Abstract
Purpose
Therapy of vitamin D-resistant hypophosphatemic rickets (VDXLR) consists of oral phosphate and vitamin D supplements. Bone deformities, pain, and small stature can occur even in children with good compliance, requiring surgical correction and bone lengthening. However, only few surgical reports are available.
Methods
Twelve patients (three males) with VDXLR were followed at our institution. Median age at diagnosis was 3 9/12 years (range, birth to 11 10/12) with a follow-up period of 7 8/12 years (1 9/12–30) and age at last follow-up of 13 6/12 years (2–30). Eight patients underwent surgical correction, three of them in combination with bone lengthening. The corrections were performed at the end of growth in three patients. Clinical endpoints were height, leg axis, and pain.
Results
Single bilateral surgical correction was performed in six patients; one patient each had three and five corrections. Bone lengthening was performed in three patients. At last follow-up, the height of seven operated patients was within normal range. In addition, leg axis was normalized in six patients with mild genua vara in two. Only one patient complained of intermittent pain. Bone healing was excellent; surgical complications were rare. There was no radiological evidence of degenerative arthropathy.
Conclusions
Medical treatment remains the main pillar of therapy in children with VDXLR. In case of bone deformity, surgery can safely be performed, independent of age or bone maturation. All patients were satisfied with the results of axial corrective surgery and bone lengthening, and in the majority only one corrective intervention was needed.
Keywords: Rickets, Correction, Axis, Lengthening, Growing children
Introduction
The X-linked vitamin D-resistant hypophosphatemic rickets (VDXLR) is a metabolic disorder first described by Albright et al. [1] in 1937. Clinical features, presenting with beginning of walking, include short stature, reduced growth rate, and bone deformity, such as coxa vara, femoral and crural bowing, and genua vara and valga [1–3] (Fig. 1a–c). Medication treatment consists of oral phosphate substitution and supplementation of active vitamin D compounds [2–6]. Despite correct substitution the main symptoms, i.e., deformity, pain, small stature, and—in some cases—also fractures can occur.
Fig. 1.

a–c Severe radiological deformities of the lower extremities of patient 1 at his first consultation
In case of drug-resistant deformity, operative procedures to correct bone deformities may be indicated for prevention of secondary complications, i.e., pain and degenerative arthropathy, or for cosmetic reasons.
Different problems related to surgical correction were reported. Some authors observed an increased rate of non-union in growing children if medical treatment was insufficient [6, 7], whereas in adult patients with a mature skeleton the healing rate after osteotomy was unremarkable [5].
Further problems for surgical correction included both the difficulty of the three-dimensional correction and the type of the osteosynthesis. Almost all available standard implants were used, and different numbers of osteotomies were performed [3, 5–11]. The choice of implant depended on the bone maturity of the patient and on surgeons’ preference. Most authors proposed surgery at or close to bone maturity because of the risk of recurrence of bone deformity and the risk of non-union in growing bones [5–7, 10].
Bone lengthening is an option in patients with short stature. The experience in patients with hypophosphatemic rickets is scarce, with only two cases reported by Dudkiewicz [12]. One patient had lengthening close to maturity with good outcome; the result of the other still growing, yet uncooperative patient was poor. Song et al. [11] presented a large study with different techniques such as distraction osteogenesis with external fixator with and without intramedullary nailing. They reported complications such as recurrent deformity, joint stiffness, deep intramedullary infection, refracture, nerve palsy, leg length discrepancy, and pin tract infection.
The aim of our study was to review our patients with VDXLR with the focus on those patients undergoing surgery, in particular lengthening procedures. The main parameters of interest were growth, height, axis of the lower limbs, pain, and degenerative arthropathy.
