Abstract
The authors present the prospective clinical outcome of nine pseudoarthroses resulting from surgical treatment carried out in nine children, whose ages varied from 6 years and 2 months to 14 years and 2 months (mean 10 years and 2 months), who had fractures of the femoral neck. Five were classified as type II, according to the Delbet classification modified by Colonna, and four were type III. The initial fractures were caused by high-energy traumas, such as trampling, bicycle falls, and car accidents. Treatment of choice was valgus osteotomy of the femoral neck associated or not with insertion of bony graft. The mean time of follow-up was 38 months, ranging from 23 to 71 months, and the mean time of pseudoarthrosis consolidation after osteotomy was 76.6 days, varying from 45 to 240 days. In this study, all the pseudoarthroses consolidated. For final analysis of clinical and radiographic results, the Ratliff’s classification was used. We obtained three cases as good results, five as fair and one as poor. The authors concluded that valgus osteotomy is a good option for treatment of pseudoarthrosis in the femoral neck fractures in children.
Keywords: Femur, Neck of femur, Hip, Fracture, Pseudoarthrosis, Osteotomy
Introduction
Fractures of the femoral neck in children and adolescents are not common [1]. They represent fewer than 1% of all the paediatric fractures [2]. However, complications accompanying these fractures are frequent—specifically avascular necrosis, pseudoarthrosis and early closure of the proximal physis of the femur—resulting in decrease of growth and coxa vara. The incidence of pseudoarthrosis varies from 7 to 10%, depending on the location of the fracture in the neck of femur [2–4].
Delbet was the first to describe the fractures of the femoral neck. He published the first classification in the French literature. Since then, Colonna [5] has quoted the Delbet classification, which is still accepted in all the literature regarding this subject, and Ratliff [2] has described the evaluation criteria of the results, based on the presence of pain, joint mobility and the child’s capacity to maintain a daily activity (Fig. 1).
Fig. 1.
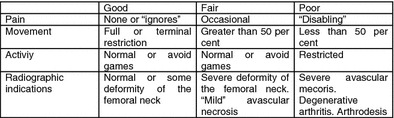
Ratliff’s concepts
The objective of this study was to prospectively evaluate the surgical results of pseudoarthrosis of the femoral neck treated by means of subtrochanteric femoral valgus osteotomy.
Materials and methods
From July 1992 to February 1998, nine of a series of patients, surgically treated at other medical centres for fractures of the femoral neck in the acute phase, were referred to our service to treat the pseudoarthroses that occurred as a consequence of these fractures. Male gender was slightly predominant in the ratio of five males to four females; seven patients were Caucasian and two were black; five pseudoarthroses occurred on the right side and four on the left. The mean age at diagnosis was 10 years 2 months, varying from 6 years 2 months to 14 years 2 months.
Of the nine patients, four (44.4%) initially underwent surgery involving fixation with threads and pins of different kinds, and then used a long leg cast (LLC). Three (33.3%) had been treated with screws and then a LLC; one (11.1%) underwent a closed reduction then used a LLC; and one (11.1%) had been treated with Coventry screw without immobilization.
The injuries causing the initial fractures were as follows: trampling in four patients (44.4%), bicycle fall in two (22.2%), car accident in two (22.2%) and direct fall in one (11.1%). Fractures were classified according to the Delbet's [5] methodology: type 1, physeal separation; type 2, transcervical; type 3, basicervical; and type 4, cervicotrochanteric. Using this classification system, five (55.5%) were classified as type II and four (44.4%) as type III.
The Ratliff’s classification [6] was used to identify avascular necrosis: type I, global avascular necrosis; type II, metaphyseal avascular necrosis; and type III, epiphyseal avascular necrosis. Avascular necrosis type II occurred in one patient (11.1%) and type III in five patients (55.5%).
All these data are described in Table 1.
Table 1.
