Abstract
Background
Elastic stable intramedullary nailing (ESIN) is used routinely world-wide for treating femoral and tibial shaft fractures in children before skeletal maturity. Overall, ESIN allows rapid limb mobilisation with few complications. However, many centres have experienced some complications resulting from secondary fracture displacement, especially in heavy adolescents and in spiroid or complex fractures due to changes in the nail’s position, leading to limb shortening, malrotation and malalignment. End caps were designed by the AO expert group to address these complications.
Purpose
The purpose of this study is to evaluate the efficiency, safety and tolerance of this new device in our first series of ten patients and 11 fractures.
Methods
Prospective follow-up of our first ten patients operated on with end caps.
Results
Our results show that there were no serious complications at a mean follow-up of 13.1 months. There was only one 10-mm leg shortening in a patient in whom the end caps could not be properly inserted. There were no infections, no additional pain and no skin irritation. The use of end caps eased the removal of the nails after bone healing, thereby preventing the formation of ossification over the tips of the nails and appeared to protect the skin next to the nail tip.
Conclusion
These results seem to prove the advantage of using end caps when performing ESIN in lower limb shaft fractures in children. A longer follow-up that includes more patients and a randomised prospective study should be carried out in the future to determine more precisely the indications of this new device.
Keywords: Elastic stable intramedullary nailing (ESIN), End cap, Unstable fracture
Introduction
Elastic stable intramedullary nailing (ESIN) is the gold standard in the treatment of diaphyseal fractures in children and adolescents, mainly in cases with unstable fractures [1]. However, residual instability does occur occasionally in spiroid or comminuted fractures, even when there is no particular technical mistake during surgery. A bail-out solution consists of an external fixation or additional traction and casting [2]. The nails may back out due to slight telescoping at the fracture site immediately after surgery and between the second and fifth post-operative days [3]. The need to lock unstable ESIN appears to be necessary in these cases. The AO expert group (Osteosynthesis Association, Davos, Switzerland) addressed this problem by designing cylindric hollow-threaded end caps to be inserted at the tip of the nails and screwed into the bone cortex [4]. To the best of our knowledge, we report here the first preliminary study on the use of such end caps in a pediatric population (ten patients; 11 femoral and tibial shaft fractures). We include data on the complications and the determinants of these complications and the post-operative follow-up, and we discuss these results relative to those obtained with a conventional surgical procedure without the use of end caps.
Material and methods
Between January 2005 and December 2006 ten patients with 11 unstable femoral or tibial shaft fractures were treated by ESIN using end caps in Strasbourg (Service de Chirurgie Orthopédique et Traumatologie Infantile; Pr J.M. Clavert, Hôpitaux Universitaires de Strasbourg). All fractures were closed except for one femoral fracture. An additional patient was treated by ESIN with end caps because of heavy pain in a pandiaphyseal fibrous dysplasia of the right femur. A stress fracture was suspected to be the cause of this pain, and the decision was made to reinforce the fracture with intramedullary nails. All children were operated on by a senior surgeon of the unit.
The ages of the children ranged from 7 to 15 years (mean 10 years); the young girl with fibrous dysplasia was 6 years old. Their weights ranged from 17 to 56 kg. There were three girls and seven boys, with one of the boys having both femoral and tibial fractures. There were two diaphyseal tibial fractures, one distal metaphyseal femoral fracture and seven diaphyseal femoral fractures; all of these fractures were oblique or comminutive.
The operative technique does not differ much from the conventional procedure. The patient is placed on an orthopaedic table, and the fracture is partially reduced by traction under fluoroscopy control. Stainless steel nails, with diameters ranging from 3 to 4 mm depending on the child’s weight and age, are inserted retrograde for the femoral fractures and antegrade for both tibial fractures. The incision is as small as that in a normal ESIN procedure. When in good position, with the fracture properly reduced, the extremities of the nails are cut, and the nails are impacted with the bewelled instrument. Thus, the extraosseous tip of each nail always measures 10 mm. An end cap is then inserted onto the tip of the nail with an appropriate screwdriver and the nail is screwed into the cortical bone under fluoroscopic control, ensuring that the end cap’s thread has a firm grip in the cortical bone (Figs. 1, 2). We took into account every problem encountered with end cap insertion, as well as the fitting of the end cap on the tip of the nails.
