Abstract
Purpose
This study presents our experience with the Ponseti method of manipulation and casting followed by Achilles tenotomy (AT) in children with arthrogryposis multiplex congenita (AMC).
Methods
Five children (ten feet) were followed for at least 24 months after the AT and are the cohort for this study. Their mean age at follow-up was 38.4 months (26 to 48 months), and the average follow-up period was 35.8 months (24–44 months). Treatment was begun within the first months of life. The AT to correct rigid equinus was performed at a mean of 14.4 weeks of life, after 7–10 cast changes (mean 8.4). Clinical criteria by Niki et al. and standard standing AP and lateral radiographs were analyzed for final evaluation. Efficacy of Ponseti casting and AT tenotomy was assessed according to the amount and continuance of the achieved correction.
Results
Seven feet had clinically satisfactory results. Among the three unsatisfactory feet, there were two (one child) with rocker-bottom pseudocorrections after repeated bilateral AT and one recurrent clubfoot (one child). Six feet required soft tissue releases at 3, 12 and 21 months after the AT due to recurrence of moderate equinus and adductus. Three feet (two children) underwent repeat AT at 10 and 15 months after the primary procedure. The mean interval between initial AT and redo surgical procedures was 11.8 months (range 3–21 months). Two feet (20%) remained without significant deformity after AT.
Conclusion
Clubfoot in AMC responds initially to the Ponseti method of casting, and deformity may be corrected or diminished. In some children, more extensive surgical treatment can be avoided and in others, delayed. Despite the need for additional surgical intervention, the Ponseti method of casting and AT does seem to be an alternative for initial treatment in children with AMC.
Keywords: Clubfoot, Arthrogryposis, Ponseti casting, Achilles tenotomy
Introduction
Clubfoot is the most frequent indication for surgical treatment in children with arthrogrypotic syndromes [1, 2]. Treatment of the clubfoot in patients with arthrogryposis multiplex congenita (AMC) [3] is a challenge due to foot and ankle stiffness and deformity, resistance to correction, tendency to relapse and coexisting hip and knee contractures [1, 4, 5]. Most orthopedic surgeons agree that initial treatment for arthrogrypotic clubfeet should begin with serial manipulations and casting followed by soft tissue surgical releases [4–6]. There are reports of talectomy or Verberely–Ogston procedure as initial surgical options for arthrogrypotic clubfeet depending on patient age [7–12]. Non-operative treatment for clubfeet in children with AMC very rarely is successful, unless the deformity is exceptionally mild [8].
The Ponseti method of manipulation and casting is now considered the standard initial treatment for idiopathic clubfeet and is also thought to be useful in rigid, teratogenic clubfeet [13, 14]. To our knowledge, reports on the results of initial treatment using parts of the Ponseti protocol in AMC are rare [15]. We present our early experience using Ponseti method manipulation and casting followed by Achilles tenotomy (AT) for clubfeet in children with AMC.
Materials and Methods
We began using Ponseti casting followed by AT to treat AMC clubfeet in 2003, considering it an initial conservative treatment preceding possible need for more extensive soft tissue releases. Between 2003 and 2007, we treated 14 clubfeet in seven children with AMC. Five patients (ten feet) were followed for a minimum of 24 months after the primary AT and represent the final study group (Table 1). This group included two boys and three girls whose mean age at follow-up was 38.4 months (26–48 months) with an average follow-up period of 35.8 months (24–44 months). Three children represented classic four-limb involvement with knee flexion contractures, flexion–abduction–external rotation contractures of the hips, shoulder adduction, elbow extension contractures, and wrist palmar flexion and ulnar deviation [3, 16]. One child had lower limb involvement with knee flexion contractures and bilateral teratologic hip dislocations. The remaining patient presented with clinical symptoms of distal arthrogryposis with rigid extension contractures at the intraphalangeal joints, thumb adduction contractures, left radial congenital dislocation, and bilateral clubfeet [16]. All of these children had bilateral, rigid, stiff–stiff clubfeet according to the Dimeglio classification, with initial Pirani scores of 6.0 [17, 18].