Materials and methods
We retrospectively analyzed the medical records of 12 patients (9 females, 3 males) with VDXLR. The first patient has been followed since 1976. Four patients were only on medical treatment, and eight patients also underwent surgery, including three patients with lengthening procedures. The diagnosis was based on the typical laboratory findings of hypophosphatemia, elevated alkaline phosphatase level, and normal parathyroid hormone serum concentration before treatment. Florid rickets, i.e., radiological evidence of rickets, lower limb deformity, or swollen metaphysis of the wrist and ankle in the physical examination, was not mandatory.
All patients received daily oral phosphate (50–100 mg/kg, maximal dose 2 g) and calcitriol (0.01–0.05 μg/kg). Table 1 shows the laboratory level of calcium, phosphorous, parathormon, and calcitriol. Height was correlated to normative Swiss data (age- and sex-related growth charts: centiles); the axis and deformity of the lower limbs were noted by physical examination. Pain and drug compliance were recorded. Plain X-rays were only ordered in case of florid rickets or suspected degenerative joint alteration. Bone maturity was defined according to bone age (X-ray of hand and wrist).
Table 1.
Pre- and postoperative laboratory levels and medication
| Patient | Calcium (mmol/l) | Phosphorous (mmol/l) | Parathormon (pg/ml) | Calcitriol (μg/day) | Phosphorous (mg/day) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Postopa | Preop | Postopa | Preop | Postopa | Preop | Postopa | Preop | Postopa | |
| 1 | 2.28 | 2.28 | 0.86 | 0.74 | 21 | 37 | 1 | 1.5 | 2,000 | 2,500 |
| 2 | 2.43 | 2.28 | 1.02 | 0.68 | 15 | 19 | 0.5 | 1 | 1,000 | 750 |
| 3 | 2.25 | 2.18 | 0.52 | 0.48 | 72 | 71 | 1.5 | 1.5 | 2,000 | 2,000 |
| 4 | 2.18 | 2.19 | 0.63 | 0.81 | 51 | 35 | 1 | 1 | 750 | 900 |
| 5 | 2.56 | 2.54 | 0.99 | 1.37 | 37 | 7 | 1 | 0.5 | 1,500 | 1,500 |
| 6 | 2.23 | 2.21 | 0.88 | 0.91 | 50 | 43 | 1 | 1 | 1,500 | 1,500 |
| 7 | 2.3 | 2.29 | 0.87 | 0.93 | 45 | 41 | 1 | 1 | 1,500 | 1,500 |
| 8 | 2.32 | 2.37 | 0.77 | 0.81 | 114 | 94 | 0.4 | 0.5 | 1,000 | 2,000 |
| 9 | 2.11 | 0.55 | 30 | 1 | 1,000 | |||||
| 10 | 2.28 | 1.06 | 120 | 0.75 | 1,500 | |||||
| 11 | 2.28 | 0.95 | 31 | 0.5 | 2,000 | |||||
| 12 | 2.32 | 1.16 | 34 | 0.75 | 1,000 | |||||
| Mean | 2.30 | 2.29 | 0.86 | 0.84 | 51.67 | 43.38 | 0.87 | 1.00 | 1,395.83 | 1,581.25 |
| Median | 2.28 | 2.28 | 0.88 | 0.81 | 41.00 | 39.00 | 1.00 | 1.00 | 1,500.00 | 1,500.00 |
| Min. | 2.11 | 2.18 | 0.52 | 0.48 | 15.00 | 7.00 | 0.40 | 0.50 | 750.00 | 750.00 |
| Max. | 2.56 | 2.54 | 1.16 | 1.37 | 120.00 | 94.00 | 1.50 | 1.50 | 2,000.00 | 2,500.00 |
| Normal | 2.1–2.7 | 1.0–1.7 | <55 | |||||||
Laboratory levels and medication preoperatively, respectively, before treatment and 1 year after surgery
aOne year after surgery
Clinical endpoints were height, leg axis, and pain.
Results
We followed 12 patients (9 females, 3 males) diagnosed with VDXLR at age from birth to 11 10/12 years (median 3 9/12) (see Table 2). The median follow-up period was 7 8/12 years (range 1 9/12–30), and the age at latest follow-up was 13 6/12 years (range 2–30 years).
