Abstract
Purpose
To demonstrate the effectiveness of intramedullary fixation of severely displaced proximal humeral physeal fractures in skeletally immature children using the elastic stable intramedullary nail (ESIN).
Methods
Retrospective recruitment of 14 patients aged 10–15-years old with severely displaced proximal humeral physeal fractures between 1999 and 2004 in a single regional specialist paediatric orthopaedic hospital. The fractures were graded using the Neer classification; severe displacement constituted Neer II–IV or displacement >1 cm and angulation >45°. Patients were followed up and assessed using the Disabilities of the Arm, Shoulder and Hand score (DASH) and the Neer Shoulder score. Radiographs were assessed for deformity. Subjective satisfaction was assessed.
Results
Fourteen patients with mean follow-up of 30 months (12–66 m) from surgery. All fractures were radiologically united at a median time of eight weeks (7–10 weeks). At follow-up, Neer Shoulder mean score was 96.79 (range 83–100) and DASH mean score 2.26 (0–7.5). Subjectively 71% were very satisfied and 29% were satisfied.
Conclusions
We commend stabilisation using ESIN in the management of the displaced proximal humeral physeal fracture in older children, once reduction of the fracture has been achieved by either closed or open means. ESIN is safe and allows early return to pre-injury function.
Keywords: Elastic nails, Proximal humeral physis
Introduction
Fractures of the proximal humeral physis are relatively uncommon in children and account for 0.45% of all paediatric fractures. Fractures of the proximal humeral physis have been classified by Neer and Horwitz [1] into grades I–IV depending on the severity of displacement and degree of comminuition. Most proximal humeral fractures in the skeletally immature patient are undisplaced or minimally displaced (Neer and Horwitz grade I) and historically have been managed nonoperatively. The treatment of severely displaced fractures (Neer II–IV) in children is controversial.
Neer’s classification is based on the four-part concept and includes anatomical and biomechanical considerations, and can predict treatment course and prognosis. The four fracture parts are the anatomical neck, the surgical neck and the greater and the lesser tuberosities. Neer one-part (I) fractures are those with none-to-minimal angulation (less than 45°), and none-to-minimal displacement (less than 1 cm) of the fracture fragments; any of the four proximal humeral segments may be fractured. Neer two-part (II) fractures consist of one displaced (and three undisplaced) fracture fragments. Neer three-part (III) fractures are those with two displaced (and two undisplaced) fracture fragments. Neer four-part (IV) fractures involve three displaced fracture fragments.
Most proximal humeral fractures in the skeletally immature patient are minimally displaced (Neer I) and are managed nonoperatively in a shoulder immobiliser followed by range of movement exercises. The treatment of severely displaced (Neer II–IV; displacement >1 cm and angulation >45°) closed proximal humeral fractures is not clear. In the younger child with good remodelling potential a nonoperative approach is favoured, whilst surgery to achieve and maintain fracture reduction is advised in the older child with little remodelling potential. Various surgical techniques using staples, screws, pins and plates for fixation have been utilised, but these techniques have not been without complications.
The aim of this study was to present the results for a group of skeletally immature patients with closed displaced proximal humeral fractures treated using elastic stable intramedullary nails (ESIN).
Patients and methods
Between January 1999 and August 2004, all patients with a proximal humeral fracture who were treated at the Sheffield Children’s Hospital were reviewed for inclusion into this retrospective study. The inclusion criteria were: age of more than 10 years (for the purposes of this study, this defined the “older” child); open epiphyseal plate; proximal humeral fracture with displacement of not less than two thirds of the humeral shaft (>1 cm); and severe (>45°) angulation.
Fourteen patients met the criteria and formed the basis of this study. There were twelve boys and two girls with a mean age of 12.5 years (10–15 years) at the time of injury. No patient had bilateral fractures. The mechanism of injury was a pedestrian vehicular accident in four and a fall during a sport-related activity in the remaining ten. All the fractures were closed injuries. Ten patients had a Neer Grade III epiphyseal fracture and four had a completely displaced metaphyseal fracture of the proximal humerus. All the fractures were treated by closed–open reduction and stabilisation using ESIN (Depuy, France).