Fig. 1.

End cap as designed by the Osteosynthesis Association, Davos, Switzerland (AO group)
Fig. 2.
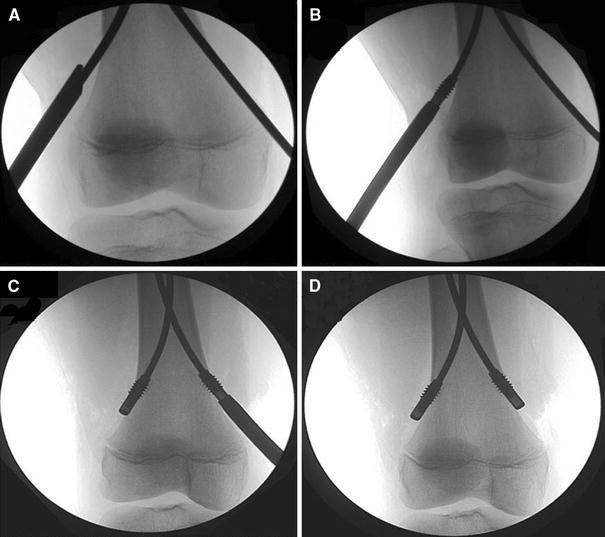
a The impaction of the nail, leaving a 10-mm tip out of the bone cortex, b, c the end cap is screwed into the cortex onto the tip of the nail with the ancillary screwdriver laterally and medially, d the final aspect of the distal locking once the two end caps are firmly in the bone
Each patient was followed up post-operatively for complications and bone healing. Complications were divided into four categories: complications related to the treatment or the instrumentation, those related to the bone and/or the fracture itself, those related to the soft tissues or the wound, such as superficial infection, and those related to general complications .
Bone healing was evaluated in terms of callus quality and bone remodelling as well as in terms of bone growth (varus/valgus, antecurvation/recurvation, limb length shortening and rotation).
Finally, for each patient, we recorded the date of discharge, the type of physiotherapy required, if any, and an estimated time for regaining full unrestricted activity.
Results
In all 11 fractures, closed reduction was achieved. When the end cap was next to the cortex, it was screwed into the cortical bone. In two cases, the medial nail in one case and both the lateral and medial nails in the other case, difficulties were encountered in inserting the end caps. Both cases involved femoral diaphyseal fractures. In one case it was impossible to screw the end cap into the bone cortex; in the second case, the end caps were held rather loosely in the bone. There were no other reasons than inadequate operative technique for this, as the nails were in both cases very correctly inserted and the fractures were anatomically reduced.
The fitting of the end caps was rated good to excellent in all cases except that with the two lateral and medial loose caps. In six cases, the end of the nail was not 100% in contact with the end cap, but in no way did this placement seem to impair the overall stability of the device, as the end cap was correctly inserted into the nail with its thread firmly gripped into the bone cortex.
With respect to the case with fibrous dysplasia of the whole femur, all procedures went very well, but the fitting of the end caps was found to be just fair.
Immediate post-operative examination found no varus/valgus deformities, no antecurvation/recurvation, one shortening of the limb of between 5 and 10 mm, one 10-mm shortening of the limb in the case which had the two loose end caps and one internal rotation greater than 10°.
In all but two cases no additional immobilisation was needed. In these two exceptions, mobilisation was necessary in one case for pain reasons and involved knee splinting for 1 week; in the second case, there was an important knee instability with a patellar fracture, requiring 6 weeks of splinting. There was no link with the ESIN or the end caps in either case.