Patients according to number, initials of the name, origin, register, gender, race, age in years and months, affected side, causing agent, type of fracture, previous treatment and type of necrosis
| Number | Name | Institution | Register | Gender | Race | Age (years and months) | Side | Causing agents | Type of fracture (DELBET) | Previous treatment | Type of necrosis (RATLIFF) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ECM | HSP | 743107 | Female | C | 11 + 4 | Right | Trampling | II | K wires + LLC | III |
| 2 | RJG | HSP | 909217 | Male | C | 6 + 2 | Right | Trampling | II | K Wires + LLC | II |
| 3 | LVF | ADJ | 12429 | Male | C | 13 | Right | Car accident | II | 2 Steinmann wires + LLC | III |
| 4 | TBF | PUCCamp | 528721356 | Female | C | 14 + 2 | Right | Bicycle fall | III | 2 Gouffon screws + LLC | – |
| 5 | WPD | IFOR | 066031 | Male | C | 7 + 6 | Right | Trampling | II | 2 Knowles screws + LLC | III |
| 6 | FSB | HSP | 86432 | Male | B | 6 + 9 | Left | Bicycle fall | II | K wires + LLC | – |
| 7 | JGR | PUCCamp | 515600369 | Female | C | 11 + 6 | Left | Direct fall | III | Cannulated screw + LLC | III |
| 8 | RLO | HSP | 74862 | Female | B | 7 + 6 | Left | Car accident | III | Closed reduction + LLC | – |
| 9 | JCR | CSSM | 0198223 | Male | C | 13 + 8 | Left | Trampling | III | Coventry screw without LLC | III |
The results of the treatment in relation to pain, movement, activities and radiographic alterations were evaluated as good, fair and poor according to the Ratliff’s concepts [2].
Surgical technique
Surgery was performed on the patient in the lateral decubitus position, with a 45° of inclination of the surgical table for such lateral approach. Subtrochanteric femoral valgus osteotomy was then performed according to the preoperative plan drawn on the radiography of each case, and it was approximately 30° in most of the cases combined with lateral resection of a bone wedge (Fig. 2a–g). Fixation was made with plates with different angulations: 120° (Fig. 2f, g) (cases 2, 3, 4, 6, 8 and 9); 95° (Fig. 3) (case 1), with screw compression for the femoral neck combined to a plate for diaphysis (Fig. 4) (cases 5 and 7). Angulation of 120° and 95° was chosen according to the femoral neck lesion and the age of the children, to avoid damage of the physes by the plate. Osteotomy compression was performed with an external compressor using the conventional technique. Capsulotomy and insertion of cancellous bone graft, obtained from the ipsilateral iliac, was packed around the fracture in three cases (1, 4, and 7) (Table 2).
Fig. 2.
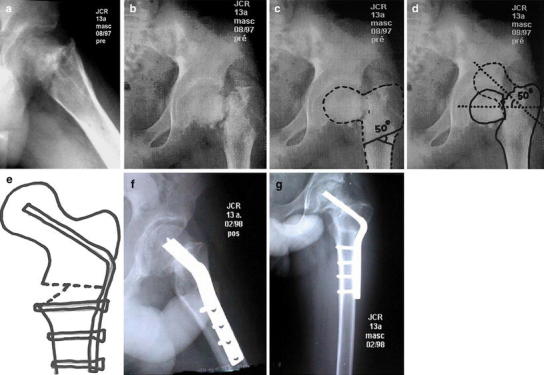
X-ray of the left hip, in Lauenstein position (a) and AP (b), showing nonunion, necrosis type III as RATLIFF, reabsorption area, varus deformity in a white, male, 13-year-old patient. c Planning of the osteotomy in the X-ray. d Design performed on the X-ray to calculate the lateral subtrochanteric wedge. e Scheme of the surgical planning. f–g Radiographs in two positions, seeing the callus formation by-passing the nonunion and the healed osteotomy
Fig. 3.