We undertook a retrospective review evaluation including clinical and radiological assessments. The mean follow-up was 30 months (12–66 months). The evaluation was carried out by a single independent observer. Clinical evaluation was both subjective and objective.
The Neer Shoulder [1] and DASH [2] (Disability of the Arm, Shoulder and Hand) scores were used for objective assessment and issued at the time of hardware removal or at most recent follow-up. The Neer Shoulder score is a 100-point shoulder score, which assesses pain during the past week, clinical testing of shoulder function, active range of movement, and anatomical or radiological examination. It is divided into four subscales: excellent 90–100; satisfactory 80–89; unsatisfactory 70–79; and failure <70.
The DASH outcome measure is another 100-point shoulder score. It is a patient-completed 30-item questionnaire measuring physical and social function together with symptoms in any or all joints in the upper extremity. Converse to the Neer Shoulder score, a lower DASH score signifies a more favourable outcome.
As part of a subjective assessment, patients were asked if they were very satisfied, satisfied or not satisfied with the outcome of treatment. In addition, a review of the medical records was undertaken. All of the patients denied any problems with the injured arm prior to surgery.
Radiological evaluation was carried out using standard anteroposterior and lateral views of the humerus and an axillary view of the shoulder on the injured side. The radiographs were undertaken at defined intervals and were evaluated for deformity, shortening, fracture union and hardware-related complications (Fig. 1).
Fig. 1.
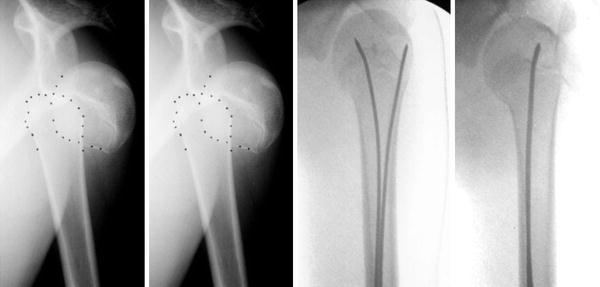
Pre- and post-operative radiographs of proximal humeral physeal injury
Surgical technique
All of the operative procedures were carried out under general anaesthetic. The affected upper limb was supported by a radiolucent arm table. An image intensifier was positioned so that the long axis of the humerus was in view. Under image intensifier guidance, surface markings were made on the skin for the fracture site, proximal and distal physes.
An initial attempt at closed reduction was made in all patients. This was performed by gentle longitudinal traction with abduction and external rotation of the arm. An image intensifier was used to monitor reduction. If closed reduction failed, the surgeon proceeded to open reduction utilising an anterior deltopectoral approach.
Two retrograde oblique drill holes were created on the lateral supracondylar ridge, one above the other, taking care to drill far enough to get through the solid columns of bone in the distal humerus. The inferior of the two holes was placed approximately 2 cm proximal to the olecranon fossa. The holes were made slightly larger than the diameter of the chosen nail. The diameter of the nail was selected based on the narrowest diameter of the medullary canal on radiographs using the formula 0.4× diameter of the canal in mm.
The first pre-bent ESIN was introduced through the inferior hole and passed upwards towards the fracture site. The second ESIN was then introduced and advanced in retrograde fashion to the fracture site. Once reduction was achieved, the ESINs were advanced across the fracture site into the humeral head. The nails were appropriately rotated to achieve final reduction and a satisfactory position in the proximal humerus without violating the cortex or shoulder joint.
The two ESINs were then bent distally and cut 1 cm from the cortical surface to allow for easy removal at a latter date. Surgical wounds were closed with absorbable Vicryl™ sutures. Skin edges were apposed using absorbable Monocryl™ subcuticular sutures.
