Abstract
Purpose
To evaluate the safety and efficacy of halo immobilization in children younger than 3 years.
Methods
All children less than 3 years of age who were placed in a halo-orthosis at a tertiary pediatric center were reviewed to determine the indications, safety, and efficacy of this method. Adequacy of immobilization and correct technique was established considering the chronology of maturation (skull and brain development). The functional outcome was analyzed.
Results
Ten patients (<3 years old) were identified from a total of 150 where halo ring/vest immobilization was used. There were six boys and four girls, with an average age of 2 years (range 10 months to 2 years and 10 months). The average time of immobilization in the halo-orthosis was 75 days (range 33–168 days), and the average follow-up time was 5 years and 2 months (range 1–12 years). There were two halo-related problems and four related to the index procedure. Halo-related problems included pin-site infection in one patient, and three pins loosening in another. There were four complications associated with the index procedure, all early in the series, including three cases of pseudarthrosis and one patient that had an insufficient decompression of basilar invagination. Two of the three failed fusions occurred at the occipito-cervical junction, which prompted us to develop new techniques for fusion at this level.
Conclusions
Halo-orthosis is a relatively safe and reliable device for immobilization of the upper cervical spine in children less than 3 years old. Understanding the developmental anatomy and a limited CT scan are helpful in pin placement. We recommend the use of a multiple pin construct, perpendicular insertion, and precise tightening with good pin-site care and frequent follow-up. The benefits seem to outweigh the risks in this population, considering the mechanical advantages of the halo-orthosis.
Keywords: Halo-orthosis, Halo vest, Cervical spine instability
Introduction
The halo-orthosis was first described in 1959 by Perry and Nickel for stabilization of cervical arthrodesis in patients with poliomyelitis [1]. Since then the indications for its use have broadened, and gained wide acceptance for both adults and, particularly, the pediatric population. There are only a few reports in the literature discussing the indications and safety of application of halo orthoses in young children [2, 3]. In fact, some authors are against the use of halo-orthoses in children as young as 3 years old, due to their smaller and thinner skulls compared to older children and adults [4]. Further, only a few studies discuss the use of halo-orthoses based on the maturity of the skull, brain development, and changes in head circumference during childhood [2, 4–6].
The purpose of this study was to evaluate the safety and efficacy of halo-orthoses in children less than 3 years old, review the indications and clinical adequacy of immobilization, and analyze the outcomes at follow-up.
Materials and methods
After appropriate IRB approval, we retrospectively reviewed our computerized spine database for all pediatric patients that underwent halo orthoses application at our institution in the past 15 years. We identified and selected all patients that were less than 3 years old at the time of halo-orthosis application, regardless of the indication for application.
Ten patients were identified from a total of 150. There were six boys and four girls, with an average age of 2 years (range 10 months to 2 years and 10 months).
Computed tomography scan (CT) with 3D reconstruction was performed prior to the procedure to assess the neck pathology and, concurrently, the skull vault thickness and the location of the sutures, and to plan the appropriate site for placement of the pins (Fig. 1).
Fig. 1.
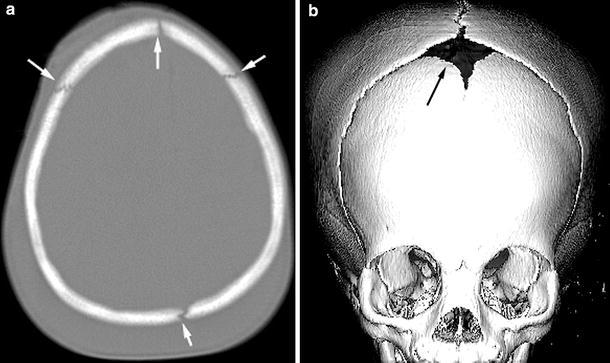
(a) CT axial image from a one-and-a-half-year-old female demonstrating the sutures (arrows), thickness, and conformation of the skull. (b) 3D reconstruction CT image demonstrating the sutures and anterior fontanele (arrow)
All the halo-orthoses were applied in the operating room, under general anesthesia, according to the previously described technique [7]. This involved the placement of a multiple-pin construct (between 6 and 10 pins) for fixation of the halo device (Fig. 2). Due to the skull anatomy and size, and scar-related problems, we tried to limit the number of anterior pins to two (one on each side), although in some cases up to four anterior pins were needed to obtain stabilization. Commercially available torque wrenches were used as previous described [8], to tighten the halo pins with a pressure of 2 in-lb; in experienced hands the so-called “freehand tightening” technique may be used. Special attention should be taken when dealing with patients that have a bone weakening condition such as osteogenesis imperfecta. In those patients the recommended pressure may exceed to their skull resistance. Wide flanged and short tipped pins were used in all cases (Fig. 3). Although the pins are not routinely retightened, it is important to verify if any loosening has occurred prior to discharge, and in every clinic appointment. All patients received an instruction sheet of how to care for their pins and also met a wound-care nurse prior to surgery.