Table 2.
Clinical data
| Patient | Sex | Bilateral corrective operation (number) | Lengthening | Age at first consultation (years) | SDS height | Age at first corrective surgery (years) | Age at last follow-up (years) | SDS final height | Overall follow-up (years) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 5 | Yes | 9 | −3.03 | 9 | 16 5/12 | −1.63 | 7 5/12 |
| 2 | F | 3 | No | 5 9/12 | −0.47 | 6 7/12 | 14 7/12 | 0 | 8 10/12 |
| 3 | M | 1 | Yes | 5 6/12 | −1.21 | 14 6/12 | 17 2/12 | −2.13 | 11 8/12 |
| 4 | M | 1 | Yes | 1 4/12 | 0 | 3 9/12 | 5 2/12 | −0.28 | 3 10/12 |
| 5 | F | 1 | No | 2 2/12 | −3.15 | 3 5/12 | 12 5/12 | −1.19 | 10 3/12 |
| 6 | F | 1 | No | 11 10/12 | −1.11 | 12 | 29 5/12 | −1.97 | 17 7/12 |
| 7 | F | 1 | No | 0 | −0.35 | 19 9/12 | 30 | −1.29 | 30 |
| 8 | F | 1 | No | 3 9/12 | −2.23 | 5 6/12 | 7 7/12 | −2.84 | 3 10/12 |
| 9 | F | 0 | – | 3 10/12 | −1.05 | – | 8 7/12 | −1.56 | 4 9/12 |
| 10 | F | 0 | – | 6/12 | 1.63 | – | 8 7/12 | 1.42 | 8 1/12 |
| 11 | F | 0 | – | 9 11/12 | −1.13 | – | 17 2/12 | −0.22 | 7 3/12 |
| 12 | F | 0 | – | 3/12 | −1.0 | – | 2 | −1.84 | 1 9/12 |
| Median | 3 9/12 | −1.08 | 7 9/12 | 13 6/12 | −1.42 | 7 8/12 | |||
| Range | 0–11 10/12 | −3.15–1.63 | 3 5/12–19 9/12 | 2–30 | −2.84–1.42 | 1 9/12–30 |
Height expressed as standard deviation score (SDS)
Eight patients underwent surgery. Six patients had a single bilateral surgical correction, whereas one patient each had three and five operations. The latter patient’s course is summarized below. The age at first corrective intervention ranged from 3 5/12–19 9/12 years (median 7 9/12); the age for the last intervention for the two patients with repeated corrective surgery was 15 2/12 and 13 3/12. Three patients underwent bone lengthening using an external fixator system (Monotube Triax, Stryker, Geneva, Switzerland) with a lengthening rate of 1 mm per day. The operated patients were followed for a median period of 9 6/12 years (range 3 10/12–30). The median follow-up from the last surgical intervention to the most recent consultation was 2 4/12 years (range 1 3/12–17 5/12). At last follow-up, five patients had a mature skeleton, and seven, including four treated surgically, were still growing. The deformity of axes before surgery respectively before treatment and the axes in the follow-up are summarized in Table 3.
Table 3.
Axis deformity pre- and postoperatively
| Patient | Preop./pretreatment | Last follow-up |
|---|---|---|
| 1 | Multiple deformity | Neutral |
| 2 | Genua valga | Neutral |
| 3 | Genua vara | Genua valga |
| 4 | Genua vara | Neutral |
| 5 | Crura vara | Neutral |
| 6 | Genua vara | Neutral |
| 7 | Crura vara | Neutral |
| 8 | Genua valga | Neutral |
| 9 | Neutral | Neutral |
| 10 | Neutral | Neutral |
| 11 | Genua valga | Neutral |
| 12 | Neutral | Genua vara |
Preoperative deformity or deformity before treatment and axes at latest follow-up. Numbers 1–8: operated. Numbers 9–12: none operated
Patients with surgery
Indication for surgery in eight patients was bone deformity, and in one case also pain.