Table 1.
Material, outcomes of casting, heelcord tenotomy, and need for soft tissue release
| Patient | Side | AC type | Age at achillotomy (weeks) | Number of cast changes | Persisted equinus after heelcord tenotomy? | Postero medial release? | Post-op. orthosis |
|---|---|---|---|---|---|---|---|
| L P | Left | Cl. | 8 | 7 | No | No | FAB and taping |
| Right | Cl. | 8 | 7 | No | No | ||
| K N | Left | L.L. | 14 | 8 | Yes | Yes | AFO |
| Right | L.L. | 14 | 8 | Yes | Yes | ||
| K A | Left | Cl. | 14 | 7 | Yes | Yes | AFO |
| Right | Cl. | 14 | 7 | Yes | Yes | ||
| N M | Left | Cl. | 20 | 10 | No | Yes | FAB |
| Right | Cl. | 20 | 10 | No | Yes | ||
| N P | Left | Dist. | 16 | 10 | Yes | Yes | FAB |
| Right | Dist. | 16 | 10 | Yes | Yes | ||
| Mean values | 14.4 | 8 | – | – | – | ||
Cl. classic AC; L.L. lower limb involvment; Dist. distal AC; FAB foot abduction orthosis
During the course of the treatment, one child with four-limb involvement underwent additional surgery in the form of soft tissue releases for bilateral knee flexion contractures. At the age of 15 and 10 months after primary bilateral ATs, through the posterior approach, hamstrings tendons and femoral attachment of gastrocnemius were dissected, which was followed by knee posterior capsuloligamentotomies. After completion of the knee procedures, repeated AT tenotomies were performed during the same surgical session due to bilateral recurrent hindfoot equinus.
All patients had not been treated previously outside our institution, and after being referred to us, underwent primary non-operative clubfoot treatment beginning within the first months of life (average 2.4 weeks) with initial manipulations and casting based on Ponseti’s principles [13]. Manipulations and casting were performed weekly until the forefoot was at least in a neutral position. The number of manipulations and casts varied from 7 to 10 (average 8.4). Residual fixed equinus was an indication for percutaneous AT, which was done under general anesthesia for all children at an average of 14.4 weeks of age (8–20 weeks). Bilateral deformities were corrected in a single session. Our postoperative protocol consisted of 5–9 weeks of immobilization (average 6.6 weeks). A long leg cast with maximal possible foot dorsiflexion and external rotation was applied, initially for 3 weeks, then the casts were changed, and immobilization continued in all children for another 2 weeks to achieve additional correction of the forefoot and possibly to improve ankle dorsiflexion. If any equinus remained 5 weeks after tenotomy, we repeated weekly manipulations and casting. Three children underwent this additional postoperative treatment for 2, 3, and 4 weeks, respectively.
After removing the last cast, six feet (three children) were treated with a foot abduction brace (FAB) with feet positioned in pronation and external rotation. Four feet (two patients) were treated with an ankle–foot orthosis (AFO) during the first 6 months following AT. Those children had severe external contractures of their hip joints; therefore, FABs seemed to increase this concomitant deformity and moreover were poorly tolerated by parents as they considered FAB to be an obstacle in rehabilitation programs. All parents were instructed to perform physical therapy (passive range of motion exercises) on the feet three times daily to maintain correction and ankle movement [15]. Children were to use the FAB or AFO full time during the first 3 postoperative months with brace removal for bathing and therapy. Nighttime-only bracing was then instituted. During the day, the feet were positioned in AFOs or, in one patient, secured in correction with adhesive taping [19, 20], which initially was done daily by us in an out-patient clinic, then continued by parents at home until the child began to stand.
