Abstract
Purpose
Chiari medial displacement osteotomy is a procedure that uses the cancellous bone of the ilium to contain the femoral head and bear weight. It is the most contraversial osteotomy of the hip joint. This study was therefore conducted to determine the results of this osteotomy with mid-term follow-up in children.
Methods
From 1995 to 2004, 20 Chiari pelvic osteotomies (in 18 patients) were performed. There were 15 male and 3 female patients. The average age at operation was 12.6 years and the mean follow-up was 54 months. The operative technique was as described by Chiari. An iliofemoral approach was used without utilizing a traction table. If there was anterior or anterolateral uncoverage of the femoral head, bone graft augmentation was performed.
Results
The angle of the osteotomy averaged 12°, with the distance from the acetabulum averaging 3.2 mm. The average displacement was 42%. Of the 20 Chiari osteotomies, 11 were categorized as excellent, 8 as good and one as fair in terms of clinical and radiological results. Student’s t test statistics showed improvements in all radiologic parameters of the hip joint (Sharp angle, center-edge angle and coverage of the femoral head). Graft resorption was observed in 25% of the patients.
Conclusion
There are very rare indications of Chiari osteotomy in patients younger than 10 years. Because of the high rate of graft resorption, Chiari osteotomy should be the last treatment option when there is anterior or anterolateral uncoverage of the hip joint.
Keywords: Pelvic osteotomy, Acetabular dysplasia, Outcome
Introduction
Chiari medical displacement osteotomy was first described in 1955, and the operation has been widely used [1]. Unlike operations that redirect the acetabular cartilage and the subchondral bone, called reconstructive procedures, the Chiari medial displacement osteotomy is a salvage procedure that uses the cancellous bone of the ilium with interposed hip joint capsule to contain the femoral head and bear weight. An osteotomy of the pelvis is performed at the superior margin of the acetabulum, and the pelvis inferior to the osteotomy along with the femur is displaced medially; then the superior fragment of the osteotomy becomes a shell, and the capsule is interposed between it and the femoral head.
In the present study, the results of Chiari osteotomy in adolescents are evaluated and all aspects of Chiari pelvic osteotomy are reviewed.
Materials and methods
From 1995 to 2004, 20 Chiari pelvic osteotomies (in 18 patients) were performed in two university hospitals. There were fifteen male patients and three female patients. The average age at operation was 12.6 years, ranging from nine years and two months to eighteen years and five months.
The preoperative diagnoses were: Perthes’ disease, ten hips; developmental dysplasia of the hip, two hips; cerebral palsy, two hips; multiple epiphyseal dysplasia, one hip; poliomyelitis, one hip; avascular necrosis of the femoral head (post slipped capital femoral epiphysis or post-traumatic), four hips.
To bring down a high-riding femoral head, a concomitant varus derotation osteotomy of the proximal femur was carried out in two patients, and in six patients it was performed before the Chiari procedure (one with open reduction of the hip and shortening of the femoral bone). A concomitant greater trochanter transfer was performed in one patient, and an adductor tenotomy was done in one patient.
The operative technique was as described by Chiari [1]. An iliofemoral approach was used without utilizing a traction table. To cover the anterior part of the femoral head, bone graft augmentation was done in twelve hips. Two patients had a bilateral Chiari operation and one had Chiari operation in one hip and a shelf augmentation procedure in the other side.
The follow-up period ranged from two years to ten years, with an average of 54 months. The patients were evaluated clinically and radiographically. Plain standing roentgenograms of the pelvis and both hips were made preoperatively and at each follow-up visit. To better determine femoral head coverage, MR imaging in ten patients and a false profile image of the hip joint in all patients were undertaken preoperatively.
Three hip parameters (the center-edge angle of Wiberg, the acetabular angle of Sharp [2], and the percentage of femoral head uncoverage) and three osteotomy parameters (the angle of the osteotomy, the distance of the osteotomy from the acetabular edge, and the percentage of displacement) were evaluated (Fig. 1).
Fig. 1.