Only in the case with fibrous dysplasia did we allow full weight bearing after the procedure. In all other cases but one, free movement was allowed, but without weight bearing for 3 weeks post-operative. Partial weight bearing (20% of total weight for 3 weeks) was allowed for the patient with distal metaphyseal femoral fracture, who was a 15-year-old, fully observant adolescent. No physiotherapy was required, and all children regained normal joint range of motion on their own.
All of the fractures healed, and there were no particularly remarkable complications. All nails were removed 4–7 months after the initial surgery, when bone healing was indicated on the X-rays (except for two cases, one with the fibrous dysplasia, and another one who moved away and was lost to follow-up). In eight cases, the date of removal had been planned beforehand and was confirmed by X-ray to be appropriate since the had bones healed correctly. Clinical examination was exactly the same as that immediately after surgery. There was no need to enlarge the initial scars, and the incisions at the distal end of the femur and proximal end of the tibia measured about 20 mm. There was no skin irritation to be noted, and the end caps apparently protected the skin quite well. Extraction of the caps was found to be extremely easy using the same screwdriver ancillary as for implantation, with extraction pushing aside all soft tissues in front of the tip of the nails so that the nail extraction was quite simple in every case. The end caps in the case with the two loose end caps were found to be free from the bone, but this disengagement had not caused any pain or conflict with the skin whatsoever. At the time of removal, all fractures had complete callus forming, with partial remodelling of the callus. In one case, full remodelling of the bone had already occurred, and no fracture or callus was visible 6 months into the follow-up.
The last follow-up visit occurred 10–24 months after the initial surgery (one additional patient being lost to follow-up after removal of the nails), and in six of nine patients we found complete remodelling of the callus. There were still three fractures only partially remodelled, one of which was the case with the two loose end caps. Clinical examination was exactly the same as after surgery and at the time of removal of the nails. There was only one more mild shortening of the limb between 5 and 10 mm.
Overall, by 1 month after the removal of the nails (5–8 months after surgery), the children were able to resume full unrestricted activity.
Discussion
Femoral and tibial spiroid, oblique and comminutive shaft fractures are almost always very displaced and unstable [2, 5]. It is now commonly accepted that ESIN is the gold standard treatment for these fractures [1, 8]. It is considered to be a physiological method of treatment because of early weight-bearing, rapid healing and minimal disturbance of bone growth [6].
However, two major complications are still frequently encountered.
The most frequent complication is pain by skin irritation due to the extraosseous portion of the nail: Narayanan et al. reported 41 irritations in 79 femoral shaft fractures treated by ESIN [7], Ligier et al. reported 13 ulcerations in 123 femoral shaft fractures [6], and Flynn et al. reported four irritations in 58 femoral fractures [8]. In our small series, we did not find any skin ulceration and observed only one case of pain after surgery, but the pain was located next to the fracture and not next to the scar. It appears that the felt tip of the end caps tend to protect the skin from any irritation, whereas the distal ends of the nails, when sharply cut, can cause discomfort at the knee. This problem is particularly important as it is the one most frequently encountered. This irritation led to one deep wound infection in Ligier’s series and to two deep wound infections in Flynn’s series. In addition, in most cases where there was no infection, revision surgery was nonetheless needed to trim the extraosseous portion of the nail. In contrast, we did not encounter any deep wound infection, nor did we need any revision surgery whatsoever after the initial operation.