Fig. 2.

Demonstration of a halo-orthosis applied according to standard technique
Fig. 3.

The ideal halo pin should be short-tipped and wide flanged [15]
The data collected included diagnosis, fusion technique, levels fused, neurological manifestations before and after the procedure, duration of halo-orthosis, complications related to the halo-orthosis and to the index procedure, and final clinical and radiographic outcomes (Fig. 4).
Fig. 4.
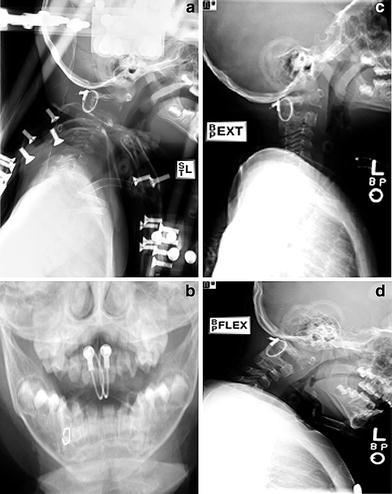
Lateral (a) and trans-oral (b) radiographs of a female 1 year 10 months old showing halo-orthosis positioned for treatment of C1-2 instability caused by C2 fracture/dislocation caused by a motor-vehicle accident. Extension (c) and flexion (d) radiographs two years post-halo-orthosis removal, showing good fusion of the C1-2 segment after a Brooks procedure (C1-C2 arthrodesis) (arrow)
Results
Four of the ten patients had a traumatic event leading to the cervical spine instability (one had occipito-C1–C2 instability; one had a C2 fracture-dislocation; one had C1–C2 instability; and one had a C3 fracture). The other six patients had non-traumatic causes of their cervical spine instability. Three patients had a congenital abnormality to the upper cervical (one patient had congenital C1-2 subluxation with stenosis; one presented with basilar impression and syringomyelia associated with hypoplastic anterior arch of C1; and one had spina bifida associated with Arnold–Chiari I malformation). Finally, three patients had upper cervical instability associated with a syndrome (one had Down syndrome with occipito-C1 instability; one had spondyloepiphyseal dysplasia with spinal canal stenosis (Fig. 5); and one had an unknown syndrome associated with Arnold–Chiari II malformation and multiple spinal abnormalities) (Table 1).
Fig. 5.