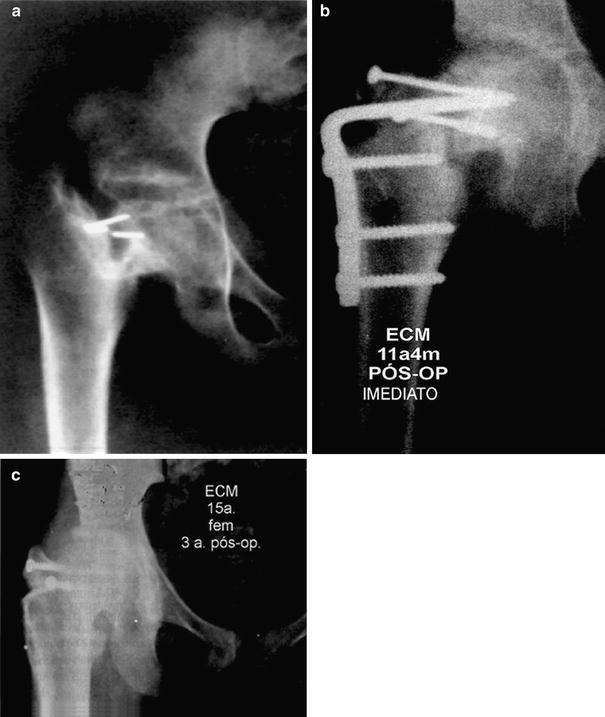
a X-ray of the right hip in frontal plane showing nonunion, necrosis type III as Ratliff, reabsortion area, varus deformity and small k. wire fragments. b Same patient after valgus osteotomy with plate fixed with 95° and two screws fixing the horizontal position of pseudoarthrosis. c X-ray after the remotion of the plate with consolidation obtained and good articular congruence
Fig. 4.
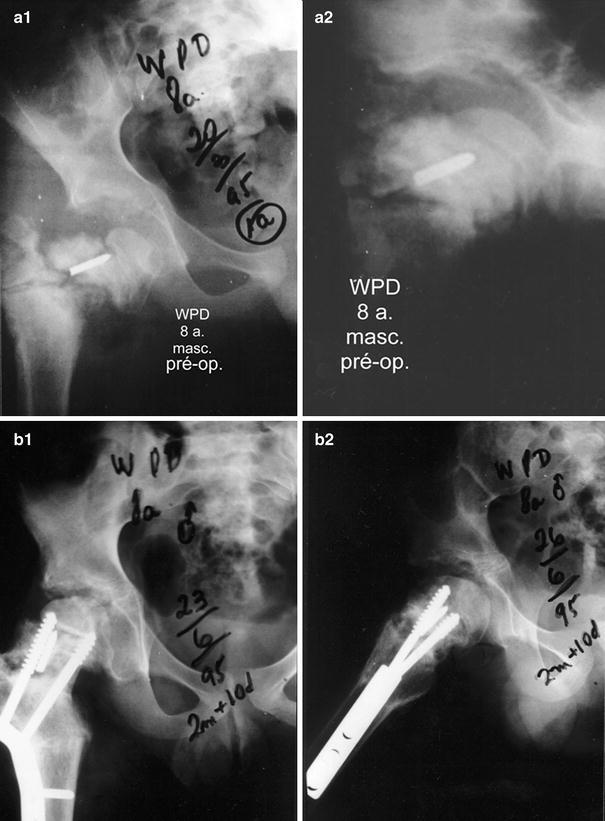
a X ray of the right hip, in frontal and lateral planes, showing nonunion, necrosis type III as RATLIFF, reabsortion area, varus deformity and a small fragment of screw. b Same patient’s pictures in frontal and lateral planes, taken 70 days after osteotomy, fixed by molded plate and healed
Table 2.