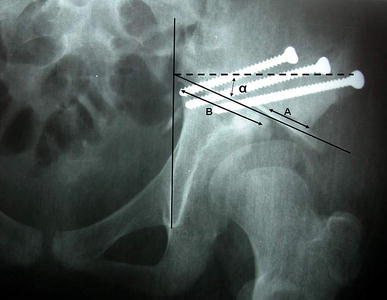
Radiographic parameters of Chiari osteotomy. Angle of Chiari (α), the angle between the line parallel to the reference line (intertear drop line) and the osteotomy line. Displacement = line A/line B × 100
The patients were evaluated clinically and radiographically based on the method of De Waal Malefijt et al. [3], which was modified by Hosney et al. [4] (Table 1). The table was modified again to better categorize each patient based on the total clinical and radiological scores. Because of the limited number of patients and the comparable hip pathology in all patients (femoral head uncoverage), we evaluated all patients with the same method.
Table 1.
Final assessment of the results
| Category (total score) | Pain | Limp | ROM | Sharp angle (°) | CE angle (°) | Uncoverage (%) |
|---|---|---|---|---|---|---|
| Excellent (0) | Noa | No | Normal | 43 | >25 | 10 |
| Good (1–6) | Improved or not deteriorateb | 45 | 20 | 20 | ||
| Fair (7–12) | Not deterioratedc | 50 | 15 | 30 | ||
| Poor (13–18) | Deterioratedd | >50 | 15 | >30 | ||
ROM Range of motion, CE center-edge
aEach item has a score of zero
bEach item has a score of 1
cEach item has a score of 2
dEach item has a score of 3
Correlations between the final results and the studied variables were determined using the Fisher exact test, whereas correlations between quantitative variables were determined with Pearson correlation and Student’st-test statistics.
Results
The angle of the osteotomy averaged 12° (range 0–32°), with the distance from acetabulum averaging 3.2 mm (0–7 mm). In the final assessment radiographs, the osteotomy step from the acetabular edge was completely remodeled in 17 hips (85% of cases) with a primary distance of ≤ 5 mm; in the others it was partially remodeled in two and not remodeled in one patient with a primary distance of 7 mm. The average displacement was 42% (range 25–78%) (based on the pre-operative measurement of the desired CE angle). There was not a significant correlation between the remodeling of the roof step, the displacement of the osteotomy and the final result categories. In spite of a high osteotomy angle in one patient (32°), there was no unwanted osteotomy ending in the sacroiliac joint.
Of the 20 Chiari osteotomies, eleven were categorized as excellent, eight as good and one as fair according to clinical and radiological results. The one fair result was a patient with coxa magna due to Perthes’ disease, who had been treated by varus osteotomy of the proximal femur in the early stages of the disease. Then he was reoperated on by Chiari osteotomy and bone graft augmentation. Postoperatively, the bone graft was resorbed. Clinically he was not deteriorated, but coverage of the femoral head was lost without subluxation (Fig. 2).
Fig. 2A–D.

A 9.5-year-old boy with Perthes’ disease, who had been operated at the age of eight with varus osteotomy of the proximal femoral bone. Eighteen months later, Chiari osteotomy and bone graft augmentation was performed for coxa magna and extruded femoral head (A–C); the nine-year follow-up radiograph showed complete resorption of the bone graft and uncoverage of the femoral head (D)
In four patients there were varying degrees of pain preoperatively; three had improvement, whereas one remained the same. Limping was improved in all but two patients, who were not deteriorated. At the last visit examination, there was no new incidence of Trendelenburg limp. Hip mobility was improved in eleven cases, remained the same in nine cases, and deterioration was not seen.
Student’s t-test statistics showed improvements of all radiologic parameters of the hip joint (Sharp angle, CE angle, and coverage of the head) (P-values: 0.002, 0.004, and 0.002, respectively). There was no correlation between radiologic parameters and the pain levels or ROM of the hip joint. The disease-type of the patients did not show any correlation with the clinicoradiological assessment results.