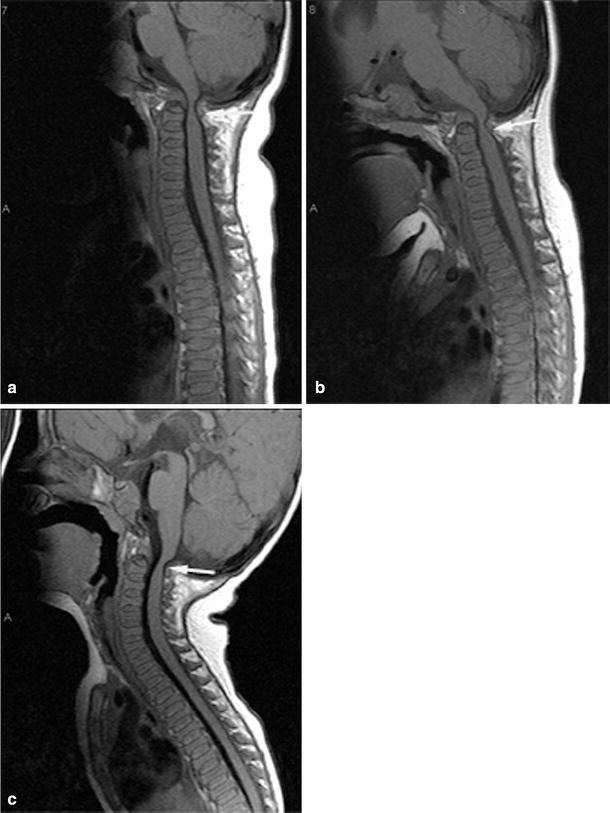
Sagittal MRI demonstrates (a) dysplastic cervicothoracic spine with decreased height of vertebral bodies and increased height of intervertebral discs, associated with marked stenosis of the spinal canal at the level of odontoid process of C2 with severe cord compression (arrow), exaggerated by flexion (b) and slightly relieved by extension (c) (patient 4)
Table 1.
Demographic characteristics of patients, including diagnosis, outcome and complications
| Patient | Gender | Agea | Diagnosis and clinical symptoms | Levels fused | Follow-upa | Clinical and surgical outcome | Halo-orthoses complications |
|---|---|---|---|---|---|---|---|
| Traumatic causes | |||||||
| 1 | F | 0 + 10 | MVA; atlanto-occipital and atlanto-axial dissociations. Quadriplegic | Occiput-C2 | 1 | Stable fusion. Persistent quadriplegia | None |
| 2 | F | 1 + 11 | MVA; C2 fracture/dislocation. Tetraplegia, ventilator-dependent | C1-2 | 1 | Stable fusion. Persistent quadriplegia | None |
| 3 | F | 2 + 4 | C1-2 instability after fall from chair | C1-2 | 9 + 5 | Two failed fusions attempts without instrumentation | None |
| 4 | M | 1 | MVA; C3 fracture/dislocation. Tetraplegia | C2-3 | 5 | Stable fusion. Persistent tetraplegia | None |
| Non-traumatic causes | |||||||
| 5 | F | 2 + 0 | Congenital C1-2 subluxation with stenosis; occipitalization of C1. Spastic quadraparesis | Occiput-C4 | 12+1 | Stable fusion. No neurologic sequelae | None |
| 6 | M | 2 + 10 | Basilar impression and syringomyelia; hypoplastic anterior arch C1. Torticollis and decreased strength lower extremities | Occiput-C2 | 3+10 | Insufficient neurosurgical decompression. Second procedure necessary. No neurologic sequelae | None |
| 7 | M | 2 + 7 | Spina bifida; upper cervical encephalocele and Chiari malformation. 2–3 beats of clonus | Occiput-C2 | 8 | Superficial dehiscence of cervical wound - treated with oral antibiotics. Radiographic evidence of recurrent instability, fractured wires and pseudarthrosis. No neurologic sequelae | Loosening of three halo-orthosis pins, tightened without issue |
| 8 | M | 2 + 6 | Down syndrome with occiput -C1 and C1-2 instability. Quadraparetic and ventilator dependent | Occiput-C2 | 5 + 9 | Stable fusion. No neurologic sequelae | None |
| 9 | M | 1 + 3 | Spondyloepiphyseal dysplasia (Kniest dysplasia) with canal stenosis and cord compression. Clonus + | Occiput-C2 | 3 | Stable fusion. No neurologic sequelae | Pin site infection, treated with oral antibiotics |
| 10 | M | 1 + 11 | Unknown syndrome with Arnold–Chiari II malformation, multiple vertebrae malformations and instability post decompression | Occiput-C2 | 6 + 3 | Superficial wound infection (treated with orals antibiotics and packing). Radiographic evidence of persistent instability, without any neurologic sequelae | None |
aYears + months
Three of the four patients that sustained acute trauma, and five from the non-traumatic group had clinically evident neurologic compression prior to the surgery. One patient from the first group and all patients from the second group improved their neurological status after surgical decompression.
