Abstract
Purpose
A recent study reported a higher incidence of pre-operative ulnar nerve symptoms in patients with flexion-type supracondylar fractures than in those with the more common extension supracondylar fractures and a greater need for open reduction (Kocher in POSNA paper #49 2006). We have encountered a specific pattern of flexion supracondylar fractures that often require open reduction with internal fixation (ORIF) due to entrapment of the ulnar nerve within the fracture.
Methods
Medical records and X-rays from 1997 to 2005 at our children’s hospital were examined to identify flexion supracondylar fractures that required open reduction. The operative reports were reviewed to identify cases that had the ulnar nerve blocking the reduction.
Results
During the 8 years examined, 1,650 supracondylar fractures had been treated by means of closed reduction and percutaneous pinning. Of these, only 1.8% or 30 cases could not be reduced closed and required open reduction internal fixation, excluding 11 open fractures. Of the 30 fractures requiring open reduction internal fixation, 24 were of the extension type needing ORIF because of interposed periosteum/muscle. The other 6 patients had flexion-type supracondylar fractures that failed closed reduction. All had a persistent medial gap at the fracture site. All 6 fractures had interposed periosteum or muscle, while in 3 cases the ulnar nerve was also entrapped within the fracture site (Figs. 1, 2)
Conclusion
Flexion-type supracondylar fractures remain a relatively uncommon variant (2–3%) of supracondylar fractures. Recent reports have noted that open treatment of these fractures is required more frequently than for extension fractures. In our series, 20% of the open cases were flexion-type fractures and in half of these the ulnar nerve was found to be entrapped in the fracture, preventing reduction.
Keywords: Supracondylar fractures, Ulnar nerve, Flexion-type supracondylar
Introduction
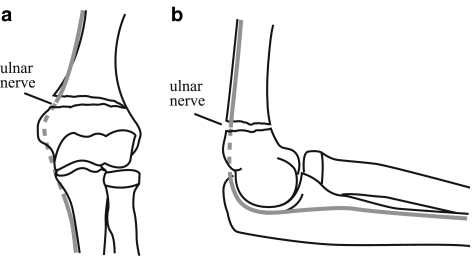
Flexion-type supracondylar fractures are uncommon in children, accounting for only 2–10% of all distal humerus supracondylar fractures [1–6]. They are usually caused by a direct fall on the posterior aspect of the elbow, resulting in a reverse angulation of that seen in the more common extension-type supracondylar fracture [5]. A greater need for open reduction internal fixation (ORIF) of these fractures has been noted as well as a higher incidence of ulnar nerve injury [2–5]. This is seen particularly with displaced type-III fractures (as classified by the modified Gartland classification system by Wilkins) [5], in which there is anterosuperior displacement of the distal fragment. The ulnar nerve injury is thought to be the result of the nerve being stretched over the posterior spike of the proximal fragment [5]. We report on a particular fracture pattern of flexion-type supracondylar fractures in which the ulnar nerve is frequently entrapped in the fracture site. The interposed nerve blocks an anatomic closed reduction and, in such a case, led the surgeons to perform ORIF. The purpose of this study was to review flexion-type supracondylar fractures that required ORIF and to determine the features of the fracture that may indicate the potential for ulnar nerve entrapment (Figs. 1, 2).
Fig. 1.
Breakdown of supracondylar fractures requiring open treatment
Fig. 2.
Type-II flexion supracondylar fracture in 5-year-old female (case 2). The patient required open reduction through medial approach, removal of the ulnar nerve from the fracture site and pinning. a AP view of fracture with medial gap prior to reduction. b Lateral view of fracture prior to reduction
Materials and methods
Patients with flexion-type supracondylar fractures who underwent ORIF between 1997 and 2005 were identified through an extensive medical record search from both the medical proactive billing system and our children’s hospital medical records' system. The total number of operative cases of supracondylar fracture treatment were separated into those treated with closed reduction and percutaneous pinning (CRPP) and those having an ORIF. Those records indicating an ORIF were reviewed to identify the subset of cases that were of the flexion-type fracture pattern. The records of the initial assessment, operative reports as well as pre- and post-operative radiographs were reviewed. Data regarding patient age, gender, pre- and post-operative examination and fracture pattern were collected. The operative findings and reason for performing an ORIF (as opposed to our standard CRPP) were gleaned from the operative record.