Six patients had single bilateral corrective surgery. The underlying deformity was genua vara, crura vara, and genua valga in three, two and one patient, respectively. The deformation for the genua vara ranged from 12 to 33°, for crura vara from 14 to 19°, and for genua valga from 14 to 25°. Genua vara were corrected by an infracondylar valgization with a K-wire fixation in one patient and plates in two patients. Crura vara were corrected with corticotomy of the tibia and fibula and simultaneous bone lengthening in two patients. The patient with genua valga was corrected by a bilateral supracondylar varisation using plates.
The lengthening procedure was performed in cases where patient desire was present; interestingly, all were males. Principally, in all small-stature patients a lengthening procedure was discussed. The final decision was established by the patient or patients’ parents.
The frowth of the operated patients is summarized in Graph 1 for boys (all underwent lengthening) and Graph 2 for girls (none underwent lengthening).
Graph 1.
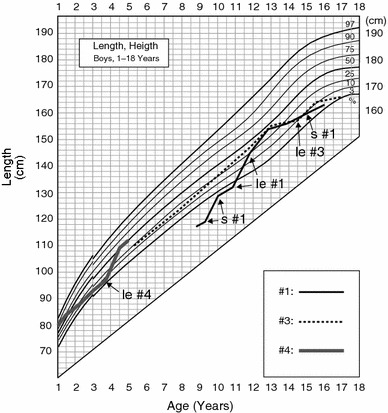
Growth chart of three male patients (nos. 1, 3, and 4). Corrective interventions are shown (arrow): le: lengthening; s: surgery
Graph 2.

Growth chart of five girls (nos. 2, 5–8) with corrective surgery. Corrective interventions are shown; s: surgery
Two patients had repeated corrective operations. One patient (no. 2) with genua valga (14°) initially underwent a supracondylar varisation using plates. Due to recurrence of genua valga at the age of 11 years, a hemiepiphysiodesis of both medial distal femora was performed [13–15]; due to right genu varum at the age of 13 years, she underwent an additional hemiepiphysiodesis of the proximal fibular side of the tibia and an epiphysiodesis of the proximal fibula by the technique described by Canale [13, 14]. At latest follow-up, the girl had a physiological axis.
One patient (no. 1) had five bilateral corrective interventions, two corrective manipulations using the external fixator in situ, and twice an osteosynthesis of a fracture with re-fracture of the right femur. This boy had presented as an asylum seeker at the age of 9 years with very short stature (well below the third centile), pain, and multiple deformities, such as coxa vara, femora vara, and crura antecurvata (Fig. 1a–c). The first intervention included acute extension osteotomies of the tibiae and corticotomies of the fibulae; the tibiae were fixed with compression screws. One year later, a subtrochanteric valgization was performed and fixed with an external fixator. This step was staged with a time delay of 3 months. A femoral lengthening by 33 mm was performed. At the age of 11 years, a corticotomy with bone lengthening of both tibiae and fibulae (35 mm) was performed with correction of crura vara. At the age of 12 years, a bilateral femoral shaft corticotomy was performed with an additional elongation of 50 mm. Six months after consolidation, a right femoral shaft fracture occurred. An elastic nailing procedure was performed with uneventful consolidation. The last corrective surgical intervention because of femoral varus deformity was a bilateral femoral shaft corticotomy on two levels at the age of 15 years and 3 months using an intramedullary nail. At latest follow-up at the age of 16 5/12 years, he is pain free, has physiological axes (Fig. 2), and his height was in the third centile (167 cm) (Graph 1).
Fig. 2.

Lower extremities of patient 1 at his last consultation with correct axes
In our small group of three patients with lengthening, one patient gained height as assessed as a rise in height centiles (no 4), one patient gained height in the beginning, but lost height centiles again during follow-up (no, 1), and one patient even showed a drop in the centiles (no. 3). This patient was, however, non-compliant and became progressively overweight (BMI = 27.5 kg/m2).