Clinical and radiographic malunion is the second most frequent complication encountered and is the result of slight telescoping at the fracture site. Narayanan et al. reported eight malunions in his series of 79 fractures (10°–14° varus, 15° recurvatum to 25° antecurvatum, including three patients who healed with 1.5–2.0 cm of shortening) and two refractures [7]. Flynn et al. reported six significant leg-length discrepancies (10–20 mm) from among 58 patients, but this study had a rather short follow-up [8]. They did not report any frontal or sagittal malunion, and they had no loss of rotational alignment, pointing out that Ligier et al. had a similar success [6]. Using end caps, we would seem to have achieved results as good as those reported in the literature, if not better since there were no significant malunion. There was only one 10-mm leg length discrepancy (but none of the two end caps in this case were really efficient since they were loose), and no sagittal, frontal or rotational malunion. However, as Flynn et al. pointed out in the context of their study, we will also need a longer follow-up with more patients to determine the incidence of permanent, clinically significant orthopaedic impairments.
In one of our patients, ESIN with end caps was a secondary surgery 2 days after the initial surgery. A very important telescoping in the fracture had occurred, and the patient needed to be operated on again. By adding end caps, the two nails were unable to back out as they had done on the first post-operative day, and it allowed the fracture to heal without any malunion (Fig. 3). By preventing nail back-out, end caps should be especially used in fractures with bone tissue loss (Fig. 4).
Fig. 3.

Transverse femoral shaft fracture in a 14-year-old boy. Elastic stable intramedullary nailing (ESIN) was performed at first without end caps. On the second post-operative day, the nails backed out and the telescoping into the fracture led to a 20° varus as well as a third fragment. This boy was reoperated on, and end caps were used to achieve complete consolidation without any malalignment or malrotation
Fig. 4.

Complex diaphyseal femoral fracture with a third fragment in a 13-year-old boy. Reduction of the fracture proved to be very unstable. Addition of end caps allowed partial callus to form, and radiographs show the inclusion of the third fragment in the callus 4 months later. This boy also required additional knee splinting for 6 weeks because of a patellar fracture with knee instability
In addition, according to Lascombes et al. [9], femoral shaft fractures induce a mean leg length discrepancy of +5 mm to +10 mm in spiral and long-oblique fractures in children younger than 10 years old on a long-term follow-up. This must be taken into account to make sure that “too well treated” fractures in young children will not end as a final leg length discrepancy by overgrowth. This could be an argument for preferably using end caps in adolescents in whom this overgrowth phenomenon is less likely to occur, thus stressing the importance of avoiding telescoping into the fracture site. In younger children, it may be less important since “natural correction” of this shortening may spontaneously happen as a result of this overgrowth phenomenon.
In the original description of the ESIN technique, no additional immobilisation was mentioned, since all of the most painful knees benefitted from secondary surgery to trim the extraosseous portion of the nails [3, 6]. Flynn et al. recommends that a knee immobiliser be worn 4–6 weeks after surgery—until callus is seen to limit pain [8]. The use of end caps would again seem to remove the need for any additional immobilisation since pain is seldom encountered. We only recommended knee immobilisation (6 weeks) in the case of the child with an associated knee instability with a patellar fracture. End caps would therefore appear meet the technical requirements of the original technique, without having to face secondary interventions to ease the pain .
Full callus bridging was observed in all our patients at 3 weeks after the operation, allowing full weight bearing. It was feared that because of increased stability due to nail-locking by the end caps, there would be less dynamisation of the fracture and delayed bone healing [4]. We did observe, however, that callus formation was not as generous as in classical ESIN procedures. In one case, we had a large gap without any callus remodelling at the time of nail removal. This mildly delayed consolidation did not cause any refracture after removal of the nails, and full unrestricted activities were possible 1 month thereafter. The fracture was likely suddenly dynamised at this time, and the X-rays showed partial callus remodelling shortly after removal. We currently do not have enough experience to recommend whether it will be necessary in the case of non-union to remove the end caps some time between implantation and planned removal to dynamise the fracture healing. Future studies will possibly be able to provide some evidence of a balance between stability of the nails and consolidation of the fracture, but we cannot yet be sure of whether this balance occurs and, if so, when. Based on our results, therefore, we support the latest technical recommendations proposed by Métaizeau [3]: mobilisation of non-weight-bearing with elbow crutches on the fifth post-operative day and full weight-bearing in oblique fractures on the 20th day.