Medical files of all children from the study were reviewed, and all underwent clinical examination. Standing antero-posterior (AP) and lateral radiographs were available for assessment for eight feet (four children). The following parameters were reviewed at the final follow-up visit: (1) walking ability, (2) presence of plantigrade feet, (3) pain complaints, (4) ability to wear conventional shoes, (5) necessity to use orthoses, (6) ankle passive range of motion (ROM), measured with a hand-held goniometer, and (7) time of redo surgery.
The following radiographic measurements were performed: talocalcaneal angle, talometatarsal-first angle on AP views, talocalcaneal angle and tibiocalcaneal angle on lateral views.
Assessment of clinical results was based on criteria described by Niki et al. [6]: a plantigrade, pain-free and braceable foot was considered a satisfactory result, whereas a non-satisfactory result was defined as a non-plantigrade foot with residual deformity necessitating another surgery.
The efficacy of the described treatment was assessed by us if it was possible to achieve correction of the initial deformity with manipulation and casting and equinus correction with the AT with correction maintained between the initial AT and any secondary surgical procedures.
Results
At final follow-up, all five children were pain free. Two children could walk outdoors without any support or orthosis using standard shoes (Fig. 1). Another two children used AFOs and standard shoes for outdoor ambulation. The remaining child, after repeated ATs and bilateral knee posterior releases, walked inefficiently indoors, with the parents’ assistance and KAFOs to improve the stability of his knees.
Fig. 1.
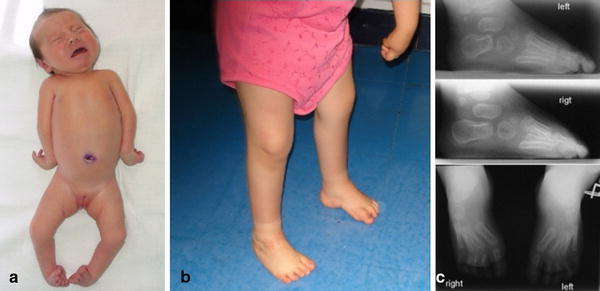
A clinical picture showing a neonate with classic AMC (a) and the same child at the age of 28 months, with clinical (b) and radiographic (c) satisfactory clubfoot correction, after the Ponseti manipulations, casting and AT tenotomy. The left foot required in repeated AT tenotomy 12 months after the initial treatment. Bilateral residual cavus and moderate forefoot supination are present
Age at walking was achieved in the whole group at 17 months on average (15–20 months).
Seven feet (four children) were plantigrade and according to the crieteria of Niki et al. [6] represented satisfactory final results. The remaining three feet (two children) had unsatisfactory results. In one of those children, after repeated bilateral AT, clinical examination revealed bilateral hindfoot varus, cavus and forefoot supination (Fig. 2). Standing radiographs of his feet in AFOs revealed pseudocorrection in the form of hindfoot in varus and equinus, and dorsiflexion through tarso-metatarsal joints (Fig. 3a). The second child presented with unilateral second recurrence of clubfoot deformity following AT and early soft-tissue release. Those feet were treated with repeated surgical corrections (Fig. 3b).
Fig. 2.

A clinical picture of 40-month-old child presenting with bilateral hindfoot equinus and varus, cavus, forefoot supination and adductus after repeated bilateral AT tenotomy and knee flexion contractures releases. Bilateral hip external rotation and residual knee flexion contractures are noted
Fig. 3.
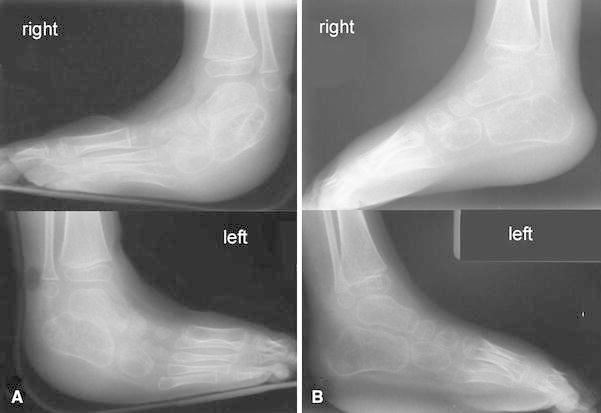
A radiographic picture of the child from Fig 3: (a) standing in AFO: hindfoot equinus and varus, forefoot supination and pseudocorrection through tarso-metatarsal joints. (b) Non-weight-bearing lateral views after postero-medial releases
Moderate residual deformities that did not disturb gait or bracing were seen on clinical examination in five out of seven plantigrade feet and consisted of bilateral cavus and 20° forefoot adduction (two feet, one child), and 10–20° of forefoot adduction in the remaining three feet (two children).