Patients according to number, surgery, time of consolidation (days), complications, procedure, shortening, follow-up (months), RATLIFF’s functional evaluation, Rfunctional evaluation. VO valgus osteotomy, PL plate, LLC long leg cast
| Number | Surgery | Time of consolidation (days) | Complications | Procedure | Shortening (cm) | Follow-up (months) | RATLIFF’s functional evaluation |
|---|---|---|---|---|---|---|---|
| 1 | VO + PL 95° + bone graft + LLC + 2 screws | 48 | Epiphysiodesis | Expectant | 3 | 71 | Fair |
| 2 | VO + PL 120° + LLC | 68 | – | – | 0 | 57 | Fair |
| 3 | VO + Pl 120° | 60 | Necrosis type 2 + epiphysiodesis | Expectant | 4 | 28 | Poor |
| 4 | 07/94: VO + PL 120° 09/94: Bone graft + LLC | 240 | Delayed | Posterior bone graft | 1 | 24 | Good |
| 5 | VO + DCP + LLC Plate + screws | 70 | Epiphysiodesis | Expectant | 1 | 44 | Fair |
| 6 | VO + PL 120° + LLC | 45 | – | – | 0 | 38 | Good |
| 7 | 05/95: VO + 06/95: DCP + + bone graft + LLC + Plate + screws | 56 | Epiphysiodesis | 2 | 36 | Fair | |
| 8 | VO + PL 120° + LLC | 45 | – | – | 0 | 29 | Good |
| 9 | VO + PL 120° | 58 | Epiphysiodesis | Expectant | 3 | 23 | Fair |
The spica cast allowed us to immobilize the hip joint with flexion of 15°, abduction of 15° and neutral rotation.
Control radiographs were performed every 2 weeks until healing of the pseudoarthrosis. The plaster cast was removed after 6 weeks, according to the radiographic control. A rehabilitation program was performed according to the age of the patient and the radiographic evaluation of the healing process of osteotomy and nonunion. Gait with partial weight bearing was allowed in all cases under the supervision of a physiotherapist. Gait with full load was allowed only after consolidation of pseudoarthrosis, confirmed by a radiographic check-up (average 76.6 days).
Results
According to the Ratliff’s concept [2], three patients (33.3%) (no. 4, 6 and 8) were assessed as having a good result, five (55.5%) as fair (1, 2, 5, 7 and 9) and one (11.1%) (3) as poor. The follow-up was from 23 to 71 months, with a mean of 36.6 months. Full healing, varying from 45 to 240 days, with a mean of 76.6 days, was obtained in all the patients.
Complications
In one patient (no. 4), a re-do surgery was needful due to a delay in the consolidation process, and then a new bone graft was performed. Late necrosis was observed in one patient (no. 3), with no final impairment of the function of the hip until the last clinical and radiographic examination. Closure of the proximal physeal plate (epiphysiodesis) was observed in five patients (no. 1, 3, 5, 7 and 9). Six patients (66.6%) underwent residual shortening: in two cases (no. 1 and 9) 3.0 cm; in one (no. 3) 4.0 cm; in one (no. 7) 2.0 cm; and in two (no. 4 and 5) 1.0 cm. The data of final results are presented in Table 2.
Discussion
Fractures of the femoral neck are considered rare entities [1, 7], but their complications are many [8, 9]. In our short series, five of the nine cases of pseudoarthrosis occurred in transcervical fractures and four in basicervical fractures (Table 1). Lam [10], Forlin et al. [11] and Hughes and Beauty [12] also reported such incidences. The predominance of pseudoarthrosis might be directly related to the difficulty to maintain stability of the fractures during treatment, since they present an oblique aspect and, consequently, a high degree of instability. In our opinion, another cause of the pseudoarthrosis is probably due to the type of synthesis material used in the first surgery (threaded pins and K wires), which did not allow good stability of the fracture, despite immobilization being achieved with a plaster cast [11]. The high-energy trauma (trampling, bicycle falls, car accidents and direct fall) also has to be considered as a factor of pseudoarthrosis of the femoral neck, which is in accordance with studies reported in the literature [1, 8, 9, 13, 14].
