Abstract
Background
The standard treatment of adolescent Blount disease includes proximal tibial osteotomy and osteotomy of the fibula. Some believe that the fibula should also be fixed to prevent migration and subluxation. The purpose of the current study was to examine the results of treatment of patients with adolescent tibia vara treated by tibial osteotomy and Taylor spatial frame (TSF) without fibular osteotomy.
Methods
Correction of deformities was performed on eight patients (ten tibias) with adolescent Blount disease using TSF. The fibula was not osteotomized in any patient and was not fixed in the last five patients.
Results
All patients had precise anatomical correction of deformities and no problems related to the fibula occurred during or after correction.
Conclusion
Based on our experience we believe that placement of the origin at the level of the proximal tibial fibular joint in conjunction with external fixation eliminates the need for fibular osteotomy and the potential morbidity of this procedure in patients with mild to moderate tibia vara.
Keywords: Adolescent Blount’s disease, Fibular osteotomy, Tibia vara, Tibial osteotomy
Introduction
Adolescent Blount disease, also known as late-onset tibia vara, is a common disorder in the second decade of life. Patients present with marked genu varum secondary to proximal tibial varus, and some also have combined depression of the medial tibial plateau [1, 2]. Posteromedial tibial growth suppression is responsible for both tibia vara and proximal tibal procurvatum, and many patients also have internal tibial torsion. The combination of three deformities in different planes (varus, procurvatum, and internal tibial torsion) results in a complex three-dimensional deformity [2]. Nonoperative treatment is ineffective for late-onset tibia vara [3]. Treatment options include lateral hemi-epiphysiodesis of the proximal tibia, physeal distraction, and tibial osteotomy using internal or external fixation. Proximal tibial valgus osteotomy and osteotomy of the fibula using external fixation is currently the gold standard in the treatment of late-onset tibia vara [1, 2, 4–7]. The Taylor spatial frame (TSF) is a relatively new external fixation device, able to correct a six-axis deformity by using a virtual hinge. Taylor suggested that, in patients with Blount disease, all deformities can be corrected without fibular osteotomy by placing the origin at the level of the proximal tibial fibular joint [8]. The purpose of this study is to report the treatment outcome of proximal tibial osteotomy without osteotomy of the fibula in patients with adolescent Blount disease.
Patients and methods
During a 3-year period from 01/03/2003 to 01/03/2006, we treated ten tibias in eight consecutive patients with adolescent Blount disease. All patients were boys with a mean age of 14.6 years (range 14–17 years). Two patients had bilateral involvement and were treated bilaterally. The pertinent data for the patients are shown in Table 1.
Table 1.
Patient characteristics
| Pt | Age (years) | MPTA pre/postop. (degrees) | PPTA pre/postop. (degrees) | MAD pre/postop. (mm) | Rotational correction (degrees) | Axial translation (shortening) (mm) | Distal fibular fixation | Fixation time (weeks) | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1. | 14 | 72/86 | 71/77 R | 65/4 | 15 ITT | 18 | Yes | 12 | Bleeding after injury of genicular artery by half-pin; superficial pin infection |
| 2. | 17 | 68/88 R72/87 L | 81 R79 L | 74/11 R57/4 L | None | 10 R10 L | Yes | 1412 | Superficial pin infection |
| 3. | 13 | 77/89 | 74/77 L | 45/3 | 10 ITT | 14 | Yes | 12 | |
| 4. | 14 | 72/88 | 70/77 L | 44/5 | 10 ITT | 22 | No | 15 | Superficial pin infection |
| 5. | 15 | 67/86 | 78/81 | 71/2 | 10 ITT | 16 | No | 12 | Superficial pin infection |
| 6. | 13 | 74/89 R73/85 L | 68/80 R72/77 L | 51/3 R62/5 L | 10 ITT5 ITT | 20 R16 L | Yes | 12 R14 L | Superficial pin infection |
| 7. | 14 | 71/86 | 77/78 | 52/4 | None | 14 | No | 12 | Superficial pin infection |
| 8. | 17 | 68/87 | 81/81 | 77/6 | 10 ITT | 15 | No | 13 | Superficial pin infection |
ITT internal tibial torsion, PPTA posterior proximal tibial angle, MPTA medial proximal tibial angle, MAD mechanical axis deviation
Preoperatively, all patients were evaluated radiographically by long standing radiograms, and deformities were analyzed according to the principles outlined by Paley [9]. On the long antero-posterior view, we recorded leg length discrepancy (LLD), mechanical axis deviation (MAD), lateral distal femoral angle (LDFA), and medial proximal tibial angle (MPTA). Lateral standing radiograms were performed for the measurement of posterior proximal tibial angle (PPTA). Rotations were measured clinically by thigh-foot angle and position of the foot relative to an imaginary line from the center of the patella and second toe of the foot.