Final examination of passive ankle dorsiflexion was demonstrated to be limited to 10° passive dorsiflexion in three feet (two children), and there was no dorsiflexion in the remaining seven. Mean plantarflexion was 11.5° (5–20°). Radiographic analysis of standing AP and lateral views of eight feet revealed in two feet (one child) bilateral pseudocorrections (equinus and varus positioning of the talocalcaneal complex and dorsiflexion of tarso-metatarsal joints on lateral radiograph) with 115 and 122° of tibiocalcaneal angles on lateral radiographs and talocalcaneal angles of 0° bilaterally. Among the remaining six feet, the mean talocalcaneal angle on AP radiographs was 17° (15–19°) and on lateral view was 17.5° (0–25°). The mean talometatarsal first angle was 135° (115–165°). The mean tibiocalcaneal angle was 89.2° (76–110°)
Medical record review demonstrated that initial weekly manipulations and casting diminished the initial deformity in all feet, although moderate forefoot adduction, which could be passively reduced to neutral position, persisted in all children. Uncorrectable equinus was an indication for AT.
Equinus in four feet (40%, two children) was corrected with the primary AT, and a plantigrade, neutral position of the foot was achieved during the procedure (Fig. 4), although passive ankle dorsiflexion was not obtained.
Fig. 4.

An intraoperative picture demonstrating repeated AT tenotomy. a preoperative 30° recurrent equinus, b neutral foot positioning with the knee in maximal extension, lack of ankle passive dorsiflexion
In the remaining six feet (60%, three children), a residual 10–20°equinus persisted after complete AT. In one child, both feet were not completely corrected by additional serial manipulations and casting, and the patient underwent early posteromedial soft tissue release 3 months after the initial AT. Four feet in two children were corrected to the neutral position with additional postoperative casting. However, equinus and forefoot adduction recurred in those feet, leading to walking or standing difficulties, and resulted in the need for postero-medial releases.
During the follow-up period, nine out of ten feet (90%, all five children) required additional surgical procedures to correct recurrent deformities. The mean time between primary AT and any secondary surgical procedure was 11.8 months (3–21 months).
To correct recurrent equinus, repeated ATs were performed in three feet (two children) after the primary procedure at 10 (bilaterally) and 15 months (unilaterally), respectively.
The remaining six feet (three children), because of more complex relapses, were treated with soft-tissue releases (postero-medial and lateral ankle release, Achilles tenotomy; talonavicular capsulotomy, reposition with K-wire fixation) performed after initial AT tenotomies at 3, 12, and 21 months, respectively.
Discussion
The goals of clubfoot management in arthrogrypotic syndromes include a plantigrade, non-painful foot that allows the patient to wear normal shoes [7, 8]. Prior initial treatment of arthrogrypotic clubfeet has been aggressive surgical techniques [1–12]. The necessity of multiple surgical interventions and high recurrence rate (up to 73%) reported after initial, extensive soft tissue surgery [6] suggest that primary aggressive surgery may not provide satisfactory outcomes, despite short-term results of radical soft tissue releases seeming to be satisfying [5]. We felt that the Ponseti method of manipulation and casting might produce a full or partial clubfoot correction in children with AMC, and thus lead to benefits including avoiding or at least decreasing the range of necessary surgical procedures.