There were three (25%) resorptions of bone grafts inserted as anterior augmentation, and one superficial infection after removal of varus osteotomy plate.
Discussion
Chiari pelvic osteotomy is a salvage procedure performed extraarticularly; therefore, it does not violate the articular cartilage and there is little danger of creating stiffness of the hip joint. The weight-bearing surface of the hip is increased (P = 0.002), and the load on the joint surfaces is decreased.
One advantage of the Chiari operation is that the medial displacement of the hip joint shortens the medial arm of the hip abductor lever system, thus diminishing the load on the femoral head. Another advantage is the immediate formation of a strong roof that is not absorbed. The disadvantages of the Chiari procedure include narrowing of the pelvis (so bilateral Chiari osteotomy in adult patients may compromise normal vaginal child delivery), a minor degree of shortening of the lower limb because of the upward and medial displacement of the inferior segment of the innominate bone, and the risk of sciatic nerve palsy [5].
Surgical technique
Chiari [1] originally recommended using a traction table, and other surgeons have also recommended the use of a traction table or traction devices [6, 7]. Matsuno et al. [8] believed that a traction table is unnecessary for this procedure and that its usage can, in fact, result in low-level osteotomy.
The ideal Chiari osteotomy was described as making an angle of 10° upwards, immediately above the hip joint capsule and displaced by 50% of the pelvic width [9] (Fig. 1). Sticking to the technical details of the operation has been considered by most of the reports to guarantee a successful outcome [10–12].
Chiari originally described the technique using an anterior iliofemoral approach [1]. The others recommended a posterolateral approach or an Ollier lateral U approach to perform a trochanteric osteotomy at the same time [8, 13]. These approaches allow a wider exposure of the acetabulum so that it is easier to make the dome-shaped osteotomy at the appropriate level. These approaches have several other advantages: the proper angle of the osteotomy line can be obtained, and when there is a high-riding greater trochanter, a postoperative positive Trendelenburg sign can be avoided by transferring the greater trochanter distally [14, 15].
Colton [9] reported that displacing a Chiari osteotomy by more than 50% can cause substantial problems with bone-healing. Placing a bone graft medially on the cut surfaces of the ilium helps to resolve this problem [16].
Results in children, related to the study of an anatomic model of the pelvis, demonstrate that the Chiari osteotomy is unable to give much coverage to the anterior part of the femoral head. This has been demonstrated on three-dimensional computed tomographic reconstruction [17]. The recognition that the width of the proximal fragment may be insufficient to produce adequate coverage has led to the use of bone graft to augment the lateral and anterior coverage [6, 16, 18].
In this study, an iliofemoral approach was used without utilizing a traction table. Fixation was performed by screws or multiple threaded Steinmann pins and bone graft augmentation was performed in 12 patients to cover the anterior part of the femoral head. The graft was resorbed in three patients (25%), and in one patient coverage of the femoral head was deteriorated.
Chiari pelvic osteotomy in developmental dysplasia of the hip (DDH)
In acetabular dysplasia after adolescence, incongruity between the femoral head and acetabulum and early osteoarthritis usually preclude a redirectional osteotomy of the acetabulum. In such instances, only salvage procedures such as Chiari osteotomy or shelf augmentation can improve femoral head coverage and decrease the shear stress that may eventually cause degenerative arthritis.
Fong et al. [19], after following-up Chiari osteotomy for 7.1 years and shelf augmentation for 4.1 years, showed that both Chiari osteotomy and shelf augmentation provided adequate femoral head coverage in a dysplastic hip without producing pain or limiting hip mobility. The Chiari operation seemed to have better results in terms of pain relief and incidence of complications such as subluxation and resorption of bone graft.