Operative technique and TSF preplanning
The patient was placed in the supine position, with a bump under the buttock on the affected side. We start by passing a strong suture just below the tibial tubercle for the later pass of the Gigli saw [9]. For easier knee flexion, we use a 2/3 ring open posterior proximally and a full ring connected by six struts distally. The reference ring should be aligned perfectly orthogonal to the axis of the corresponding tibial fragment and parallel to the anterior plane of the bone in order to eliminate rotational offset. We fixed the proximal ring by two 6 mm half-pins and a 1.8 Ilizarov wire, and distally by three half-pins and one wire. After completion of the fixation and application of all six struts, two anterior struts were removed to allow completion of the proximal tibial osteotomy by Gigli saw. In the first three patients, the fibulas were fixed distally by two 1.8 Ilizarov Kirshner wires fixed to a third ring just above the ankle joint. In all the other patients, the distal fibula was not transfixed to the tibia, and none of the patients had any proximal fibular fixation. The center of the reference ring was marked by two long bolts on the antero-posterior and lateral views for easier determination of mounting parameters. Long tibial X-rays were performed in the operating room.
The TSF was used in the total residual program. TSF preplanning included calculation of three groups of parameters: deformity, mounting, and frame. For a detailed explanation of the method, the reader is referred to the original description [8]. In general, deformity parameters show the relationship between the origin and the corresponding points calculated based on preoperative X-rays. The origin is defined as the point on the reference fragment, and the corresponding point is defined as the point on the moving fragment. The origin was located along the mechanical axis of the reference fragment—the proximal fragment in our patients—while corresponding points were located on the mechanical axis of the moving distal fragment (Fig. 1a, b). In all patients, the origin was placed at the level of the proximal tibial fibular joint. The corresponding point on AP and lateral views was determined according to the distance from the origin to the proximal tibial fibular joint (Fig. 1a, b). Deformity parameters included antero-posterior and lateral views of angulation and translation, axial view angulation, and axial translation (which determine shortening or lengthening of the given case). Rotational deformity is determined by clinical examination. Mounting parameters reflect the relationship between the reference ring (the ring applied to the reference fragment) and the origin. Because the proximal fragment was chosen as the reference fragment, the proximal ring was the reference ring in all patients. Frame parameters define information on the diameters of the rings and lengths of the struts. Lastly, the surgeon chooses the structure at risk (the structure which will undergo the most risky elongation during deformity correction) and safe velocity correction (usually about 1 mm per day). In all our patients, the medial cortex of the osteotomy of the tibia was chosen as the structure at risk (during correction of the varus to valgus, no nerve structure underwent elongation, which is why we used the posterior medial cortex of the tibia as the structure at risk).
Fig. 1.