There were a few surgical complications. One patient with bone lengthening had a temporary ankle contracture. Another patient with elongation had a pin tract infection that healed on antibiotic therapy without interruption the elongation procedure. Bone healing was excellent. The implants were removed in all patients.
At the last follow-up, six of the eight operated patients had physiological axes. Two patients had mild genua vara; one complained of intermittent pain over the last 2 years. There was no radiological evidence of degenerative arthropathy.
Patients without surgery
Three of the four non-operated patients had presented with physiological axis; only one had mild genua valga. Height was normal, ranging from 10th to 97th centiles (Graph 3); at last follow-up, one patient with initially physiological axis had mild genua vara, whereas the patient with initial genua valga had a physiological axis. No patient complained of pain. Height ranged from below the 3rd to the 90th centile.
Graph 3.

Growth chart of four girls (nos. 9–12) on medical treatment
Discussion
Vitamin D-resistant hypophosphatemic rickets (VDXLR) is a rare metabolic disease that needs close cooperation between different disciplines. The main therapeutic pillars are adequate phosphate and vitamin D substitution to enhance axes and longitudinal growth. Surgery is needed for patients with limb deformity. The primary goal of surgery is to correct the axis to avoid pain and secondary joint degeneration. It has been stated that surgery should not be done before the end of bone maturation because of the potential risks of non-union and recurrence of deformity [5]. The concept at our unit, however, is to do corrective surgery when medical therapy fails to maintain normal axes and longitudinal growth, independently of age or bone maturation.
Eight patients had corrective osteotomies for axial deviation, three of them also a lengthening procedure. In the majority of patients, a single bilateral simultaneous intervention restored the correct axis. There was no case of non-union in the whole series. Two patients had recurrent deformities despite the fact that initial surgery had successfully restored the axis and that medical treatment was adequate with good compliance, suggesting a more severe metabolic disease. One of those patients had a recurrence at knee level twice despite a good surgical correction. With close clinical follow-up, recurrence of bone deformity could be recognized early to allow for appropriate surgical interventions, i.e., hemiepiphysiodesis and epiphysiodesis, resulting finally in a physiological axis. This case concurs with Novais and Stevens' [15] finding that hemiepiphysiodesis is a good procedure in cases close to bone maturity or with small deformity. With the calculating height, respectively, the growth potential, smaller deformity can be corrected with this minimally invasive procedure.
The second patient with recurrent deformity was the boy undergoing five bilateral corrective interventions. However, not all operations were because of recurrence. He had severe deformities at all levels of the legs at diagnosis when he arrived as the son of asylum seekers. The patient is highly satisfied with the final result (Fig. 2), yet at the price of a high number of interventions for corrective operations and implant removals.
Short stature is also a main issue for children with VDXLR, making lengthening procedures an option. The common indication for long bone lengthening is a shortening of the whole or partial limb in one or both legs. The main causes are either congenital or posttraumatic [16, 17]. The technique is to lengthen the osteotomied bone by callus distraction. There are various published techniques and experiences [18–23]. The procedure is often performed with a circular or a monolateral external fixator, but also over an intramedullary nail [24]. Initial reports of callus distraction had a low rate of complications [18–22] in contrast to published experiences a few years later [16, 20, 24–29]. The study of Tjernström [16] showed that most complications were mild or moderate, and rarely severe. Thirty-six of 42 patients in his study were satisfied with the lengthening procedure. In a newer study of Garcia-Cimbrelo [24] using a nail for femoral lengthening, the complication rate was low.