Ohashi et al. [20] and Macnicol et al. [21] proved that Chiari osteotomy is probably radiologically effective for about 25–30 years. Interestingly, Yanagimoto et al. [22] evaluated the results of Chiari pelvic osteotomy for DDH after follow-up of ten years or more. They found that early DDH (mean age at surgery: 21 years) is a good indication for Chiari pelvic osteotomy because of the good results at follow-up of ten years or more. Hashemi-Nejad et al. [23] reported equivalent medium-term clinical and radiographic results after total hip arthroplasty (THA) when patients who had a previous successful Chiari osteotomy are compared with a control group of patients with dysplastic hips who had not undergone prior pelvic osteotomies. They indicated that THA in the post-Chiari group required fewer acetabular augmentation procedures and had shorter operating times, less blood loss, and fewer early complications.
Minoda et al. [24] evaluated biomechanical, radiological, and clinical effects of Chiari pelvic osteotomy on subsequent total hip arthroplasty in comparison with total hip arthroplasty in DDH without previous surgery. They showed that all patients had good or excellent clinical results, but that abductor force and joint force were smaller in the Chiari group, with longer operative times and more blood loss. Pain relief has been considered a constant feature of Chiari osteotomy in adult patients [1, 9, 14, 25]. Mannor et al. [26] recorded a revision rate of 20% 2–19 years after Chiari osteotomy. Long-term review inevitably shows a decline in the relief from pain, with an associated decrease in function [27, 28]. In a long-term review, Macnicol et al. [21] showed that although there are some relatively early revisions, the survival at 20 years is almost 95%.
Høgh and Macnicol [5] and Calvert et al. [29] confirmed that the radiographic progression of osteoarthritis was linear over time. Better function was achieved if the hip was operated on when the patient was younger, preferably by the age of 20–25 years [21].
Hosny et al. [4] reported that unsatisfactory outcome was present in 68% of cases younger than ten years old, whereas it was only 23% in the older group. The disappointing results in children might be related to the anti-Chiari effect. The large growth potential of the Y-growth plate and thus of the acetabulum can often result in a decentering and cranial movement of the femoral head [30].
Reddy and Morin [31] thought that this “anti-Chiari effect” was not related to an injury to the growth cartilage of the roof acetabulum but rather to a technical mistake during the Chiari osteotomy, because they did not meet such problems in their series. Bitan et al. [32] have shown in an experimental study that this anti-Chiari effect seemed to be due to the position of the osteotomy being too high.
Chiari pelvic osteotomy is rarely indicated in children and young patients with DDH, because other more anatomic osteotomies are available. There were two patients with DDH in the present study; one had avascular necrosis after open reduction, shortening and varus osteotomy of the femoral bone; the other was an 18-year-old patient with painful severe dysplasia and subluxation of the hip joint.
An anti-Chiari effect was not seen in this study because the minimum age of the patients was nine years and two months. In the author’s opinion, there is no damage of the acetabular growth center; when performing a Chiari osteotomy, the level of the osteotomy is up to the triradiate cartilage. The anti-Chiari effect probably occurs due to the persistence of the acetabular growth when this type of surgery is performed in young children.
Cerebral palsy (CP)
The two procedures with the longest historical usage in patients with CP are the Chiari osteotomy and the shelf acetabular augmentation procedure.
Dietz et al. [25] studied 24 Chiari osteotomies in CP patients at a mean seven-year follow-up and found that a pain-free joint could be obtained in 79% of hips. Seven of the 24 hips still had migration indices >30°, indicating that the subluxation persisted despite surgery. Osterkamp and colleagues [33] published the results of Chiari osteotomy performed in conjunction with varus femoral osteotomy in nine patients and without femoral procedures in three patients. Pain relief was obtained in five of six patients who complained of pain preoperatively. Two hips redislocated. They felt that the osteotomy was simple to perform and led to satisfactory results. Pope and associates [34] reported that, following varus femoral osteotomy and a Chiari osteotomy, five of seven hips remained reduced. The series with the greatest success rate was that of Altar et al. [35], in which 14 of 15 hips remained stable following a Chiari osteotomy combined with a varus osteotomy and muscle release at three-year follow-up. If patients with hip dysfunction grow up without treatment, the disease will continue to advanced osteoarthritis. After a follow-up period of six-years on eleven hips of adult CP patients who underwent Chiari pelvic osteotomy, Nishioka et al. [36] reported that good results could be achieved in 86.6% of cases.