Results
During the 8-year period, 1,650 supracondylar fractures had been treated operatively, with the vast majority receiving a CRPP (Fig. 1). All reductions were performed by senior members of the Pediatric Orthopaedic Society of North America (POSNA) in the operating room. Axial traction and flexion was used to reduce extension supracondylar fractures [5], and axial traction with extension was used to reduce flexion supracondylar fractures as outlined by Williamson [6]. During this time, 41 supracondylar fractures required ORIF. Of these, 35 were of the extension type and 6 the flexion type. Of the extension injuries, 31% (11) were open fractures requiring irrigation and debridement followed by pinning. The remaining 24 extension-type fractures failed attempts at closed reduction and were subsequently opened. Causes of failure of closed reduction included 7 (29%) with severe comminution and 17 with interposed periosteum/ muscle (71%)—of which five had pre-operative nerve palsies involving the median/anterior interosseus nerve, although at time of treatment none was found to have nerve entrapment or laceration. Only one extension-type fracture (3%) was found to have the ulnar nerve entrapped in the fracture preventing reduction, and this patient did not have pre-operative ulnar nerve palsy. Of the flexion-type fractures, there were 4 female and 2 male patients, with average age of 7 years (5–10 years), and one had pre-operative ulnar nerve palsy (Table 1). All had failed closed reduction attempts and a persistent medial gap at the fracture site was noted radiographically (Fig. 2). In 2 of the cases, the medial soft tissues of the elbow had a puckering that suggested soft tissue entrapment. When the fracture sites were opened, 2 were found to have interposed periosteum, 1 had severe comminution and 3 (50%) had the ulnar nerve entrapped in the fracture site preventing reduction (Fig. 3). These patients were followed for an average of 13 weeks (range 6–36 weeks) with acceptable alignment, full range of motion, evidence of clinical and radiologic healing and resolution of the single ulnar nerve neuropathy at final follow-up.
Table 1.
Patient demographics
| Patient | Age (years) | Sex | Fracture type | Pre-operative exam | Operative findings |
|---|---|---|---|---|---|
| 1. | 8 | Female | Flexion type II | Ulnar neuropathy | Ulnar nerve entrapped in fracture site |
| 2. | 5 | Female | Flexion type II | Neuro intact | Ulnar nerve entrapped in fracture site |
| 3. | 5 | Male | Flexion type II | Neuro intact | Periosteum/fat in fracture site |
| 4. | 7 | Male | Flexion type III | Neuro intact | Ulnar nerve entrapped in fracture site |
| 5. | 10 | Female | Flexion type II | Neuro intact | Unstable fracture |
| 6. | 9 | Female | Flexion type III | Neuro intact | Periosteum in fracture site |
Fig. 3.
Type-II flexion supracondylar fracture in 8-year-old female (case 1). a AP view of fracture with medial gap. b Lateral view of fracture. c AP view of fracture after closed reduction attempt. d AP view after open reduction and pinning with closure of medial gap. The ulnar nerve was entrapped in the fracture site. e Lateral view after open reduction and pinning
Discussion
Flexion-type supracondylar fractures remain a relatively uncommon variant of childhood supracondylar fractures (2–10% of supracondylar fractures) but represent a difficult group to treat. Many methods of treatment exist including: closed reduction with casting in flexion, closed reduction with casting in extension, traction, closed reduction percutaneous pinning and ORIF [1, 3, 5, 6]. It is recommended that type-I minimally displaced fractures be casted with or without an attempt at reduction. For type-II and -III fractures, closed-reduction percutaneous pinning is recommended [3, 5]. There has been a greater need for ORIF of these flexion-type supracondylar fractures as well as a higher rate of injury to the ulnar nerve than observed with the extension-type fracture pattern [2, 3, 5].