Finally we would like to underline our choice of using stainless steel nails instead of titanium nails. Experimental studies [10] have proven that stainless steel nails are more rigid than titanium nails and that the former show a similar resistance to recall forces when a 3.5-mm stainless steel nail is compared to a 4-mm titanium nail.
Weight-bearing is a very important challenge as far as adolescents are concerned. However, it seems that in large and heavy adolescents, with an almost fused proximal femoral growth plate, the use of an intramedullary locking nail should be considered. Ex vivo experiments have shown that weight-bearing with 3.5-mm stainless steel nails with end caps cannot exceed 2000 N [10].
Conclusion
These preliminary results on a small population of patients provide support for the proposal that end caps are an interesting step forward under circumstances in which ESIN reaches its limits, particularly in adolescents in whom spontaneous correction of malunion or limb shortening due to fracture telescoping is less likely to occur. End caps address the recurrent problem of skin ulceration during post-operative management and tend to facilitate nail removal by protecting the tip of the nail from callus formation, thus shortening overall operating time and avoiding larger scarring during removal of the nails. End caps may also address the problem of nail stability in pathological fractures in which bone quality is very poor. However, all of these very encouraging results must be verified over the long term in studies with a longer follow-up and in multicentric studies including a larger number of patients. Such prospective studies will enable randomising ESIN with and without end caps in unstable femoral and tibial shaft fractures to determine more precisely the indications and unlocking rules.
References
- 1.Lascombes P, Bertrand H, Hadjukowicz J (2000) Fracture of the diaphysis of the tibia in children using elastic stable intramedullary nailing (British Society for Children’s Orthopaedic Surgery: London- January 28, 2000). J Bone Joint Surg Br 82-B[Suppl 3]:239
- 2.Lascombes P, Métaizeau JD (2006) Fracture du fémur. In: Embrochage centromédullaire élastique stable. Elsevier, Paris, pp 207–240
- 3.Métaizeau JP. Stable elastic intramedullary nailing for fractures of the femur in children (operative technique) J Bone Joint Surg Br. 2004;86-B(7):954–957. doi: 10.1302/0301-620X.86B7.15620. [DOI] [PubMed] [Google Scholar]
- 4.Clavert JM, Giacomelli MC, Gicquel P (2006) Verrouillage de l’embrochage centromédullaire élastique stable. In: Embrochage centromédullaire élastique stable. Elsevier, Paris, pp 47–50
- 5.Lascombes P (2006) Fracture de jambe. In: Embrochage centromédullaire élastique stable. Elsevier, Paris, pp 241–261
- 6.Ligier JN, Métaizeau JP, Prévot J, Lascombes P. Elastic stable intramedullary nailing of femoral shaft fractures in children. J Bone Joint Surg Br. 1988;70-B(1):74–77. doi: 10.1302/0301-620X.70B1.3339064. [DOI] [PubMed] [Google Scholar]
- 7.Narayanan UG, Hyman JE, Wainwright AM, Rang M, Alman BA (2004) Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop 24(4):363–369 [DOI] [PubMed]
- 8.Flynn JM, Hresko T, Reynolds RAK, Blasier RD, Davidson R, Kasser J (2001) Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop 21(1):4–8 [DOI] [PubMed]
- 9.Lascombes P, Fockens W, Guichet JM (1997) Femoral shaft fractures in children: the effect on leg length of elastic intramedullary nailing. In: Orthopaedics Proc Eur Federation Natl Assoc Orthop Traumatol. Free Papers: fractures in children. J Bone Joint Surg Br 79-B(2S):187
- 10.Clavert JM, Giacomelli MC, Gicquel P (2006) Inox ou titane? In: Embrochage centromédullaire élastique stable. Elsevier, Paris, pp 25–29