The postoperative regime consisted of application of a collar and cuff sling to the operated upper arm for three weeks. Patients were encouraged to start pendulum exercises of the shoulder as soon as comfortable.
Routine removal of the implant was performed as part of considered good practice, and undertaken under general anaesthesia as a daycase procedure at six months.
Results
All 14 patients underwent surgery and two ESIN nails were used in each patient. In eight patients the fracture was reduced by closed means, whilst in the other six open reduction was required. An anterior deltopectoral approach was utilised. As the fracture site was explored, it was apparent that the closed reduction was blocked by the interposition of periosteum and the long head of biceps.
The commonest ESIN nail size was 2.5 mm. Average operating time was 74 min. Length of hospital stay varied between 2–3 days. Post-operatively, mean follow-up in clinic was 30 months (12–66 months).
Neer Shoulder and DASH scores are presented in tabulated format (Table 1). Neer Shoulder score following operative management of displaced proximal humeral fractures in older children using ESIN was mean score 96.79 (range 83–100). DASH shoulder score was mean 2.26 (0–7.5).
Table 1.
Outcome following elastic nailing for proximal humeral physeal fracture
| Case no. | Age | Sex | Mechanism of injury | Reduction method | DASH score | Neer Shoulder score | Subjective outcome |
|---|---|---|---|---|---|---|---|
| 1 | 13 y 8 m | M | Sport (rugby) | Closed | 5.0 | 90 | Very satisfied |
| 2 | 12 y 9 m | M | Sport (rugby) | Open | 0.0 | 100 | Very satisfied |
| 3 | 10 y 0 m | M | RTA | Open | 0.0 | 100 | Very satisfied |
| 4 | 13 y 0 m | F | Sport | Open | 6.7 | 93 | Satisfied |
| 5 | 12 y 0 m | F | Sport (horse-riding) | Closed | 0.0 | 98 | Very satisfied |
| 6 | 12 y 0 m | M | Sport (motocross) | Closed | 0.0 | 100 | Very satisfied |
| 7 | 15 y 4 m | M | Sport | Open | 5.8 | 100 | Very satisfied |
| 8 | 10 y 0 m | M | RTA | Closed | 2.5 | 100 | Satisfied |
| 9 | 12 y 0 m | M | Sport | Closed | 2.5 | 93 | Very satisfied |
| 10 | 14 y 6 m | M | RTA | Open | 0.0 | 100 | Very satisfied |
| 11 | 11 y 6 m | M | RTA | Open | 7.5 | 83 | Satisfied |
| 12 | 13 y 0 m | M | Sport | Closed | 1.7 | 100 | Satisfied |
| 13 | 13 y 10 m | M | Fall | Closed | 0.0 | 100 | Very satisfied |
| 14 | 13 y 0 m | M | Fall | Closed | 0.0 | 98 | Very satisfied |
RTA road traffic accident
One patient presented with radial nerve symptoms. This was a transient radial nerve neurapraxia, which occurred at the time of fracture and symptoms had fully resolved at post-operative follow-up.
No major complications were observed in relation to surgery. Soft tissue irritation by the protruding distal end of the nail from the humerus was observed in three patients. This resolved in all cases on removal of hardware.
In a subjective measure of outcome at follow- up, 71% of patients were very satisfied and 29% satisfied; no patients reported their outcome as not satisfied.
All fractures appeared radiologically united at a median time of eight weeks (7–10 weeks). There was no instance of loss of reduction, residual deformity or nail migration during the post-operative period.
Routine removal of hardware was undertaken in all 14 patients. The implants were removed under general anaesthesia as a daycase procedure without difficulty at a median time of six months from the index operation. There were no observed complications in association with removal of hardware.
Discussion
Fracture of the proximal humeral physis in children is a relatively uncommon injury and accounts for less than 1:200 of all paediatric fractures. The mechanism of injury in fractures of the proximal humeral physis in children is often similar to that responsible for producing a shoulder dislocation in an adult. The common causes are sports-related injuries and road traffic accidents. This compares to our series with ten sports-related cases and the remaining four cases related to pedestrian vehicular accident.
