Abstract
Purpose
To assess the clinical and radiological results of one-stage hip reconstruction for late neglected developmental dysplasia of the hip (DDH) in children above 8 years of age.
Methods
Nineteen hips in 16 patients, 14 females and two males (three being bilateral), were treated by open reduction adequate shortening (up to 5 cm) with derotation, and limited varization if needed, tight capsulorrhaphy, and appropriate pelvic reconstruction (Salter or triple acetabular osteotomy). The average age at operation 10.6 years (range 8–18 years). The period of follow up ranged from 3 to 9 years. A modified approach for the hip joint and upper femur was utilized, allowing better exposure. Pre- and post-operative plain radiography was performed for all cases and at follow up. Computed tomography (CT) or multislice CT with 3D reconstruction were carried out pre-operatively for recent cases and post-operatively for all, and were found to be helpful in providing a panorama of the dysplastic hip and in planning the required surgery and assessing the results.
Results
According to the McKay modified criteria, 15 hips (79%) were clinically excellent to good, while four hips (21%) were fair to poor. Radiographically, according to the Severin modified criteria, 16 hips (84%) were excellent to good and three hips (16%) were fair to poor. Limb length discrepancy ranged from 0.5 to 2.1 cm, as measured by CT scanograms. Complications were avascular necrosis (AVN) in an early case due to limited femoral shortening with resultant excessive stress over the femoral head and subluxation in another case.
Conclusion
A one-stage hip reconstruction for late neglected cases of DDH have achieved excellent results if adequate shortening with derotation is performed, together with appropriate acetabular reconstruction and tight capsulorrhaphy. Varization should not replace part or all of the required shortening, and should be added if required.
Keywords: Neglected DDH above 8 years of age, Hip reconstruction, Developmental dysplasia of the hip
Introduction
The principles of the treatment of developmental dysplasia of the hip (DDH) for older children are different from those for newborns [1–3]. The difficulty of management is in how to overcome the contracted soft tissues and stimulate the acetabular remodeling ability [4]. The problem lies in reducing the femoral head into the acetabulum, maintaining the concentric reduction, and obtaining a satisfactory functional hip [5].
Many authors have recommended a one-stage procedure for hip reconstruction consisting of open reduction, femoral shortening with or without varus derotation osteotomy, adequate capsulorrhaphy, and pelvic osteotomy [6–10].
Femoral shortening helps prevent excessive pressure on the femoral head when it is relocated in the acetabulum, which may predispose to avascular necrosis (AVN) [5, 9, 10]. The relocated hip is often very unstable, owing to a dysplastic shallow acetabulum, and a pelvic operation is required to achieve stable concentric reduction of the hip [8, 10].
The aim of the current study is to evaluate the results of hip reconstruction performed in one stage for late, neglected DDH, in children presenting at the age of 8 years and above. The important factors contributing to a successful hip reconstruction are also highlighted.
Material and methods
Nineteen hips in 14 females and two males (three being bilateral) were collected from the Health Insurance Hospital for School Children and Newborns in Alexandria, Egypt. All were late neglected DDH and presenting for the first time at an age ranging from 8 to 18 years (average 10.6 years). Patients with neuromuscular disorders were excluded. The main reason for presentation was an evident painless limp with appreciable shortening. The period of follow up ranged from 3 to 9 years (average 5.3 years).
Imaging studies
Plain anteroposterior view with internal rotation, together with lateral views, were done for all cases. Computed tomography (CT) or multislice CT with 3D reconstruction views were carried out pre-operatively for the last seven operated cases and at follow up for all. These were found to be helpful in declaring the magnitude of the problem and the degree of coxa valga, if present, and femoral neck anteversion.
Radiographic evaluation included examination of the pre-operative and follow up radiographs for quantitative measurements of the acetabular index and center-edge (CE) angle of Wiberg. Careful examination was done for the shape of the femoral head, neck, and the acetabulum.