In the present study there were only two patients with CP because acetabular dysplasia in CP is more global and acetabular fossa is so shallow for Chiari osteotomy. Therefore, other osteotomies, like Dega osteotomy, are more efficient [37]. Chiari osteotomy may be indicated in patients with closed triradiate cartilage and an incongruent hip joint.
Legg–Calvé–Perthes’ syndrome (LCP)
Chiari osteotomy improves the lateral coverage of the deformed femoral head, but doesn’t reduce the lateral impingement in abduction, and may exacerbate any existing abductor weakness [38]. Chiari osteotomy may be useful in an enlarged, poorly covered femoral head that is beginning to develop symptoms of early degenerative joint disease.
Recently, Reddy and Morin [31] performed 22 Chiari osteotomies in 21 children with severe LCP and failed conservative treatment in the early stages of the disease. They followed their patients for 6.1 years and showed that Chiari osteotomy provided an improvement in the femoral head coverage and hip congruency. Patient radiographs showed progressive spherical remodeling of the femoral head and improvement of the concentricity. Klisic et al. [39] showed that Chiari’s osteotomy is helpful where other kinds of containment cannot be expected to be successful.
If there is more global uncoverage or anterior uncoverage of the femoral head, augmentation by bone graft or other osteotomies like shelf procedure or triple osteotomy may be indicated. In the present study, there were ten hips with LCP, all of which were class 4 or 5 in the Stulberg classification [40] with aspheric femoral head. Anterior uncoverage was present in four hips, so Chiari osteotomy with bone graft augmentation was performed. One of these bone grafts was resorbed completely (Fig. 2).
Conclusion
The Chiari osteotomy can produce good or excellent results in adolescent or young adult patients who have specific indications, including painful dysplasia or uncoverage of the femoral head, in which incongruity or poor acetabular development make other reconstructive procedures inappropriate.
Because of the 25% resorption rate of bone graft, Chiari osteotomy should be the last treatment option if there is anterior or anterolateral uncoverage of the femoral head.
References
- 1.Chiari K. Medial displacement osteotomy of the pelvis. Clin Orthop. 1974;98:55–71. doi: 10.1097/00003086-197401000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein SL (2001) Developmental hip dysplasia and dislocation. In: Morrissy RT (ed) Weinstein SL Lovell and Winter’s pediatric orthopaedics, 5th edn. Lippincott Williams and Wilkins, Philadelphia, PA
- 3.De Waal Malefyt MC, Hoogland T, Nielson HKL. Chiari osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Am. 1982;64:996–1004. [PubMed] [Google Scholar]
- 4.Hosny GA, Fabry G. Chiari osteotomy in children and young adults. J Pediatr Orthop B. 2001;10:37–42. [PubMed] [Google Scholar]
- 5.Hogh J, MacNicol MF. The Chiari pelvic osteotomy: a long-term review of clinical and radiographic results. J Bone Joint Surg Br. 1987;69:365–73. doi: 10.1302/0301-620X.69B3.3584186. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez DL, Isler B, Muller M. Chiari’s osteotomy: a note on technique. Clin Orthop Res. 1984;185:53–58. [PubMed] [Google Scholar]