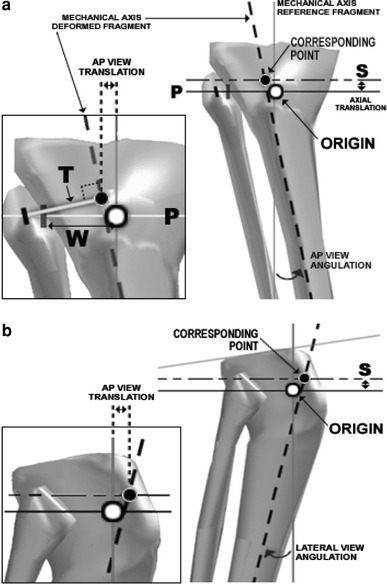
a, bDetermination of the deformity parameters on the AP and lateral view (Ref. [8], with permission). In order to perform correction without fibula osteotomy: origin placed along the mechanical axis of the reference fragment (proximal tibia) at the level of the proximal tibial fibular joint. W distance from the origin to the proximal fibula. Corresponding point: located on the mechanical axis of the distal deformed fragment. To determine the corresponding point distance, T (equal distance to W) should be placed perpendicular to the mechanical axis of the deformed fragment. S axial translation (shortening of the given case)
All patients began struts adjustments after the 6th postoperative day with velocity correction of 1–1.5 mm daily. Physiotherapy was started on the morning after surgery, and early weight-bearing was encouraged in all patients. After radiological confirmation of union at the osteotomy site, dynamization of the frame was achieved by struts release and partial removal of wires/pins (Fig. 2c).
Fig. 2.

a–f Fourteen-year-old with left Blount disease. a Clinical picture before treatment. b X-ray before treatment. c Clinical picture shortly before frame removal (12 weeks from treatment). Note that frame is dynamized by partial removal of half-pins and Kirshner wires. d, e AP and lateral standing views 28 months after surgery. f Clinical picture 20 months after surgery
Results
Mean follow-up was 3.7 years (range 2.1–4.1 years). The mean preoperative proximal tibial varus was 16.2° (range 12–19°), and was corrected to normal values in all patients. Mean preoperative MPTA was 71.4° (range 67–77°), and was corrected to a mean of 87.1° (range 85–89°). Mean preoperative PPTA was 75.1° (range 68–81°). In four patients (five tibias) with a proximal tibial procurvatum, the PPTA was corrected to normal ranges. The mean correction of internal tibial torsion was 10° (range 5–15°) performed in six patients (eight tibias). Preoperative MAD was 55.8 mm medial to the center of the knee (range 44–77 mm) and was corrected to a mean of 4.9 mm (range 2–11 mm). Five patients had mild distal femoral varus with a slightly abnormal LDFA (mean 92°, range 88–93°). Two patients were treated by concomitant lateral distal femoral stapling. Frames were removed at an average of 12.8 weeks (range 12–15 weeks). We did not find any displacement of the tibio-fibular joint, neither distally nor proximally. There was no recurrence of deformity and all patients had full range of motion with no limitation of functional activity at the latest follow-up visit.
Complications included superficial tract infections in seven patients (nine tibias), and bleeding after injury of the genicular artery by half-pin, which resolved upon pin replacement. There were no neurological complications, delayed unions, or non-unions. No complications related to the fibula were observed during and after correction.
Discussion
The treatment goal in adolescent Blount disease is correction of the mechanical axis to prevent development of medial knee compartment osteoarthrosis [10]. Various methods of correction and different osteotomies have been used to correct tibial deformities. Acute and gradual corrections by internal and external fixations have been described [1, 2, 4–7, 11]. Most patients with adolescent Blount disease are obese, and have a relative contraindication to internal fixation due to increased complication rates [2, 7, 18]. External fixation has certain advantages in these patients, allowing excellent stability and early weight-bearing. Monolateral and circular fixators have been described with good final results [1, 7].
The Taylor spatial frame is a relatively new external fixator that allows six-axis correction of most complex deformities with computer accuracy [5, 8, 11]. Late-onset tibia vara or adolescent Blount disease is a complex three-dimensional deformity [2] which includes proximal tibial varus deformity, proximal tibial procurvatum, and internal tibial torsion. The TSF is able to correct varus, procurvatum, and internal tibial torsion simultaneously in the same frame without a need for hinge placement and frame modification. We found only one paper that described correction of tibia vara by TSF [5]. Feldman et al. reported their experience in 19 patients (22 tibias) with infantile and adolescent tibia vara. The authors corrected 21 of 22 tibias within 3° of normal. Fibular osteotomy was performed in 17 of 22 cases.