Important surgical considerations
The hip is exposed via a modified iliofemoral approach for the hip and upper femur utilizing a combined Smith Peterson and bikini approach of Somerville. The incision as shown in Fig. 1a starts at the mid iliac crest, extends anteriorly past the anterior superior iliac spine to the mid inguinal point, and turns posteriorly to the flare of the greater trochanter and then distally parallel to the femoral shaft. The interval between the sartorius and tensor fascia lata is developed. Exposing and severing the underlying tendon of the rectus femoris shows the capsule covering the dislocated femoral head. Next, peel off the glutei from the outer table of the iliac bone and the iliacus from the inner table and expose well the iliac bone for any pelvic procedure. Through the distal limb of the approach, cut through the vastus lateralis to show the femoral shaft. Now, the iliac bone, the hip, and the upper third femur are exposed, allowing for accurate estimation of the needed femoral shortening, varization, and derotation (Fig. 1b).
Fig. 1a, b.
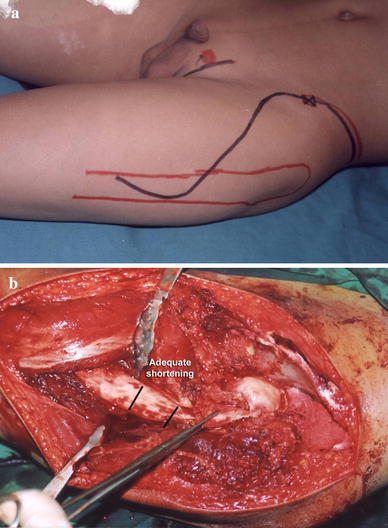
The modified iliofemoral approach. a Skin incision extending from the mid iliac crest to a mid inguinal point, then downwards and posteriorly to the trochanteric flare, to continue parallel to the femoral shaft. b Following full exposure, the iliac bone, the hip joint all round, and the upper third of the femoral shaft are well exposed
Extensive adductor tenotomy is performed through a straight incision from the adductor tubercle down to the ischial tuberosity using a diatherm and remaining close to the distal pubic ramus, releasing all of the adductors down to bone. This will facilitate femoral head reduction later (Fig. 2). The iliopsoas tendon is hooked and severed at the pelvic brim using a diatherm.
Fig. 2.
a Adductor incision: a straight incision extending from the adductor tubercle down to the ischial tuberosity. b Adductor tenotomy along the inferior pubic ramus down to bone. Osteotomy of the pubic rami could be done in triple pelvic osteotomy
Capsulotomy
The capsule should be clearly exposed from the overlying glutei superolaterally and the soft tissues inferomedially using a diatherm to minimize bleeding. The capsule is then incised well to show the underlying femoral head and the deeply seated acetabular fossa. The ligamentum teres, if present, should be severed and followed down to the acetabulum. The transverse ligament is felt by the tip of the index finger and released to ensure a stable seating of the femoral head after clearing the acetabular fossa from soft tissues. One may apply gentle traction to reduce the femoral head; this will partially stretch the surrounding soft tissues and give an idea of its slackness and the expected femoral shortening needed.
Adequate femoral shortening
This is one of the cornerstones for a successful reduction. Varization should not be attempted to limit the required femoral shortening. Up to 5 cm of shortening might be needed in some older children to effectively slacken the contractured soft tissues. When calculating the required femoral shortening, one should consider the expected pressure exerted over the femoral head following the pelvic procedure. It happened that, following acetabular reconstruction, further shortening was required to relieve pressure exerted over the femoral head. The fixing plate was removed and reapplied after re-shortening. One should be confident that the femoral head is well seated, stable, and under no pressure at the end of the procedure.
In 11 cases (57%), the femoral head appeared to be abnormally smaller than the other side and the acetabulum was comparatively better developed. These cases, although highly dislocated, were easily reduced into the reconstructed acetabulum.
Derotation and varization
The described exposure was helpful in estimating the required femoral derotation and varization. Following shortening, the degree of derotation was calculated after fixing the plate to the proximal fragment, usually over the lateral trochanteric flare. The femoral head was reduced into the acetabulum, temporally maintained by 2 K-wires introduced through the trochanter. The distal fragment is then rotated externally to bring the patella to face the ceil. Applying the straight plate over the flare of the trochanter allowed a few degrees of varization, which was enough in most cases, since the pre-operative neck shaft angle was within the normal range.