Many authors advocate nonoperative treatment of severely displaced fractures regardless of age of the patient. This is because the proximal humeral physis remains open in girls until age 17 years and in boys until 18 years. Furthermore, the proximal humeral growth accounts for 80% of the length of the humerus. Hence, the potential for remodelling is great. In addition, the shoulder joint has an excellent arc of motion, enabling it to overcome and compensate for residual deformity. Finally, various complications have been reported in association with operative management.
A review of the reports of nonoperative treatment of proximal humeral fractures reveals a number of shortcomings in the current literature: (1) nonoperative treatment has not strictly been nonoperative; (2) a significant number of undisplaced or minimally displaced fractures have been included; and (3) small numbers of older children or adolescents. Reports have tried to examine the outcome of nonoperative treatment for these fractures in the older child or adolescent and found increased subjective complaints such as weakness, cosmesis and overall decrease in shoulder function.
Dameron and Reibel [3] in their case series of 46 proximal humeral physeal fractures observed poor outcome in patients aged 14 years or older, who lost fracture reduction during the course of treatment. Burgos-Floves et al. [4] reported excellent results in 22 patients with Neer grade III and IV proximal humeral epiphyseal fractures treated with closed/open reduction and fixation with Kirschner wires. They recommend a more aggressive approach to correct the initial displacement and angulation in older children. Beringer et al. [5] in 1998, Dobbs et al. [6] in 2003, and Schwendenwein et al. [7] in 2004 concluded in their reports that achieving and maintaining reduction of severely displaced proximal humeral epiphyseal fractures in the older adolescent is beneficial.
In our unit we used Beatys [8] guidelines for accepting position for humeral alignment. Fracture reduction was carried out under general anaesthesia. In eight patients this was achieved by closed manipulation. In six patients (43%) closed reduction failed and an open reduction was undertaken through the deltopectoral approach. This rate of opening is in keeping with published data. The long head of biceps and periosteum was found to be interposed in the fracture and prevented reduction in all these cases.
Maintaining fracture reduction is important to overall outcome, but this can be challenging. Traction, slings, abductor bolster bracing or shoulder spica have been used to maintain fracture reduction, but displacement rates of up to 80% have been reported.
Fracture reduction may otherwise be maintained with internal fracture fixation using plates, staples, screws or wires. Complications such as osteomyelitis, impingement caused by hardware, loss of reduction and fractures have been reported using these modes of fracture fixation.
In view of reported complications we have used ESIN to maintain fracture reduction. ESIN was developed in the late 1970s by the team of Jean Prevot [9] and Paul Metaizeau [10] at The Childrens Hospital of Nancy in France. The concept of using ESIN for the treatment of proximal humeral fractures in children was first reported by Ligier et al. [11] in 1983. In 1990 Sessa et al. [12] reported on 55 humeral fractures in the skeletally immature treated by centromedullary nailing. They reported a 14% varus malunion rate and 2% of their patients had infection. Johnson et al. [13] in 2006 recommended the use of flexible nailing as a safe method of maintaining reduction in unstable or irreducible displaced fractures of the proximal humerus in children.
In our case series of 14 older children, Neer Shoulder score following operative management of displaced proximal humeral fractures using ESIN was mean score 96.79 (range 83–100); 13 cases scored as excellent and the remaining one case as satisfactory. DASH shoulder scoring was mean score 2.26 (0–7.5); seven cases had the best possible outcome score of zero.
We have not observed any major complications in our case series. In particular, we have not observed problems such as deep infection, growth plate injury or new fracture that has been reported with other forms of fracture fixation. The minor complication of soft tissue irritation related to proud hardware at the distal humerus in three patients was addressed on routine removal of hardware at an interval of six months. We accept that a second operative procedure is invariably required to remove the hardware. No complications were associated with this secondary procedure in our series.