The average time of halo-orthoses immobilization was 75 days (range 33–168 days) and the average follow-up time was 5 years and 2 months (range 1–12 years).
Post-operatively, there were two halo-orthoses-related complications and four related to the index procedure. Halo-orthoses related problems included three pins loosening in one patient (patient 7; re-tightened without further problems) and transient pin site infection in another patient (patient 9; successfully treated with oral antibiotics for 10 days and fusion achieved without delays) (Fig. 6). None of the halo-orthoses needed to be removed because of these complications. It is important to pay special attention to pins that are retightened, as there is a risk of skull penetration and epidural abscess.
Fig. 6.
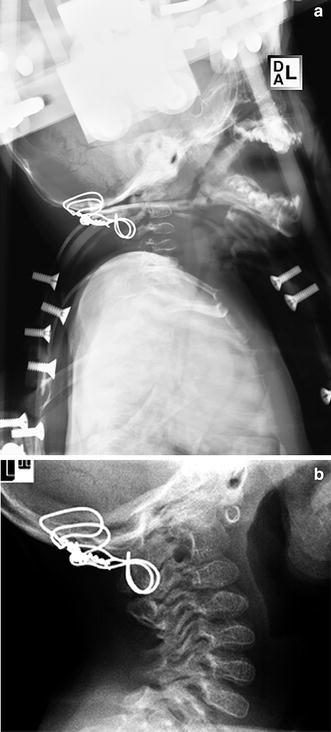
(a) Lateral radiograph of a 1 year and 3 months old boy with spondyloepiphyseal dysplasia and marked canal stenosis (Fig. 5), in the halo-orthosis after surgical decompression and occipital-C2 fusion. (b) Lateral radiographs at three-years follow-up, demonstrating good fusion mass
There were four complications associated to the index procedure, all early in the series, including three cases of pseudarthrosis and one patient that had an insufficient decompression of basilar invagination (patient 6). Three patients underwent revision surgery, and all, except for one (patient 3; who required a third procedure after two failed fusions without instrumentation), achieved stable fusion (detailed information is given in Table 2). Because one of the patients that developed pseudarthrosis had a fibrous union and was clinically stable (patient 10), revision surgery was not indicated. Interestingly, two of the three failed fusions occurred at the occipito-cervical junction, which prompted us to develop new techniques for fusion at this level [9, 10].
Table 2.
Management of index surgery-related complications
| Patient | Complication | Management | Final outcome |
|---|---|---|---|
| 3 | Failed fusion after two attempts of arthrodesis without instrumentation | Third surgical procedure with internal fixation (wires) and graft augmentation | Stable fusion (clinically and radiographically) |
| 6 | Insufficient decompression of basilar invagination | Second surgical procedure with wide decompression, graft augmentation and fusion extension to C3 | Stable fusion (clinically and radiographically) |
| 7 | Radiographic evidence of recurrent instability and fractured wires | Second procedure with revision of the fusion, internal fixation (wires) and grafting | Stable fusion (clinically and radiographically) |
| 10 | Radiographic evidence of persistent instability on dynamic imaging, intact hardware and no neurologic compromise | Close observation | Fibrous union (clinically stable) |
Discussion
Perry and Nickel first described the use of halo-orthosis for stabilization of the upper cervical spine, after cervical arthrodesis in a patient with poliomyelitis [1]. Since then, the indications for use of halo orthoses have gradually expanded not only for use in adults but also in children.
Most of the reports regarding the use of halo-orthoses in the pediatric population and its associated complications have not focused on the implications of chronology of maturation (skull and brain development), and the head circumference changes that matter in the application of the orthosis. While applying a halo-orthosis in children younger than 3 years old it is important to note that the posterior fontanelle closes at around 4 months of age and the anterior fontanelle at around 18 months, and that the cranial bones complete their inter-digitation by 24 months. Therefore cranial distortion and cranial bone shifting with pin placement are a possible risk [1, 2].