Pelvic procedure
The pelvic procedure utilized in this study was a Salter osteotomy in 12 hips. The acetabular fragment was intentionally displaced more lateral than anterior. This will offer stability without uncovering the head posteriorly. Triple pelvic osteotomy was performed in seven hips. Adequate displacement of the acetabular fragment was difficult without additional pubic and ischial osteotomies performed through the adductor incision. At least three stout K-wires (>2 mm) were needed to keep the reconstruction stable.
A fibercast hip spica in mild internal rotation and abduction limited to 10–20° is applied. More abduction will tend to push the laterally displaced acetabular fragment medially, disrupting the reconstruction and uncovering the femoral head. Immobilization should continue for 6–8 weeks. The K-wires are removed with the cast, while the femoral plate is removed 6–12 months later.
Results
The patients were evaluated clinically and radiologically at 3-month intervals. The reported results reflect data collected from the last follow up.
According to the modified McKay criteria [11] (Table 1), out of the 19 hips comprising this study, ten (53%) were excellent, achieving a stable painless hip, no limp, negative Trendelenburg sign, and a full range of movement (Figs. 3 and 4). Five (26%) were good because of a slight limp and some limitation of range of movement (Figs. 5 and 6), although, radiographically, these cases may prove to be excellent.
Table 1.
Modified McKay criteria
| Excellent | Stable, painless hip, no limp, negative Trendelenburg sign, and a full range of movement |
| Good | Stable, painless hip, slight limp, negative Trendelenburg sign, and a slight decrease in range of movement |
| Fair | Stable, painless hip, limp, positive Trendelenburg sign, and limitation of movement |
| Poor | Unstable or painful hip, or both; positive Trendelenburg sign |
Fig. 3a–k.
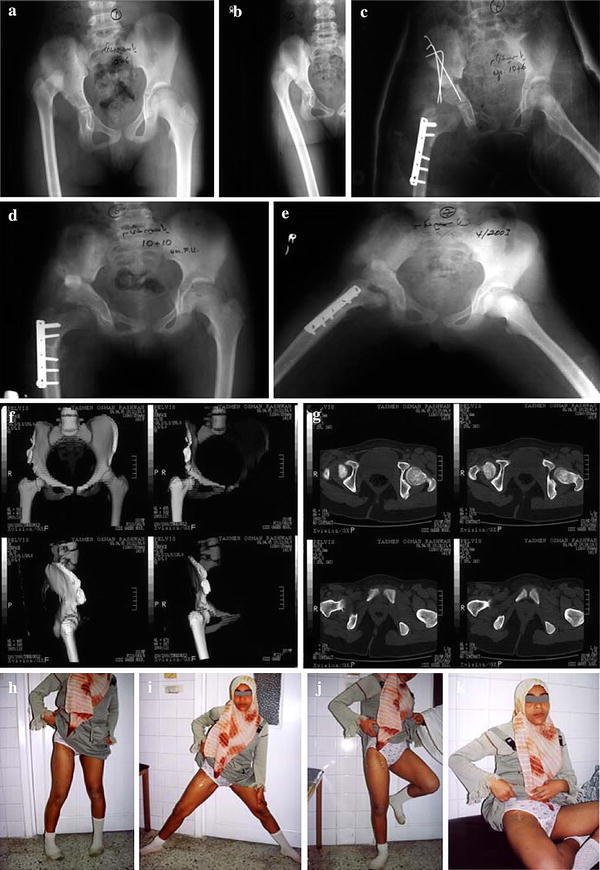
Right developmental dysplasia of the hip (DDH) in an 11-year-old girl with excellent outcome. a, b Pre-operative radiograph in internal rotation revealing a normal neck shaft angle with a relatively small femoral head. c Post-operative reduction, well-contained head, triple pelvic osteotomy with the excised femoral segment used as a graft to maintain acetabular displacement. d, e Radiograph at 2 years follow up in full abduction with extended hips. f, g Multislice computed tomography (CT) sections and 3D reconstruction revealing normal anteversion angle and a normal hip articulation. h–k Photographs of the patient at 17 years of age with a mobile hip performing all movements
Fig. 4a–m.