- 7.Salvati EA, Wilson PD. Treatment of irreducible hip subluxation by Chiari’s iliac osteotomy. A report of results in 19 cases. Clin Orthop. 1974;98:151–161. doi: 10.1097/00003086-197401000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Matsuno T, Ichioka Y, Kaneda K. Modified Chiari pelvic osteotomy: a long-term follow-up study. J Bone Joint Surg Am. 1992;74:4708. [PubMed] [Google Scholar]
- 9.Colton CL, Chiari K. Osteotomy for acetabular dysplasia in young subjects. J Bone Joint Surg Br. 1972;54:578–589. [PubMed] [Google Scholar]
- 10.Handelsman JE. The Chiari pelvic sliding osteotomy. Orthop Clin North Am. 1980;11:105–125. [PubMed] [Google Scholar]
- 11.Windhager R, Pongracz N, Schonecker W, Kotz R. Chiari osteotomy for congenital dislocation and subluxation of the hip: results after 20 to 34 years follow-up. J Bone Joint Surg Br. 1991;73:890–895. doi: 10.1302/0301-620X.73B6.1955430. [DOI] [PubMed] [Google Scholar]
- 12.Matsui M, Masuhara K, Nakata K, Nishil T, Ochi T. Early deterioration after modified rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Br. 1997;79:220–224. doi: 10.1302/0301-620X.79B2.7202. [DOI] [PubMed] [Google Scholar]
- 13.Ito H, Matsuno T, Minami A. Comparison of the surgical approaches for a Chiari pelvic osteotomy. J Bone Joint Surg. 2003;85:204–208. doi: 10.1302/0301-620X.85B2.13325. [DOI] [PubMed] [Google Scholar]
- 14.Graham S, Westin GW, Dawson E, Oppenheim WL. The Chiari osteotomy. A review of 58 cases. Clin Orthop. 1986;208:249–285. [PubMed] [Google Scholar]
- 15.Ito H, Matsuno T, Minami A. Chiari pelvic osteotomy for advanced osteoarthritis in patints with hip dysplasia. J Bone Joint Surg Am. 2004;86:1436–1445. doi: 10.2106/00004623-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Betz RR, Kumar SJ, Palmer CT, MacEwen GD. Chiari pelvic osteotomy in children and young adults. J Bone Joint Surg Am. 1988;70:182–191. [PubMed] [Google Scholar]
- 17.Klaue K, Sherman M, Perren SM, Wallin A, Looser C, Ganz R. Extra-articular augmentation for residual hip dysplasia. J Bone Joint Surg Br. 1993;75:750–754. doi: 10.1302/0301-620X.75B5.8376432. [DOI] [PubMed] [Google Scholar]
- 18.Bailey TE, Hall JE. Chiari medial displacement osteotomy. J Pediatr Orthop. 1985;5:635–641. doi: 10.1097/01241398-198511000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Fong HC, Lu W, Li YH, Leong JCY. Chiari osteotomy and shelf augmentation in the treatment of hip dysplasia. J Pediatr Orthop. 2000;20:740–744. doi: 10.1097/01241398-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Ohashi H, Hirohashi K, Yamano Y. Factors influencing the outcome of Chiari pelvic osteotomy: a long-term follow-up. J Bone Joint Surg Br. 2000;82:517–526. doi: 10.1302/0301-620X.82B4.9583. [DOI] [PubMed] [Google Scholar]
- 21.Macnicol MF, Lo HK, Yong KF. Pelvic remodeling after the Chiari osteotomy: a long-term review. J Bone Joint Surg Br. 2004;86:648–654. doi: 10.1302/0301-620X.86B5.14653. [DOI] [PubMed] [Google Scholar]
- 22.Yanagimoto S, Hotta H, Izumida R, Sakamaki T. Long-term results of Chiari pelvic osteotomy in patients with developmental dysplasia of the hip: indications for Chiari pelvic osteotomy according to disease stage and femoral head shape. J Orthop Sci. 2005;10(6):557–563. doi: 10.1007/s00776-005-0942-4. [DOI] [PubMed] [Google Scholar]
- 23.Hashemi-Nejad A, Haddad FS, Tong KM, Muirhead-Allwood SK, Catterall A. Does Chiari osteotomy compromise subsequent total hip arthroplasty? J Arthroplasty. 2002;17:731–739. doi: 10.1054/arth.2002.31974. [DOI] [PubMed] [Google Scholar]