Another important cause of pseudoarthrosis is related to local vascularization that is altered or damaged by the duration of the trauma, leading to some nutritionally deficient epiphyseal vessels, causing avascular necrosis of the neck of the femur. This is consistent with studies by Ingram [9] and Durbin [15]. McDougall [16] advocates care in the reduction and manipulation procedures to avoid damage to the vessels of the femoral neck. The major circulatory pattern found in the epiphysis in children and adolescents with the opened physeal plate is performed by the lateral epiphyseal artery, which is a branch of the medial femoral circumflex artery [17, 18]. The physeal plate, in patients in this age range, constitutes an impassable barrier for the metaphyseal circulation [18, 19]; so, the lateral epiphyseal vessels are practically the only way to maintain nutrition to the proximal neck and femoral head [19]. Sotto-Hall et al. [20] mentioned the need for an articular punction of the haematoma during the first surgery to decrease intracapsular pressure and avoid collapse of the epiphyseal vessels. Drake and Meyers [21] suggested, in their studies, that this is a needless procedure; we fully agree with them.
With regard to the surgical treatment, according to the Pauwels concept [22], when the deformity is fixed, transforming the shearing forces of pseudoarthrosis in compression and performing mechanical stabilization, the pseudoarthrosis heals most of the time, as in our series with only one case of delay in the consolidation. This was also observed by Forlin et al. [11] and Touzet et al. [23]. The angulated fixed nail-plate induces dynamic compression forces; the use of screws leads merely to a static compression.
When considering race as a factor, seven cases of pseudoarthrosis of the femoral neck occurred in Caucasian (77.7%) and two (22.2%) in black patients, but the low number of cases did not allow us to conclude any predominant racial influence. Nevertheless, Miller [1], in his series of 39 patients (25 Caucasian and 14 black), mentioned that there might be a racial influence in the circulation of the neck of the femur to justify the greater incidence of poor and fair results in white people. Trueta [24], in 1968, studying the vascularity of six South African Bantu children and three Brazilian black, verified that “the vessels from the teres ligament were seen to be anastomosed to the lateral epiphyseal vessels and to the few vessels still remaining from the surface of the metaphysic”. This fact suggests that “before the age of 6 years, the black child should be less exposed to ischaemic changes of the femoral epiphysis than the child of European stock.”
Closure of the femoral physis, observed in five of our cases (no. 1, 3, 5, 7 and 9—Table 2), despite being an important complication, did not interfere with the healing of the pseudoarthrosis after appropriate surgical treatment. The occurrence of an epiphysiodesis allows use of a longer nail which induces a better stabilization of the osteotomy [8].
Conclusion
The mechanical stabilization obtained with valgus osteotomy of the proximal femur is important to consolidate pseudoarthrosis.
Necrosis of the femoral neck (type III), when associated with pseudoarthrosis, does not interfere in the healing when stabilized by the subtrochanteric femoral valgus osteotomy.
Such an osteotomy as part of the primary surgical treatment may prevent the occurrence of pseudoarthrosis.
Acknowledgments
The authors thank Sheila Ribeiro de Campos Solla for helping to correct the manuscript.