Left DDH in a 12-year-old girl with excellent outcome. a, b Pre-operative radiograph and 3D reconstruction CT views showing a highly dislocated relatively small femoral head. c Post-operative radiograph, with well-contained femoral head following 5 cm femoral shortening with derotation, minimal varization Salter pelvic osteotomy. d Two years follow up radiographs. e, f Three years follow up radiographs with full abduction in extension. g–i Three years follow up CT with reconstruction views showing well-contained femoral head with normal anteversion angle. j–m Photographs showing full range of movements of the left hip, yet with an unsightly scar
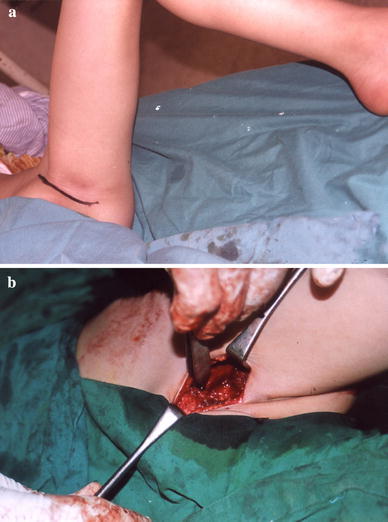
Fig. 5a–d.
Bilateral DDH in a 10-year-old girl with good outcome. a Pre-operative radiograph showing highly dislocated femoral heads. b Late post-operative radiograph for both hips. The left was reconstructed first; a triple pelvic osteotomy was performed. The right side followed; a Salter osteotomy was found to be enough to cover the head. c, d CT with 3D reconstruction showing an excellent reconstruction, with accepted anteversion angle, yet the left hip had limitation of abduction
Fig. 6a–c.
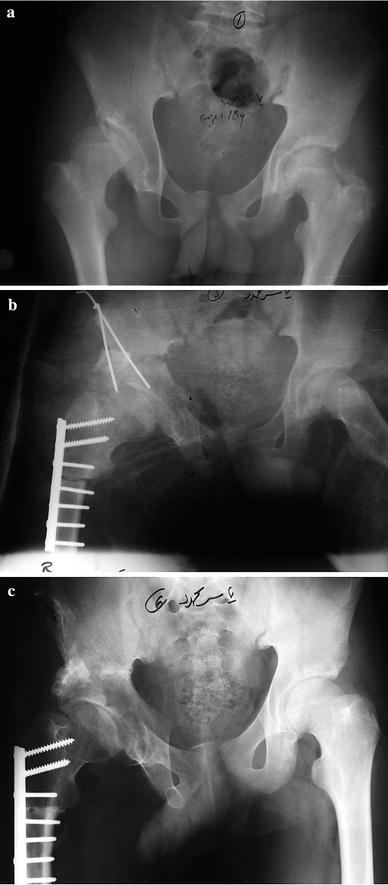
Right DDH in a 18-year-old male with good outcome. a Pre-operative radiograph showing a dysplastic acetabulum. b Post-operative radiograph. The head is well-contained and 3 cm shortening was needed to bring the head down and to compensate for the pelvic procedure. c Late follow up radiograph
The unsatisfactory cases were three fair patients (16%) with a stable painless hip, yet positive Trendelenburg sign and limitation of movement, which was usually abduction (10–25°) and internal rotation in flexion (0–10°) due to excessive external derotation. The only poor case (5%) was unstable, showing evidence of radiological coxa plana due to AVN of the femoral head (Fig. 7).
Fig. 7a–d.
Right DDH in a 9-year-old girl with a poor result. a, b Pre-operative radiographs in neutral and internal rotation. c Late post-operative view showing excessive varization at the expense of shortening with evident avascular necrosis (AVN). d Coxa vara 7 years later (aged 16 years)
According to the modified Severin criteria [12] (Table 2), 16 hips (84%) were graded as excellent to good, while two (11%) were considered as fair due to a dysplastic acetabulum with a CE angle less than 20°. In one, coxa valga developed mostly due to the arrest of trochanteric growth secondary to plate application transfixing its epiphyseal plate (Fig. 8). The other was coxa plana graded clinically as poor. The poor case (5%) was a subluxated hip which was clinically fair. Two weeks post-operatively, the child walked in the clinic in his hip spica while holding his father’s hand. Plain radiographs revealed a subluxated head with disruption of the acetabular reconstruction.