According to Ponseti’s experience, his method may be used to treat so-called “complex” idiopathic clubfeet, which were defined as rigid, teratogenic clubfeet, classified as stiff-stiff in the Dimeglio classification [17], with severe plantar flexion of all metatarsals and deep creases around the heel and sole of the foot. In a recent paper, Ponseti et al. described modification of treatment for such clubfeet, even though syndromic conditions including arthrogrypotic feet were excluded from that study [13]. This previously noted paper supports to some extent the idea of adapting the Ponseti method of manipulation and casting to arthrogrypotic clubfeet. Stiffness, initial severity of the deformity, higher rate of recurrences and difficulties obtaining satisfactory correction with manipulations seem to be common issues with complex and syndromic clubfeet, despite different etiologies.
Although our patient cohort was small and the follow-up period relatively brief, the minimal 2-year period of observation allowed us to observe three trends in this group. Our first view is that arthrogrypotic clubfeet responded to the initial manipulations and castings described by Ponseti, with early complete or partial deformity correction despite initial major rigid deformities (Fig. 5). The number of manipulations and casting needed to obtain satisfactory positioning of the foot was higher on average than reported for idiopathic clubfeet [13, 21]. This may be explained by stiffness of the soft tissues and the need for manipulative corrections in children with AMC to proceed slowly to avoid secondary bony changes, pseudocorrections or fractures [22].
Fig. 5.
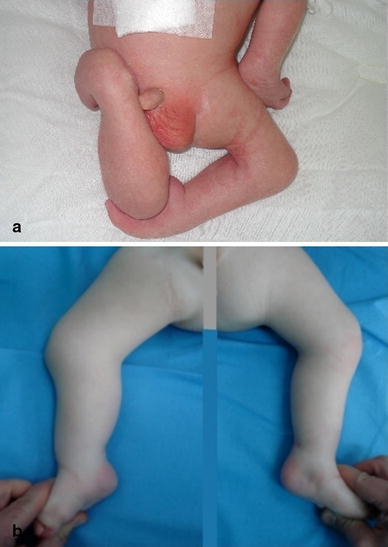
A clinical picture demonstrating initial severe lower limb contractures in a newborn with AMC (a) and the same child 6 months after simultaneous manual corrections of all contractures and Ponseti casting followed by the AT tenotomy for clubfeet. Moderate residual equinus persisted bilaterally (b)
Our second observation was that even complete AT was not always sufficient to correct equinus and bring the foot to a neutral position. Compared to reports on idiopathic clubfeet treatment, when dorsiflexion is expected after AT [13, 19, 20], only four feet from our series (40%) achieved a neutral position following the initial AT, and prolonged casting (2 weeks) did not result in improving ankle dorsiflexion. Six feet obtained only partial equinus correction, and residual equinus was treated by additional manipulation and casting, but this repeated technique did not lead to maintained correction, and additional surgery was required.
Our third observation was that two feet did not require additional soft tissue surgical procedures up to the time of last follow-up. That child was treated with one AT of her right foot and with a repeated AT of the left foot. Non-painful and plantigrade feet remained, giving us a satisfactory result as for arthrogrypotic clubfeet [6]. However, there were residual deformities, in form of cavus and moderate forefoot supination and adductus, which make her further surgical treatment possible (Fig. 1).
The optimal treatment after early relapse or undercorrection following initial manipulations, casting and AT tenotomy in syndromic children is not known. Repeated non-operative treatment is suggested [6], but prolonged casting and immobilization in children with AMC may increase other contractures or may disturb other on-going treatment, especially around the knees, or may lead to pseudocorrections. This is why we decided to perform soft tissue surgery in recurrent clubfeet resistant to the repeated Ponseti casting protocol.