Lengthening of long bones for short-stature patients with VDXLR has been reported by Dudkiewicz [12]. He had used the principal of callotasis with an external fixator and an elongation rate of 1 mm per day (0.25 mm four times a day). The external fixator was left in situ until radiographic union was established in accordance with other reports of lengthening [21]. The study of Dudkiewicz [12] concluded that though a metabolic bone disease is not a common indication for lengthening and could be problematic, lengthening can be considered as an option. The study of Song et al. [11] showed a larger number of bone lengthenings. Some of the complications reported are severe, such as nerve palsy or deep intramedullary infection, which happened in combination with distraction and intramedullary nailing. This combination makes sense to prevent refracture, but the complication of deep intramedullary infection is very severe and has to be evaluated with the risk of refracture. Our complications with lengthening were minor. Joint stiffness resolved after stopping lengthening. Pin tract infection healed after antibiotic therapy.
We agree with Dudkiewicz’s report and the study of Song et al. [11, 12]. The results of our small group demonstrate that the lengthening technique is a satisfactory option for short stature also in compliant patients with metabolic bone disease.
We conclude that medical treatment remains the main pillar of therapy in children with VDXLR. In case of bone deformity, surgery can safely be performed, independent of age or bone maturation. All patients were satisfied with the results of axial corrective surgery and bone lengthening, and in the majority only one corrective intervention was needed. The role of the lengthening procedure to improve short stature needs further studies. Close cooperation between pediatricians and orthopedic surgeons is mandatory for optimal care of these patients.
References
- 1.Albright F, Butler AM, Bloomberg E. Rickets resistant to vitamin D therapy. Am J Dis Child. 1937;54:529–547. [Google Scholar]
- 2.Rohmiller MT, Tylkowski C, Kriss VM, Mier RJ. The effect of osteotomy on bowing and height in children with X-linked hypophosphatemia. J Pediatr Orthop. 1999;19(1):114–118. [PubMed] [Google Scholar]
- 3.Rubinovitch M, Said SE, Glorieux FH, Cruess RL, Rogala E. Principles and results of corrective lower limb osteotomies for patients with vitamin D-resistant hypophosphatemic rickets. Clin Orthop Relat Res. 1988;237:264–270. [PubMed] [Google Scholar]
- 4.Petersen DJ, Boniface AM, Schranck FW, Rupich RC, Whyte MP. X-linked hypophosphatemic rickets: a study (with literature review) of linear growth response to calcitriol and phosphate therapy. J Bone Miner Res. 1992;7(6):583–597. doi: 10.1002/jbmr.5650070602. [DOI] [PubMed] [Google Scholar]
- 5.Eyres KS, Brown J, Douglas DL. Osteotomy and intramedullary nailing for the correction of progressive deformity in vitamin D-resistant hypophosphataemic rickets. J R Coll Surg Edinb. 1993;38(1):50–54. [PubMed] [Google Scholar]
- 6.Ferris B, Walker C, Jackson A, Kirwan E. The orthopaedic management of hypophosphataemic rickets. J Pediatr Orthop. 1991;11(3):367–373. doi: 10.1097/01241398-199105000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Evans GA, Arulanantham K, Gage JR. Primary hypophosphatemic rickets. Effect of oral phosphate and vitamin D on growth and surgical treatment. J Bone Joint Surg Am. 1980;62(7):1130–1138. [PubMed] [Google Scholar]
- 8.Enderle A. Biologico-mechanical behavior of bone in osteomalacia and in phosphate diabetes in adulthood. Orthopade. 1988;17(5):432–439. [PubMed] [Google Scholar]