Table 2.
Modified Severin classification
| Excellent | |
| IA | CE angle >19°, age 6 to 13 years; CE angle >25°, age >14 years |
| Good | |
| IB | CE angle 15° to 19°, age 6 to 13 years; CE angle 20° to 25°, age >14 years |
| II | Moderate deformity of the femoral head, femoral neck or acetabulum, but otherwise the same as grade I |
| Fair | |
| III | Dysplastic hip, no subluxation; CE angle <20°, age >14 years |
| Poor | |
| IV | Subluxation |
| V | Femoral head in false acetabulum |
| VI | Redislocation |
CE: center-edge
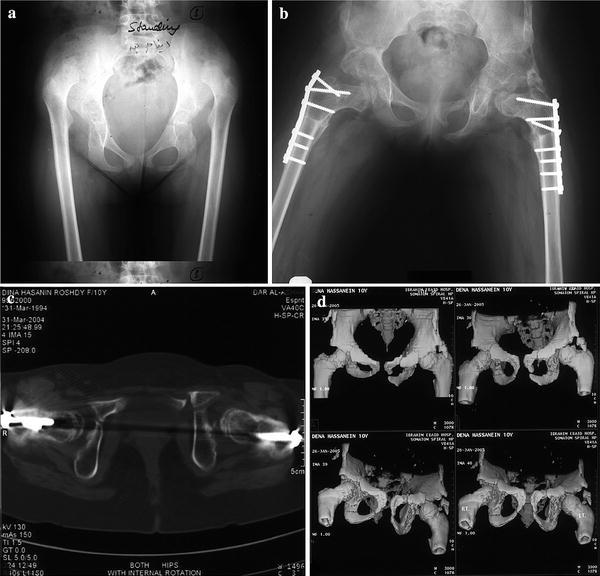
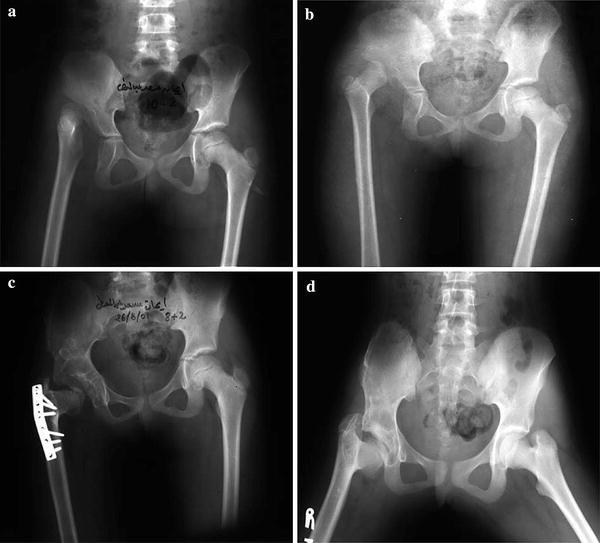
Fig. 8a–d.

Left DDH in an 8-year-old girl with a fair outcome. a Pre-operative radiograph. b Post-operative radiograph showing a well-contained femoral head with acceptable neck shaft angle. c Two years follow up radiograph showing coxa valga, yet still a well-contained head and intact Shenton line. d Eight years follow up (aged 16 years) showing severe coxa valga with subluxation
Limb length discrepancy (LLD) should not be considered as a complication. It was not an issue bothering the patient or the parents, and was found to decrease gradually at follow up. At late follow up visits, the LLD ranged from 0.5 to 2.1 cm in six patients, as accurately measured by CT scanograms, especially in older presenting patients. Shoe lift was all that was needed.
Table 3 summarizes the clinical data of the studied patients.
Table 3.