Another question concerns the most appropriate post manipulation and casting bracing protocol for arthrogrypotic feet. Foot Abduction Brace (FAB) use, considered standard in the formal Ponseti method [21, 23], may not be beneficial in children with AMC because of coexisting contractures around hips, especially with fixed hip external rotation. Additionally, gastrocnemius-soleus muscle activation or passive stretching from active knee and hip movement, as seen in normal children in FABs, cannot be expected in children with AMC, since active lower extremity movements are usually quite limited. Noncompliance with classic FAB was reported in idiopathic clubfeet [15, 24] and considered as a factor increasing the risk of recurrence of the deformity, and also was observed in our group, and explained by parents as an obstacle in everyday care and physical therapy. Nevertheless, between exercises, an individually selected bracing method, taking into account coexisting contractures and deformities of the lower extremities, should be used and may include daily taping by instructed parents in maximal dorsiflexion, abduction, and pronation, as described in classic papers [19, 20] or FAB or AFO; however, in our series, children who used AFOs presented with ankle stiffness followed by relapse. We propose that the best way to maintain the correction was via physical therapy (passive range of motion exercises) conducted by an informed parent and controlled by an orthopedic surgeon and therapist. This protocol was adapted by Dobbs et al. to idiopathic, neurogenic, and six syndromic clubfeet and was reported as beneficial to maintain ankle range of motion, which was achieved with AT tenotomy [15]. There are also reports of articulating FAB for idiopathic clubfeet, which are better tolerated than classical FABs [24]. Further investigations need to be performed to asses this type of bracing efficacy and tolerability in children with syndromic clubfeet and to determine the best postoperative bracing protocol for arthrogrypotic clubfeet following Ponseti casting and AT tenotomy.
Prolonged periods of manipulations and casting, performing AT under general anesthesia, troubles with FAB bracing in AMC children, and the need for physical therapy, including ankle range of motion exercises, were the differences between our protocol and the original Ponseti method [13]. Those differences led us to call our method of treatment the Ponseti-like treatment, based on Ponseti's principles of clubfoot pathology, the principles of weekly manipulations and casting, followed by AT tenotomy.
Interpretation of clinical and radiographic results in arthrogrypotic clubfeet remains challenging. There are numerous methods of outcome evaluation for idiopathic clubfeet [25], whereas those concerning syndromic clubfeet are rare [1, 6, 7]. Evaluation systems proposed for idiopathic clubfeet may not be appropriate for syndromic ones. We decided to evaluate the clinical results with Niki et al.'s criteria [6] and the efficacy of the Ponseti method manipulation and casting by two additional criteria: (1) the ability to achieve deformity correction with manipulation and casting, followed by the AT and (2) maintenance of the achieved correction. Following these criteria, in our hands, 40% of the feet had immediate equinus correction, whereas the maintenance of our Ponseti-like protocol lasted for an average of 11.8 months.
Need for radiographic evaluation and control of clubfeet under treatment using various radiographic measurements is controversial since it is often difficult to obtain objective standard radiographs in young children with AMC [1]. Nevertheless, we feel radiographs should be performed during treatment to detect gross pathologies, e.g., pseudocorrections.
Our experience confirms that arthrogrypotic clubfeet recurrences are frequent [1, 4–6] and are seen after Ponseti method casting and AT as well. The 80% rate of need for additional soft tissue surgical releases in our series indicates that the Ponseti method of casting and AT, in cases of syndromic clubfeet, does not provide the excellent results found in management of idiopathic clubfeet. Nevertheless, in AMC children, as in one child of our series, this treatment protocol was able to provide satisfactory, as for syndromic clubfeet, deformity correction maintained at follow-up. In our other patients, the method led to a good initial response and/or partial correction of the deformity. Feet that required additional soft tissue surgery after this protocol were well prepared for it, and the recurrent or undercorrected deformity was moderate (Fig. 5), so aggressive primary surgical procedures, including four-quarter soft tissue releases or salvage talectomy, were avoided during the follow-up period, which limited the potential of further scaring and stiffness. The Ponseti protocol of manipulation and casting, followed by AT tenotomy, being a minimally invasive method, seems to be a useful alternative in the initial treatment of arthrogrypotic clubfeet, despite the usually transitory correction and frequent subsequent need for soft tissue or more aggressive surgery.