Many believe that disruption of the strutting effect of the fibula is crucial to achieving correction in patients with proximal tibial varus. Excision of the fibular head and a segment of the fibular diaphysis are both commonly described [12]. This approach caused seven peroneal nerve palsies in 42 osteotomies [13]. Taylor suggested that correction of Blount’s deformities with varus and rotation, the tibial malalignment, malrotation, and malposition may be corrected without fibular osteotomy. Only in deformities with varus, rotation, and significant procurvatum (when the procurvatum is greater than the varus) should the fibula should be osteotomized according to Taylor [8]. “If no additional fibular length is needed most tibial deformities can be corrected with fixing or osteotomizing the fibular.” In order to achieve correction of the proximal tibial deformity, the origin should be placed at the level of the proximal tibial fibular joint. The concept of proximal tibia vara correction by tibial osteotomy with preservation of the fibula by placing Ilizarov hinges at the level of the proximal tibial fibular joint was described earlier [14], but the current standard correction of proximal tibial varus deformities includes proximal tibial osteotomy and fibular osteotomy on various levels [1, 2, 5–7, 15].
Taylor suggested that, when no additional fibular length is needed, most tibial deformities can be corrected without fixing and osteotomizing of the fibula [8]. We did not fix the fibular in the last five of our patients and had uniformly good results with no problems related to fibular length and subluxation of the fibula. Also, while correction of the tibial length may theoretically change tibio-fibular relations, we did not found this in our patients, probably because of the small and gradual tibial lengthening.
Neurovascular complications are a potential risk of fibular osteotomy. The rate of peroneal nerve palsy depends on the level of the fibular osteotomy. Peroneal nerve palsy related to the fibular osteotomy varies from none to 20% [16]. Wootton et al. [17] found motor weakness and/or sensory deficit in 21 patients (20%) of 118 proximal tibial osteotomies; in half of these patients the neurological deficit was permanent. The authors concluded that the neurological deficit was related to the level of the fibular osteotomy and, based on their cadaver studies, recommended that fibular osteotomy should not be performed at the level from just below the fibular head to 15 cm distal to this level.
Two studies identified a danger zone for the fibular osteotomy: between 6 and 13 cm distal to the head of the fibula where the nerve to the extensor hallucis longus lies close to the fibula [13, 20]. Rupp at al. analyzed potential neurovascular risk structures with respect to the fibular osteotomy. At the proximal one-third of the fibula, the peroneal nerve and its muscular branches are a primary risk; the peroneal nerve artery and vein are at risk in the middle third of the fibula, and only the distal third is a relatively safe zone [19]. Common practice in tibial deformity correction is subperiostal excision of 1 cm of fibula through a lateral incision at the junction of the middle and distal third of the fibular shaft but, even when performed at this ‘safe’ level, there are reports of injury to the superficial peroneal nerve at the site of the peroneal nerve and EHL palsy [6].
The weak point of this study is the relatively small cohort of patients. However, our early results are encouraging and, based on these, we believe that correction of proximal tibial varus in patients with adolescent Blount disease can be achieved without fibular osteotomy, eliminating the potential risks of this procedure.
Conclusion
According to our initial experience, we believe that most patients with adolescent Blount disease could have successful and predictable correction of mild to moderate tibial deformities without a need for osteotomy and fixation of the fibula.
Acknowledgments
The authors thank Dr. J. Charles Taylor for permission to use illustrations from his website. We also thank Mrs. M. Perlmutter for her help in the preparation of this paper.