In a previous study from our own institution, we reported 37 children (3–16 years of age) managed with immobilization in a halo-orthosis. There were complications noted in 68% of the patients, and those rates were comparable to the rates in the adult population [6, 11]. Pin site loosening with or without infection was the most common complication. This usually resolved with a course of oral antibiotics or pin replacement with tightening. Children younger than 10 years were noted to have a higher incidence of complications [11]. In another retrospective study that compared halo-orthoses complications in adults and children, the incidence of complications in children was almost four times higher than in adults [12]. In the current study, our inclusion criterion was limited to three years and younger based on skull osteology and the clinical studies previous described [4, 13].
Two of the ten patients in this series developed pin site complications, such as pin site loosening with or without infection. Three patients failed to achieve osseous union following the index surgery. One can only speculate as to the cause of the nonunion. Possible explanations include: an associated syndrome such as Down syndrome where fusion difficulties are well known [14]; arthrodesis following a wide decompression that left a limited fusion bed; and insufficient surgical stabilization either from the fusion technique or the halo application. The occurrence of non-union early in this series prompted us to develop newer techniques for arthrodesis of the upper cervical spine, with apparently better results [9, 10].
Most studies have presented a higher complication rate in children treated with halo orthoses [6, 11, 12]. Some authors advise against halo-vest application in children younger than 3 years because of the comparatively thinner skull compared with older children and adults. By so doing, one can avoid the potential risk of complications including skull penetration, pin loosening, and pin site infection [4]. There are very few reports in the literature discussing the role of halo orthoses in children less than 3 years. Mubarak et al. [2] reported three patients less than 3 years of age treated by halo-orthosis. Two of the three developed loosening and pin site infection but all achieved successful fusion. They stressed the importance of using a multiple pin construct rather than the usual four pins fixation in adults. We concur with this and we have used between six and ten pins per patient to enhance the stabilization. One study analyzed the halo use in children younger than 3 years and 9 of 13 children presented with some complication [3].
Further, we advise close attention to several technical principles during halo-orthosis immobilization in children. In a comparative evaluation of halo-orthoses pin designs and different angles of pin insertion, in an immature animal skull model, we observed that a wide flanged, short tipped pin design and perpendicular pin insertion was associated with a lower likelihood of complications, because of an improved capacity of the skull vault to resist penetration and increased structural property (increased load at the pin–bone interface) [15, 16]. These principles associated with an optimum technique of halo-orthosis pin insertion, aiming to avoid over or under tightening (i.e. preventing skull inner table penetration, or pins loosening), by utilizing the most accurate and reliable torque wrenches, are encouraged [8]. Furthermore, in a study using dried human cadaver skulls, the eight-pin fixation was shown to be mechanically better than the four-pin construct for the immature skull model [17]. Finally, due to the high variability of skull thickness in children we strongly recommend computed tomography scans in the pre-operative evaluation and planning, to determine safe areas for pin placement.
Understanding the chronology of skull development in children, attention to the recommended technique, and proper pin-site care can help to decrease the risk of complications associated with halo-orthoses in children less than 3 years old. Although there are several newer surgical implants designed for stabilizing the upper cervical spine in older and larger children and adults, these techniques may not be appropriate for children less than three. Because of size and bone strength constraints, external fixation through a halo-orthosis may be the preferred method of providing or augmenting adequate fixation for the unstable cervical spine in this group. Although there are reported complications from this technique, the benefits seem to outweigh the risks in this population, considering the mechanical superiority of halo-orthosis to the collar orthoses in these cases where stable immobilization is indicated.
Halo-orthosis seems to be an effective and safe instrument for upper cervical spine stabilization in children less than 3-years-old, when applied following the described protocol. We recommend the use of pre-operative CT scan to plan appropriate pin placement, and the use of wide flanged and short tipped pins in a multiple pin construct, inserted perpendicular to the outer table and tightened using precise wrenches.