Subjectively all 14 patients in our series were very satisfied or satisfied with their outcome. None of the patients complained of loss of glenohumeral movement or loss of function. All returned to the pre-injury level of sports participation within a short time. This we believe is due to the good fracture reduction, maintenance of this reduction, a short period of immobilisation and the minimal complication rate.
A limitation of our study is that we have a relatively small number of cases. In addition, the study aimed to look at these fractures in the older child. The mean age of the 14 patients in this case series was 12.5 years and does not fully represent the adolescent approaching skeletal maturity.
Based on a review of the literature, we believe that operative fixation to reduce and maintain position should be considered for the management of severely displaced proximal humeral fractures in the older child or adolescent as they have reduced remodelling potential.
The results of our study demonstrate that once reduction has been achieved, by closed or open means, the ESIN provides excellent fracture fixation, maintains the reduction, is safe, and allows for early mobilisation and a return to pre-injury function.
References
- 1.Neer CS, Horowitz BS. Fractures of the proximal humeral epiphyseal plate. Orthopaedics. 1965;41:24–31. [PubMed] [Google Scholar]
- 2.Hudak PL, Amadio PC, Bombardier C, et al. (1996) Development of an upper extremity outcome measure: The DASH. Am J Ind Med 29:602–608 [DOI] [PubMed]
- 3.Dameron TB, Reibel DB. Fractures involving the proximal epiphyseal plate. JBJS(A) 1969;51:289–297. [PubMed] [Google Scholar]
- 4.Burgos-Floves J, Gonzalez-Herranz P, Lopez-Mondejar JA, et al. (1993) Fracture of the proximal humeral epiphysis. Int Orthop 17:16–19 [DOI] [PubMed]
- 5.Beringer DC, Weiner DS, Noble JS, et al. (1998) Severely displaced proximal humeral epiphyseal fractures: a follow up study. J Pediatr Orthop 18:31–37 [PubMed]
- 6.Dobbs MB, Luhmann SL, Gordon E, Strecker WB, Schoernecker PL. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop. 2003;23:208–215. [PubMed] [Google Scholar]
- 7.Schwendenwein E, Hajdri S, Gaebler C, Stengg K, Vecsei V. Displaced fractures of the proximal humerus in children require open/closed reduction and internal fixation. Eur J Pediatr Surg. 2004;14:51–55. doi: 10.1055/s-2004-815781. [DOI] [PubMed] [Google Scholar]
- 8.Beaty JH (1992) Fractures of the proximal humerus and shaft in children. In: Eibert RE (ed) AAOSW instructional course lectures, Chicago. Am Acad Orthop Surg 369–372 [PubMed]
- 9.Prévot J, Lascombes P, Ligier JN (1993) L’embrochage centromédullaire élastique stable: méthode d’ostéosynthèse des fractures des members chez l’enfant. Principe et application au femur. A propos de 250 fractures suivies depuis 1979. Chirurgie 119:473–476 [PubMed]
- 10.Ligier JN, Métaizeau JP, Prévot J, Lascumber P. Elastic stable intramedullary pinning of long bone shaft fracture in children. Z Kinderchir. 1985;40:209–212. doi: 10.1055/s-2008-1059775. [DOI] [PubMed] [Google Scholar]
- 11.Ligier JN, Métaizeau JP, Prévot J. Embrochage centromédullaire élastique á foyer fermé en traumatologie pédiatrique. Chir Pediatr. 1983;24:383–385. [PubMed] [Google Scholar]
- 12.Sessa S, Lascombes P, Prévot J, Gagneux E, Blanquart D. Embrochage centromédullaire dans les fractures de l’extrémité supérieure de l’humérus chez l’enfant. Chir Pediatr. 1990;31:43–46. [PubMed] [Google Scholar]
- 13.Johnson P, Kurien N, Belthur MV, Jones S, Flowers MJ, Fernandes JA (2006) Flexible nailing for displaced humeral fractures in children. JBJS(Br) 88B(Supp):119