Clinical data of the studied cases
| Case no. | Age at operation | Operation | Follow up data | |||||
|---|---|---|---|---|---|---|---|---|
| Shortening (cm) | Pelvic procedure | Duration | Gait | LLD | Clinical evaluation | Radiographic evaluation | ||
| 1 | 8 | 3 | Salter | 9 | Normal | – | Excellent | IA |
| 2 | 9 | 2.5 | Salter | 8 + 7 | Trendelenburg | −2 | Poor | III |
| 3 | 11 | 4 | TPO | 6 | Normal | – | Excellent | IA |
| 4 | 8 | 3 | Salter | 8 | Trendelenburg | +2 | Fair | III |
| 5 | 10 | 3 | Salter | 6 + 6 | Normal | – | Excellent | IA |
| 6 | 10 | 4 | TPO | 6 + 3 | Normal | – | Good | IB |
| (7) | 10 + 8 | 5 | Salter | 5 + 7 | Normal | – | Good | IA |
| 8 | 11 | 2 | Salter | 6 | Normal | – | Good | IB |
| 9 | 12 + 3 | 4.5 | TPO | 6 | Normal | −1.5 | Excellent | II |
| 10 | 18 | 3 | TPO | 5 + 9 | Normal | −2.1 | Good | IA |
| 11 | 10 + 5 | 3 | TPO | 5 | Normal | – | Excellent | IA |
| (12) | 12 | 3.5 | TPO | 4 + 6 | Normal | – | Good | II |
| 13 | 13 | 3 | Salter | 4 + 6 | Normal | −1.5 | Excellent | IB |
| 14 | 8 + 3 | 2.5 | Salter | 4 | Normal | – | Excellent | IA |
| (15) | 8 | 2 | Salter | 3 + 2 | Trendelenburg | – | Fair | IV |
| 16 | 12 | 3.5 | Salter | 3 | Normal | −0.5 | Excellent | IA |
| 17 | 11 + 2 | 4 | TPO | 3 | Trendelenburg | – | Fair | IB |
| 18 | 8 + 2 | 2 | Salter | 3 | Normal | – | Excellent | IA |
| 19 | 9 | 2 | Salter | 3 | Normal | – | Excellent | II |
For bilateral cases, the second side is indicated by in parentheses
Clinical evaluation: modified McKay criteria
Radiographic evaluation: modified Severin classification
AVN: avascular necrosis; TPO: triple pelvic osteotomy
Complications
AVN occurred in one case presenting at the age of 9 years. Care to limit shortening to a minimum and relying on excessive varization to adequately stabilize the femoral head resulted in tight reduction with excessive pressure exerted over the femoral head.
Subluxation of the hip occurred in one occasion due to walking in plaster.
A green stick supracondylar femoral fracture occurred in one occasion with bilateral DDH. Reconstruction was performed in two consecutive settings without allowing an interval for physiotherapy. Follow up plain radiography showed a marked decrease of bone density and the patient remained in hip spica for around 5 months. The right femur broke at the time the spica was removed. It united readily.
Cases operated early in this study had less favorable results than late ones. The learning curve improved regarding dealing with technical problems and in considering the importance of certain cornerstones contributing to a successful outcome.
Discussion
On reviewing the literature, reports on the management of late neglected DDH presenting after the age of 8 years were scarce. This was simply because such neglected cases are usually seen in developing countries. The Health Insurance Hospital for School Children and Newborns is a tertiary care hospital dealing with such cases and accepting referrals from the Central and West delta provinces.
Some authors warned against the operative treatment of such cases [13–16]. Others reported on large series where open reduction with femoral shortening gave satisfactory results [1, 5, 6, 8, 17, 18]. The age at operation ranged from 3 to 14 [10], 4–10 [18], 8–17 [19], and 10–17 [17] years. In the current study, the age ranged from 8 to 18 years, with an average of 10.6 years. According to an interesting study delivered by Lindstrom et al. [4], significant and continuing improvement of the acetabular index was observed between 2 and 8 years after reduction when the femoral head remained concentrically reduced. Harris [20] stated that a congruous reduction should be obtained before the age of 4 years because a significant correction by acetabular growth occurs up to approximately 8 years of age. The author, therefore, believes that neglection should be considered late for cases with DDH presenting above 8 years of age, since acetabular remodeling is not expected.
