Treatment of congenital club foot. J Bone Joint Surg Am 74:448–454 [PubMed]
- 39.Dobbs MB, Purcell DB, Nunley R, Morcuende JA (2006) Early results of a new method of treatment for idiopathic congenital vertical talus. J Bone Joint Surg Am 88:1192–1200 [DOI] [PubMed]
- 40.Drennan JC (1996) Congenital vertical talus. Instr Course Lect 45:315–322 [PubMed]
- 41.Duncan RD, Fixsen JA (1999) Congenital convex pes valgus. J Bone Joint Surg Br 81:250–254 [DOI] [PubMed]
- 42.Kodros SA, Dias LS (1999) Single-stage surgical correction of congenital vertical talus. J Pediatr Orthop 19:42–48 [DOI] [PubMed]
- 43.Oppenheim W, Smith C, Christie W (1985) Congenital vertical talus. Foot Ankle 5:198–204 [DOI] [PubMed]
- 44.Stricker SJ, Rosen E (1997) Early one-stage reconstruction of congenital vertical talus. Foot Ankle Int 18:535–543 [DOI] [PubMed]
- 45.Walker AP, Ghali NN, Silk FF (1985) Congenital vertical talus. The results of staged operative reduction. J Bone Joint Surg Br 67:117–121 [DOI] [PubMed]
- 46.Mazzocca AD, Thomson JD, Deluca PA, Romness MJ (2001) Comparison of the posterior approach versus the dorsal approach in the treatment of congenital vertical talus. J Pediatr Orthop 21:212–217 [DOI] [PubMed]
- 47.Grice DS (1952) An extra-articular arthrodesis of the subastragalar joint for correction of paralytic flat feet in children. J Bone Joint Surg Am 34 A:927–940 passim [PubMed]
- 48.Grice DS (1955) Further experience with extra-articular arthrodesis of the subtalar joint. J Bone Joint Surg Am 37-A:246–259 passim [PubMed]
- 49.Zorer G, Bagatur AE, Dogan A (2002) Single stage surgical correction of congenital vertical talus by complete subtalar release and peritalar reduction by using the Cincinnati incision. J Pediatr Orthop B 11:60–67 [DOI] [PubMed]
- 50.Dobbs MB, Nunley R, Schoenecker PL (2006) Long-term follow-up of patients with clubfeet treated with extensive soft-tissue release. J Bone Joint Surg Am 88:986–996 [DOI] [PubMed]
- 51.Colton CL (1973) The surgical management of congenital vertical talus. J Bone Joint Surg Br 55:566–574 [PubMed]
- 52.Clark MW, D’Ambrosia RD, Ferguson AB (1977) Congenital vertical talus: treatment by open reduction and navicular excision. J Bone Joint Surg Am 59:816–824 [PubMed]
- 53.Adelaar RS, Dannelly EA, Meunier PA, Stelling FH, Goldner JL, Colvard DF (1976) A long term study of triple arthrodesis in children. Orthop Clin North Am 7:895–908 [PubMed]
- 54.Angus PD, Cowell HR (1986) Triple arthrodesis. A critical long-term review. J Bone Joint Surg Br 68:260–265 [DOI] [PubMed]
- 55.Drew AJ (1951) The late results of arthrodesis of the foot. J Bone Joint Surg Br 33-B:496–502 [DOI] [PubMed]
- 56.McCall RE, Lillich JS, Harris JR, Johnston FA (1985) The Grice extraarticular subtalar arthrodesis: a clinical review. J Pediatr Orthop 5:442–445 [DOI] [PubMed]
- 57.Ross PM, Lyne ED (1980) The Grice procedure: indications and evaluation of long-term results. Clin Orthop Relat Res 194–200 [PubMed]
- 58.Scott SM, Janes PC, Stevens PM (1988) Grice subtalar arthrodesis followed to skeletal maturity. J Pediatr Orthop 8:176–183 [PubMed]
- 59.Smith JB, Westin GW (1968) Subtalar extra-articular arthrodesis. J Bone Joint Surg Am 50:1027–1035 [PubMed]
- 60.Southwell RB, Sherman FC (1981) Triple arthrodesis: a long-term study with force plate analysis. Foot Ankle 2:15–24 [DOI] [PubMed]
- 61.Laaveg SJ, Ponseti IV (1980) Long-term results of treatment of congenital club foot. J Bone Joint Surg Am 62:23–31 [PubMed]
- 62.Dobbs MB, Purcell DB, Nunley R, Morcuende JA (2007) Early results of a new method of treatment for idiopathic congenital vertical talus. Surgical technique. J Bone Joint Surg Am 89 Pt 1(Suppl 2):111–121 [DOI] [PubMed]
- 63.Chen R, Gordon JE, Luhmann SJ, Schoenecker PL, Dobbs MB (2007) A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop 27:522–528 [DOI] [PubMed]
- 64.Cooper DM, Dietz FR (1995) Treatment of idiopathic clubfoot. A thirty-year follow-up note. J Bone Joint Surg Am 77:1477–1489 [DOI] [PubMed]