Reference
- 1.Alekberov C, Shevtsov VI, Karatosun V, et al. Treatment of tibia vara by the Ilizarov method. Clin Orthop Relat Res. 2003;409:199–208. doi: 10.1097/01.blo.0000052937.71325.a2. [DOI] [PubMed] [Google Scholar]
- 2.Gordon JE, Heidenreich FP, Carpenter CJ, et al. Comprehensive treatment of late-onset tibia vara. J Bone Joint Surg Am. 2005;87:1561–1570. doi: 10.2106/JBJS.02276. [DOI] [PubMed] [Google Scholar]
- 3.Park SS, Gordon JE, Luhmann SJ, et al. Outcome of hemiepiphyseal stapling for late-onset tibia vara. J Bone Joint Surg Am. 2005;87:2259–2266. doi: 10.2106/JBJS.C.01409. [DOI] [PubMed] [Google Scholar]
- 4.Coogan PG, Fox JA, Fitch RD. Treatment of adolescent Blount disease with the circular external fixation device and distraction osteogenesis. J Pediatr Orthop. 1996;16:450–454. doi: 10.1097/01241398-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Feldman DS, Madan SS, Koval KJ, et al. Correction of tibia vara with six-axis deformity analysis and the Taylor spatial frame. J Pediatr Othop. 2003;23:387–391. [PubMed] [Google Scholar]
- 6.Dilawaiz Nadeem R, Quick TJ, Eastwood DM. Focal dome osteotomy for the correction of tibial deformity in children. J Pediatr Orthop B. 2005;14:340–346. doi: 10.1097/01202412-200509000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Smith SL, Beckish ML, Winters SC, et al. Treatment of late-onset tibia vara using Afghan percutaneous osteotomy and orthofix external fixation. J Pediatr Othop. 2000;20:606–610. doi: 10.1097/01241398-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Taylor JC Correction of general deformity with Taylor spatial frame. http://www.jcharleystaylor.com Accessed February 2008
- 9.Paley D. Principles of deformity correction. Berlin: Springer; 2002. [Google Scholar]
- 10.Brooks WC, Gross RH. Genu varum in children: diagnosis and treatment. J Am Acad Orthop Surg. 1995;3:326–335. doi: 10.5435/00124635-199511000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor spatial frame. J Pediatr Orthop B. 2006;15:387–395. doi: 10.1097/01.bpb.0000228380.27239.8a. [DOI] [PubMed] [Google Scholar]
- 12.Billings A, Scott DF, Camargo MP, Hofmann AA High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion. Long-term follow-up. J Bone Joint Surg Am. 2000;82:70–79. Erratum in: J Bone Joint Surg Am. 2000;82:450 [DOI] [PubMed]
- 13.Kirgis A, Albreicht S. Palsy of the deep peroneal nerve after proximal tibial osteotomy: an anatomical study. J Bone Joint Surg Am. 1992;74:1180–1185. [PubMed] [Google Scholar]
- 14.Catagni MA, Guerreschi F, Ahmad TS, Cattaneo R. Treatment of genu varum in medial compartment osteoarthritis of the knee using the Ilizarov method. Orthop Clin North Am. 1994;25:509–514. [PubMed] [Google Scholar]
- 15.Hatzokos I, Drakou A, Christodoulou A, et al. Inferior subluxation of the fibular head following tibial lengthening with a unilateral external fixator. J Bone Joint Surg Am. 2004;86:1491–1496. doi: 10.2106/00004623-200407000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Wright JM, Crockett HC, Slawski DP, et al. High tibial osteotomy. J Am Acad Orthop Surg. 2005;13:279–289. doi: 10.5435/00124635-200507000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Wootton JR, Ashworth MJ, MacLaren CA. Neurological complications of high tibial osteotomy—the fibular osteotomy as a causative factor: a clinical and anatomical study. Ann R Coll Surg Engl. 1995;77:31–34. [PMC free article] [PubMed] [Google Scholar]
- 18.Henderson RC. Tibia vara: a complication of adolescent obesity. J Pediatr. 1992;121:482–486. doi: 10.1016/S0022-3476(05)81811-6. [DOI] [PubMed] [Google Scholar]
- 19.Rupp RE, Podeszwa D, Ebraheim NA. Danger zones associated with fibular osteotomy. J Orthop Trauma. 1994;8:54–58. doi: 10.1097/00005131-199402000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Elgafy H, Ebraheim NA, Shaheen PE, Yeasting RA. Extensor hallucis longus innervation: an antomic study. Clin Orthop Relat Res. 2002;398:245–251. doi: 10.1097/00003086-200205000-00034. [DOI] [PubMed] [Google Scholar]