Some authors recommended Salter osteotomy as an essential step in the reconstructive procedure [5–8, 21], while others [18] used Tonnis acetabuloplasty and believed that Salter or Pemberton osteotomies are contraindicated. Ok et al. [19] used Chiari osteotomy in only three out of 11 affected hips 8–17 years old. Their procedure consisted of open reduction and limited femoral shortening, with derotation and varization as a basic step. They believed that the first important surgical principle is an “excessive femoral neck varus,” femoral shortening up to 1.5 cm only came next. Shih and Shih [5] believed that the femoral neck shaft angle measuring 100–110° is the best radiographic outcome. Normal acetabular remodeling cannot be expected to occur in the majority of hips after varus derotation osteotomy alone in older children [5, 20]. Although coxa vara is considered when the neck shaft angle is below 110°, in the current study, values down to 100° are accepted as within normal values, as a few degrees of varization aiming at stability was attempted occasionally. Papavasilious and Papavasilious [17] did not mention any pelvic procedures adopted in their 11 patients (16 hips) with ages ranging from 10 to 17 years. They performed open reduction with femoral shortening and derotational osteotomy only. In most of our cases (57%), the dislocated femoral head was comparatively smaller and acetabulum was less dysplastic. This was evident on plain radiography; the femoral head was easily contained in the reconstructed acetabulum. In the available literature, there is no mention for such observation.
Although pre-operative skeletal traction to slacken the contractured soft tissues was recommended in most old reports and revived recently by Ok et al. [19], the current study agrees with most recent studies recommending adequate femoral shortening to bring down the femoral head to be easily contained in the acetabulum [1, 6, 17–19, 22]. Vallamshetla et al. statement that “too much shortening is often better than too little” is the clue to a successful reduction and an excellent functional outcome [18]. In some reports, shortening did not exceed 2 cm [21] or 1.5 cm [2]. In this study, the older the patient, the greater the need for shortening, which might happen to reach 5 cm. One should bear in mind the following; first, the resulting limb length discrepancy will be less than the pre-operative value simply because bringing down the head into the acetabulum will compensate for such shortening to a great extent; second, varization should not be attempted to replace part or all of the required shortening, since this may end with a Trendelenburg gait; third, any trial to limit the required shortening at the expense of increased pressure exerted over the femoral head will end with either AVN, limitation of joint mobility, or subluxation or dislocation. Limb length discrepancy diminished over time, especially in children below 12 years of age, and it did not become a problem. Compensation by a shoe lift was used in all cases. A stable painless mobile hip should be the target. The only case of AVN ending with coxa vara and the limitation of hip movement was due to a faulty limited shortening with increased tension over the femoral head early in this study. This agrees with the observation of many authors [5, 9, 10, 18].
A proposed approach to the hip and upper femur is adapted to allow for a better exposure. The required shortening, derotation and varization if needed, alongside any pelvic procedure, can be performed and stability tested with the hip exposed under direct vision. The only disadvantage is the unsightly scar which is near to that of Smith Peterson utilized by some authors [10, 17]. Using two separate incisions, a bikini for the hip and another straight incision for the femoral shaft for cosmetic reasons, will not offer such an excellent exposure for a successful reconstruction.
The mean period of follow up in most recent studies was 3 [21], 6.2 [18], and 7.1 [19] years, which is not a long enough period for evolving osteoarthritic changes to show up in young patients. The same applies for the current study (5.3 years).
Complications encountered in this study are limited and could be avoided if care is given to the technical details. This entails a generous clear exposure of the hip and upper femur, performing adequate femoral shortening, with correctly estimated derotation allowing the femoral head to be easily reduced into the well-reconstructed acetabulum, preventing undue pressure exerted over the femoral head and ending with a tight capsulorrhaphy.
The author believes that surgical reconstruction for children above 8 years of age carries almost the same principles applied for younger patients, yet acetabular development should not be expected and, accordingly, every effort should be made to reconstruct it. This applies for unilateral and bilateral DDH. There is no evidence to support the deterioration of such hips due to any evolving osteoarthritic changes. If ever this should happen in the future, hip replacement will be made much easier.
Acknowledgments
Thanks go to Dr. Ali M. A. Massoud for his assistance in the operating theater and for collecting the references.