References
- 1.Miller WE. Fractures of the hip in children from birth to adolescence. Clin Orthop Relat Res. 1973;92:155–187. doi: 10.1097/00003086-197305000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Ratliff AHC. Fractures of the neck of the femur in children. J Bone Joint Surg Br. 1962;44:528–542. doi: 10.1302/0301-620X.44B3.528. [DOI] [PubMed] [Google Scholar]
- 3.Chrestian P, Bollini G, Jacquemier M, Ramaherison P. Fractures du col du femur de lénfant. Chir Pediatr. 1981;22:397–403. [PubMed] [Google Scholar]
- 4.Ratliff AHC. Complications after fractures of the femoral neck in children and their treatment. J Bone Joint Surg Br. 1970;52:175–183. [Google Scholar]
- 5.Delbet cited by Colonna PC (1929) Fractures of the neck of the femur in children. Am J Surg 6:793–797
- 6.Ratliff AHC. Traumatic separation of the upper femoral epiphysis in young in young children. J Bone Joint Surg Br. 1968;50:757–770. [PubMed] [Google Scholar]
- 7.Rang M. Children’s fractures. 2nd edn. Philadelphia: J B Lippincott; 1983. [Google Scholar]
- 8.Canale ST, Bourland WL. Fracture of the neck of the femur and intertrochanteric region of the femur in children. J Bone Joint Surg Am. 1977;59:431–443. [PubMed] [Google Scholar]
- 9.Ingram AJ, Bachynski B. Fractures of the hip in children. J Bone Joint Surg Am. 1953;35:867–886. [PubMed] [Google Scholar]
- 10.Lam SF. Fractures of the neck of the femur in children. J Bone Joint Surg Am. 1971;53:1165–1179. [PubMed] [Google Scholar]
- 11.Forlin E, Guille BA, Kumar SJ, Rhee KJ. Complications associated with fracture of the neck of the femur in children. J Pediatr Orthop. 1992;12:503–509. doi: 10.1097/01241398-199207000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Hughes LO, Beaty JH. Fractures of the head and neck of the femur in children. J Bone Joint Surg Am. 1994;76:283–291. doi: 10.2106/00004623-199402000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Colonna PC. Fracture of the neck of the femur in childhood. Ann Surg. 1928;88:902–907. doi: 10.1097/00000658-192811000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiner DS, O’dell HW. Fractures of the hip in children. J Trauma. 1969;9:62–79. doi: 10.1097/00005373-196901000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Durbin FC. Avascular necrosis complicating undisplaced fractures of the neck of the femur in children. J Bone Joint Surg Br. 1959;41:758–765. doi: 10.1302/0301-620X.41B4.758. [DOI] [PubMed] [Google Scholar]
- 16.McDougall A. Fractures of the neck of the femur in childhood. J Bone Joint Surg Br. 1961;43:16–28. [Google Scholar]
- 17.Ogden JA. Changing patterns of proximal femoral vascularity. J Bone Joint Surg Am. 1974;56:941–50. [PubMed] [Google Scholar]
- 18.Trueta J. The normal vascular anatomy of the human femoral head during growth. J Bone Joint Surg Br. 1957;39:358–373. doi: 10.1302/0301-620X.39B2.358. [DOI] [PubMed] [Google Scholar]
- 19.Chung SMK. The arterial supply of the developing proximal end of the human femur. J Bone J Surg Am. 1976;58:961–970. [PubMed] [Google Scholar]
- 20.Sotto-Hall R, Johnson LH, Johnson RA. Variations in the intra-articular pressure of the hip joint in injury and disease. J Bone Joint Surg Am. 1964;46:509–516. [PubMed] [Google Scholar]
- 21.Drake JK, Meyers MH. Intracapsular pressure and hemartrosis following femoral neck fracture. Clin Orthop Relat Res. 1984;182:172–175. [PubMed] [Google Scholar]
- 22.Pauwels F. Biomechanics of the locomotor apparatus. English edn. New York: Springer; 1965. [Google Scholar]
- 23.Touzet P, Rigault P, Padovani JP, Pouliquen JC, Mallet JF, Guyonvarch G. Fractures of the neck of the femur in children. Rev Chir Orthop Reparatrice Appar Mot. 1979;65:341–349. [PubMed] [Google Scholar]
- 24.Trueta J. Studies of the development decay of the human frame, 2nd ed. Philadelphia: J. B. Lippincott; 1968. Vascular pattern of the femoral head during growth. [Google Scholar]