Footnotes
The authors certify that their institution has approved the reporting of this study, that all the investigations were conducted in conformity with ethical principles of research, and informed consent was obtained.
References
- 1.Perry J, Nickel VL. Total cervicalspine fusion for neck paralysis. J Bone Joint Surg Am. 1959;41-A:37–60. [PubMed] [Google Scholar]
- 2.Mubarak SJ, Camp JF, Vuletich W, Wenger DR, Garfin SR. Halo application in the infant. J Pediatr Orthop. 1989;9:612–614. doi: 10.1097/01241398-198909010-00021. [DOI] [PubMed] [Google Scholar]
- 3.Caird MS, Hensinger RN, Weiss N, Farley FA. Complications and problems in halo treatment of toddlers: limited ambulation is recommended. J Pediatr Orthop. 2006;26:750–752. doi: 10.1097/01.bpo.0000235395.19042.3f. [DOI] [PubMed] [Google Scholar]
- 4.Garfin SR, Roux R, Botte MJ, Centeno R, Woo SL. Skull osteology as it affects halo pin placement in children. J Pediatr Orthop. 1986;6:434–436. doi: 10.1097/01241398-198607000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Garfin SR, Botte MJ, Centeno RS, Nickel VL. Osteology of the skull as it affects halo pin placement. Spine. 1985;10:696–698. doi: 10.1097/00007632-198510000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986;68:320–325. [PubMed] [Google Scholar]
- 7.An HS, Riley LH., III . An atlas of surgery of the spine. 1st edn. Philadelphia, NY: Lippincott Raven; 1998. pp. 10–12. [Google Scholar]
- 8.Copley LA, Dormans JP, Pepe MD, Tan V, Browne RH. Accuracy and reliability of torque wrenches used for halo application in children. J Bone Joint Surg Am. 2003;85-A:2199–2204. doi: 10.2106/00004623-200311000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MW, Drummond DS, Flynn JM, Pill SG, Dormans JP. A technique of occipitocervical arthrodesis in children using autologous rib grafts. Spine. 2001;26:825–829. doi: 10.1097/00007632-200104010-00026. [DOI] [PubMed] [Google Scholar]
- 10.Dormans JP, Drummond DS, Sutton LN, Ecker ML, Kopacz KJ. Occipitocervical arthrodesis in children. A new technique and analysis of results. J Bone Joint Surg Am. 1995;77:1234–1240. doi: 10.2106/00004623-199508000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Dormans JP, Criscitiello AA, Drummond DS, Davidson RS. Complications in children managed with immobilization in a halo vest. J Bone Joint Surg Am. 1995;77:1370–1373. doi: 10.2106/00004623-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Baum JA, Hanley EN, Jr, Pullekines J. Comparison of halo complications in adults and children. Spine. 1989;14:251–252. doi: 10.1097/00007632-198903000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Wong WB, Haynes RJ. Osteology of the pediatric skull. Considerations of halo pin placement. Spine. 1994;19:1451–1454. doi: 10.1097/00007632-199407000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Segal LS, Drummond DS, Zanotti RM, Ecker ML, Mubarak SJ. Complications of posterior arthrodesis of the cervical spine in patients who have Down syndrome. J Bone Joint Surg Am. 1991;73:1547–1554. [PubMed] [Google Scholar]
- 15.Copley LA, Pepe MD, Tan V, Dormans JP, Gabriel JP, Sheth NP, Asada N (1998) A comparative evaluation of halo pin designs in an immature skull model. Clin Orthop:212–218 [DOI] [PubMed]
- 16.Copley LA, Pepe MD, Tan V, Sheth N, Dormans JP. A comparison of various angles of halo pin insertion in an immature skull model. Spine. 1999;24:1777–1780. doi: 10.1097/00007632-199909010-00005. [DOI] [PubMed] [Google Scholar]
- 17.Letts M, Girouard L, Yeadon A. Mechanical evaluation of four- versus eight-pin halo fixation. J Pediatr Orthop. 1997;17:121–124. [PubMed] [Google Scholar]