Fowles et al. reported a 9.7% incidence of flexion supracondylar fractures in their series of supracondylar humerus fractures. Displaced type-III fractures accounted for 11 of 17 (65%) of their flexion fractures and 3 of these 17 (17.6%) had ulnar nerve injuries. In these 3 cases, the nerve was found to be draped over the proximal fragment spike. No other nerve injuries were reported for the flexion type and all were associated with radial displacement of the distal fragment. This compares to a rate of only 1% ulnar nerve injuries in those with an extension-type fracture.
Kocher et al. [3] recently reported a 3% incidence of flexion-type supracondylar fractures. They found a greater need for ORIF with flexion (29%) than with extension-type fracture (10%). In his study, pre-operative nerve symptoms were also more common in the flexion type (18%) than in extension type (14%), with almost all occurring in the ulnar nerve.
These results are similar to ours. Although we do not report the incidence of our flexion-type fractures in the 1,650 cases, assuming a rate of 2–10% as previously stated, we have also found a greater need for open flexion supracondylar fractures. Overall, we only opened 1.8% (30 of 1,650) of our supracondylar fractures and 20% (6) of these were flexion type. All 6 of the patients in this series had nearly identical radiographic findings: flexion supracondylar fracture, sagittal view and medial gap on coronal view (Fig. 3). All were noted to have a persisted medial gap on intra-operative imaging after attempted closed reduction. Upon opening, the ulnar nerve was found to be entrapped in the fracture site blocking reduction in half of the cases. This high incidence of ulnar nerve entrapment is likely to be secondary to the ulnar nerve being tethered distal to the fracture within the cubital tunnel of the distal humerus by Osborne’s fascia and to the proximal forearm by flexor carpi ulnaris fascia. As the distal fragment is displaced anteriorly and radially, the ulnar nerve is then pulled into the fracture site posterior to the medial spike of the proximal fragment. This results in the ulnar nerve being entrapped medially and preventing reduction, as identified by the persistent medial gap seen in all our cases that required open treatment (Fig. 4).
Fig. 4.
Depiction of path of ulnar nerve when entrapped in fracture site and triad of findings. a Medial gap on coronal view with ulnar nerve in fracture site (50%). b Flexion supracondylar fracture on sagittal view
In summary, flexion-type supracondylar fractures represent an uncommon but often difficult-to-treat group of fractures. There is an increased likelihood for open reduction because of soft tissue interposition in the fracture site. Ulnar nerve entrapment must be considered with any flexion-type supracondylar fractures that have pre-operative ulnar nerve symptoms and/or a persistent medial gap in the fracture after attempts at closed reduction. When this medial gap is noted, ORIF is likely needed through a medial approach so that the ulnar nerve and soft tissue may be freed and an anatomic reduction achieved. The ulnar nerve appears to be at high risk with flexion-type supracondylar humerus fractures and in half of the cases was found within the fracture site.
Footnotes
Study conducted at Rady Children’s Hospital and Health Center. No financial support was received for this project.
References
- 1.DeBoek H (2001) Flexion-type supracondylar elbow fractures in children. J Pediatr Orthop 21:460–463 [DOI] [PubMed]
- 2.Fowles JV, Kassab MT (1974) Displaced supracondylar fractures of the elbow in children. J Bone Joint Surg Br 56(3):490–500 [PubMed]
- 3.Mahan ST, May CD, Kocher MS (2006) Operative management of displaced flexion supracondylar humerus fractures in children. J Pediatr Orthop 27(5):551–556 [DOI] [PubMed]
- 4.Louahem DM, Nebunescu A, Canavese F, Dimeglio A (2006) Neurovascular complications and severe displacement in supracondylar humerus fractures in children: defensive or offensive strategy? J Pediatr Orthop B 15(1):51–57 [DOI] [PubMed]
- 5.Wilkins KE (1996) Upper extremity: supracondylar fractures of the distal humerus. In: Rockwood CA, Wilkins KE, Beaty JH (eds) Fractures in children, 4th edn. Lippincott-Raven, Philadelphia 669–752
- 6.Williamson DM, Cole WG (1991) Flexion supracondylar fractures of the humerus in children: treatment by manipulation and extension cast. Injury 22(6):451–455 [DOI] [PubMed]