References
- 1.Ashley RK, Larsen LJ, James PM. Reduction of dislocation of the hip in older children: a preliminary report. J Bone Joint Surg Am. 1972;54:545–550. [PubMed] [Google Scholar]
- 2.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg Am. 1984;66:412–420. [PubMed] [Google Scholar]
- 3.Coleman SS. Congenital dysplasia and dislocation of the hip. St. Louis, MO: CV Mosby; 1978. pp. 95–154. [Google Scholar]
- 4.Lindstrom JR, Ponseti IV, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip. J Bone Joint Surg Am. 1979;61:112–118. [PubMed] [Google Scholar]
- 5.Shih CH, Shih HN. One-stage combined operation of congenital dislocation of the hips in older children. J Pediatr Orthop. 1988;8:535–539. doi: 10.1097/01241398-198809000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Galpin RD, Roach JW, Wenger DR, Herring JA, Birch JG. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am. 1989;71:734–741. [PubMed] [Google Scholar]
- 7.Karakaş ES, Baktir A, Argün M, Türk CY. One-stage treatment of congenital dislocation of the hip in older children. J Pediatr Orthop. 1995;15:330–336. doi: 10.1097/01241398-199505000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Klisic P, Jankovic L. Combined procedure of open reduction and shortening of the femur in treatment of congenital dislocation of the hips in older children. Clin Orthop Relat Res. 1976;119:60–69. [PubMed] [Google Scholar]
- 9.Gabuzda GM, Renshaw TS. Reduction of congenital dislocation of the hip. J Bone Joint Surg Am. 1992;74:624–631. [PubMed] [Google Scholar]
- 10.Browne RS. The management of late diagnosed congenital dislocation and subluxation of the hip—with special reference to femoral shortening. J Bone Joint Surg Br. 1979;61:7–12. doi: 10.1302/0301-620X.61B1.422637. [DOI] [PubMed] [Google Scholar]
- 11.McKay DW. A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res. 1974;98:124–132. doi: 10.1097/00003086-197401000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand. 1941;84(Suppl 63):1–142. [Google Scholar]
- 13.McMurry TP. Operative treatment of old unreduced dislocation. 3. London: Edward Arnold; 1949. pp. 335–356. [Google Scholar]
- 14.Salter RB. Textbook of disorders and injuries of the musculoskeletal system. 2. Baltimore, MD: Williams & Wilkins; 1983. pp. 123–131. [Google Scholar]
- 15.Sharrard WJW. Pediatric orthopedics and fractures. 3. Oxford, UK: Blackwell; 1993. pp. 291–357. [Google Scholar]
- 16.Strange CFG. The hip. London, UK: William Heinemann; 1965. pp. 56–86. [Google Scholar]
- 17.Papavasiliou VA, Papavasiliou AV. Surgical treatment of developmental dysplasia of the hip in the periadolescent period. J Orthop Sci. 2005;10:15–21. doi: 10.1007/s00776-004-0850-z. [DOI] [PubMed] [Google Scholar]
- 18.Vallamshetla VRP, Mughal E, O’Hara JN. Congenital dislocation of the hip. A re-appraisal of the upper age limit for treatment. J Bone Joint Surg Br. 2006;88:1076–1081. doi: 10.1302/0301-620X.88B8.17592. [DOI] [PubMed] [Google Scholar]
- 19.Ok IY, Kim SJ, Ok JH. Operative treatment of developmental hip dysplasia in children aged over 8 years. J Pediatr Orthop Br. 2007;16:256–261. doi: 10.1097/BPB.0b013e32801088f1. [DOI] [PubMed] [Google Scholar]
- 20.Harris NH. Acetabular growth potential in congenital dislocation of the hip and some factors upon which it may depend. Clin Orthop Relat Res. 1976;119:99–106. [PubMed] [Google Scholar]
- 21.Dogan M, Bozkurt M, Sesen H, Yildirim H. One-stage treatment of congenital severely dislocated hips in older children through various acetabuloplasty techniques: 22 children followed for 1–5 years. Acta Ortho Pediatr. 2005;76:212–219. doi: 10.1080/00016470510030599. [DOI] [PubMed] [Google Scholar]
- 22.Ryan MG, Johnson LO, Quanbeck DS, Minkowitz B. One-stage treatment of CDH in children 3 to 10 years old. Functional and radiographic results. J Bone Joint Surg Am. 1998;80:336–344. doi: 10.2106/00004623-199803000-00005. [DOI] [PubMed] [Google Scholar]