- 9.Schwagerl W. Orthopedic problems of vitamin D-resistant rickets (phosphate diabetes) Fortschr Med. 1983;101(27–28):1287–1292. [PubMed] [Google Scholar]
- 10.Greene WB, Kahler SG. Surgical aspects of limb deformity in hypophosphatemic rickets. South Med J. 1985;78(10):1185–1211. doi: 10.1097/00007611-198510000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Song HR, Soma Raju VV, Kumar S, Lee SH, Suh SW, Kim JR, et al. Deformity correction by external fixation and/or intramedullary nailing in hypophosphatemic rickets. Acta Orthop. 2006;77:307–314. doi: 10.1080/17453670610046073. [DOI] [PubMed] [Google Scholar]
- 12.Dudkiewicz I, Schindler A, Ganel A. Elongation of long bones for short stature in patients with hypophosphatemic rickets. Isr Med Assoc J. 2003;5(1):66–67. [PubMed] [Google Scholar]
- 13.Canale ST, Christian CA. Techniques for epiphysiodesis about the knee. Clin Orthop Relat Res. 1990;255:81–85. [PubMed] [Google Scholar]
- 14.Canale ST, Russell TA, Holcomb RL. Percutaneous epiphysiodesis: experimental study and preliminary clinical results. J Pediatr Orthop. 1986;6(2):150–156. doi: 10.1097/01241398-198603000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Novais E, Stevens PM. Hypophosphatemic rickets: the role of hemiepiphysiodesis. J Pediatr Orthop. 2006;26:238–244. doi: 10.1097/01.bpo.0000218531.66856.b7. [DOI] [PubMed] [Google Scholar]
- 16.Tjernstrom B, Olerud S, Rehnberg L. Limb lengthening by callus distraction. Complications in 53 cases operated 1980–1991. Acta Orthop Scand. 1994;65(4):447–455. doi: 10.3109/17453679408995491. [DOI] [PubMed] [Google Scholar]
- 17.Ganel A, Horoszowski H, Kamhin M, Farine I. Leg lengthening in achondroplastic children. Clin Orthop Relat Res. 1979;144:194–197. [PubMed] [Google Scholar]
- 18.Monticelli G, Spinelli R. Leg lengthening by closed metaphyseal corticotomy. Ital J Orthop Traumatol. 1983;9(2):139–150. [PubMed] [Google Scholar]
- 19.De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis) J Pediatr Orthop. 1987;7(2):129–134. doi: 10.1097/01241398-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Paley D. Current techniques of limb lengthening. J Pediatr Orthop. 1988;8(1):73–92. doi: 10.1097/01241398-198801000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Aldegheri R, Renzi-Brivio L, Agostini S. The callotasis method of limb lengthening. Clin Orthop Relat Res. 1989;241:137–145. [PubMed] [Google Scholar]
- 22.Ilizarov GA. The principles of the Ilizarov method 1988. Bull Hosp Jt Dis. 1997;56(1):49–53. [PubMed] [Google Scholar]
- 23.Wagner H. Surgical lengthening or shortening of femur and tibia. Technique and indications. Orthopade. 1972;1:59–74. [Google Scholar]
- 24.Garcia-Cimbrelo E, De Curto la Mano A, Garcia-Rey E, Cordero J, Marti-Ciruelos R. The intramedullary elongation nail for femoral lengthening. J Bone Joint Surg Br. 2002;84(7):971–977. doi: 10.1302/0301-620X.84B7.12984. [DOI] [PubMed] [Google Scholar]
- 25.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 26.Eldridge JC, Bell DF. Problems with substantial limb lengthening. Orthop Clin North Am. 1991;22(4):625–631. [PubMed] [Google Scholar]
- 27.Garcia-Cimbrelo E, Olsen B, Ruiz-Yague M, Fernandez-Baillo N, Munuera-Martinez L. Ilizarov technique. Results and difficulties. Clin Orthop Relat Res. 1992;283:116–123. [PubMed] [Google Scholar]
- 28.Aquerreta JD, Forriol F, Canadell J. Complications of bone lengthening. Int Orthop. 1994;18(5):299–303. doi: 10.1007/BF00180230. [DOI] [PubMed] [Google Scholar]
- 29.Herzenberg JE, Scheufele LL, Paley D, Bechtel R, Tepper S. Knee range of motion in isolated femoral lengthening. Clin Orthop Relat Res. 1994;301:49–54. [PubMed] [Google Scholar]