- 24.Minoda Y, Kadowaki T, Kim M. Total hip arthroplasty of dysplastic hip after previous Chiari pelvic osteotomy. Arch Orthop Trauma Surg. 2006;126:394–400. doi: 10.1007/s00402-006-0141-6. [DOI] [PubMed] [Google Scholar]
- 25.Dietz FR, Knutson LM. Chiari pelvic osteotomy in cerebral palsy. J Pediatr Orthop. 1995;15:372–380. doi: 10.1097/01241398-199505000-00022. [DOI] [PubMed] [Google Scholar]
- 26.Mannor DA, Weinstein SL, Dietz FR (1996) Long-term follow-up of Chiari pelvic osteotomy in myelomeningocele. J Pediatr Orthop 16:769–773 [DOI] [PubMed]
- 27.Lack W, Windhager R, Kutschera HP, Engel A. Chiari pelvic osteotomy for osteoarthritis secondary to hip dysplasia; indications and long-term results. J Bone Joint Surg Br. 1991;73:229–234. doi: 10.1302/0301-620X.73B2.2005145. [DOI] [PubMed] [Google Scholar]
- 28.Macnicol MF, Uprichard H, Mitchell GP. Exercise testing after the Chiari pelvic osteotomy. J Bone Joint Surg Br. 1981;63:48–52. doi: 10.1302/0301-620X.63B1.7204474. [DOI] [PubMed] [Google Scholar]
- 29.Calvert PT, August AC, Albert JS, Kemp HB, Catterall A. The Chiari pelvic osteotomy: a review of the long-term results. J Bone Joint Surg Br. 1987;69:551–555. doi: 10.1302/0301-620X.69B4.3611157. [DOI] [PubMed] [Google Scholar]
- 30.Purath W. Die beobachtung des sogenannten anti-Chiari effektes nach bekenosteotomien bei kindern. Z Orthop. 1979;117:301–308. [PubMed] [Google Scholar]
- 31.Reddy RR, Morin C (2005) Chiari osteotomy in Legg–Calve–Perthes disease. J Pediatr Orthop Br 4:1–9 [DOI] [PubMed]
- 32.Bitan F, Duriez J, Egozcue R, Flautre B, Morel G, Morin C. The effect of Chiari osteotomy on acetabular development during growth. An experimental study in dogs [in French] Int Orthop. 1989;13:355–358. doi: 10.1007/BF00268041. [DOI] [PubMed] [Google Scholar]
- 33.Osterkamp J, Caillouette JT, Hoffer MM. Chiari osteotomy in cerebral palsy. J Pediatr Orthop. 1988;8:274–277. doi: 10.1097/01241398-198805000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Pope DF, Bueff HU, De Luca A. Pelvic osteotomies for subluxation of the hip in cerebral palsy. J Pediatr Orthop. 1994;14:724–730. doi: 10.1097/01241398-199414060-00007. [DOI] [PubMed] [Google Scholar]
- 35.Altar D, Grant AD, Bash J, Lehman WB. Combined hip surgery in cerebral palsy patients. Am J Orthop. 1995;24:52–55. [PubMed] [Google Scholar]
- 36.Nishioka E, Momota K, Shiba N, Higuchi F, Inoue A. Joint–preserving operation for osteoarthrosis of the hip in adult cerebral palsy. Aust N Z J Surg. 2000;70:431–437. doi: 10.1046/j.1440-1622.2000.01852.x. [DOI] [PubMed] [Google Scholar]
- 37.Mubarak SJ,Valencia FG, Wenger DR (1992) One-stage correction of the spastic dislocated hip: use of periacetabular acetabuloplasty to improve coverage. J Bone Joint Surg Am 74:1374 [PubMed]
- 38.Quain S, Catterall A. Hinge abduction of the hip: diagnosis and treatment. J Bone Joint Surg Br. 1986;68:61–64. doi: 10.1302/0301-620X.68B1.3941142. [DOI] [PubMed] [Google Scholar]
- 39.Klisic P, Bauer R, Bensahel H, Grill F (1985) Chiari’s pelvic osteotomy in the treatment of Legg–Calve–Perthes disease. Bull Hosp Joint Dis Orthop Inst 45(2):111–118 [PubMed]
- 40.Stulberg SD, Cooperman DR, Wallensten R (1981) The natural history of Legg–Calvé–Perthes’ disease. J Bone Joint Surg Am 63:1095 [PubMed]