References
- 1.Sodergard J, Ryoppy S. Foot deformities in arthrogryposis multiplex congenita. J Pediatr Orthop. 1994;14(6):768–772. doi: 10.1097/01241398-199414060-00015. [DOI] [PubMed] [Google Scholar]
- 2.Guidera KJ, Drennan JC (1985) Foot and ankle deformities in arthrogryposis multiplex congenita. Clin Orthop Relat Res 194:93–98 [PubMed]
- 3.Bernstein RM. Arthrogryposis and amyoplasia. J Am Acad Orthop Surg. 2002;10(6):417–424. doi: 10.5435/00124635-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Widmann RF, Do TT, Burke SW. Radical soft-tissue release of the arthrogrypotic clubfoot. J Pediatr Orthop B. 2005;14(2):111–115. doi: 10.1097/01202412-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Chang CH, Huang SC. Surgical treatment of clubfoot deformity in arthrogryposis multiplex congenita. J Formos Med Assoc. 1997;96(1):30–35. [PubMed] [Google Scholar]
- 6.Niki H, Staheli LT, Mosca VS. Management of clubfoot deformity in amyoplasia. J Pediatr Orthop. 1997;17(6):803–807. [PubMed] [Google Scholar]
- 7.Cassis N, Capdevila R. Talectomy for clubfoot in arthrogryposis. J Pediatr Orthop. 2000;20(5):652–655. doi: 10.1097/01241398-200009000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Lloyd-Roberts CG, Lettin AWF. Arthrogryposis multiplex congenita. J Bone Joint Surg Br. 1970;52:494–508. [Google Scholar]
- 9.Letts M, Davidson D. The role of bilateral talectomy in the management of bilateral rigid clubfeet. Am J Orthop. 1999;28(2):106–110. [PubMed] [Google Scholar]
- 10.Spires TD, Gross RH, Low W, Barringer W. Management of the resistant myelodysplastic or arthrogrypotic clubfoot with the Verberely–Ogston procedure. J Pediatr Orthop. 1984;4(6):705–710. doi: 10.1097/01241398-198411000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Gross RH. The role of the Verberely–Ogston procedure in the management of the arthrogrypotic foot. Clin Orthop Relat Res. 1985;194:99–103. [PubMed] [Google Scholar]
- 12.Solund K, Sonne-Holm S, Kjolbye JE. Talectomy for equinovarus deformity in arthrogryposis. A 13 (2–20) year review of 17 feet. Acta Orthop Scand. 1991;62(4):372–374. doi: 10.3109/17453679108994473. [DOI] [PubMed] [Google Scholar]
- 13.Ponseti IV, Smoley EN. Congenital clubfoot: the results of treatment. J Bone Joint Surg Am. 1963;45A:2261–2275. [Google Scholar]
- 14.Ponseti IV, Zhivkov M, Davis N, Sinclair M, Dobbs MB, Morcuende JA. Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res. 2006;451:171–176. doi: 10.1097/01.blo.0000224062.39990.48. [DOI] [PubMed] [Google Scholar]
- 15.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment for idiopathic clubfeet. J Bone J Surg Am. 2004;86 A-(1):22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Hall JG. Arthrogryposis multiplex congenita: etiology, genetics, classification, diagnostic approach, and general aspects. J Pediatr Orthop B. 1997;6:159–166. doi: 10.1097/01202412-199707000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Dimeglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B. 1995;4:129–136. doi: 10.1097/01202412-199504020-00002. [DOI] [PubMed] [Google Scholar]
- 18.Dyer PJ, Davis N. The role of the Pirani scoring system in the management of club foot by the Ponseti method. J Bone Joint Surg Br. 2006;88(8):1082–1084. doi: 10.1302/0301-620X.88B8.17482. [DOI] [PubMed] [Google Scholar]
- 19.Fripp AT, Shaw NE (1967) Clubfoot. E and S Livingstone, Edinburgh and London
- 20.Turco VJ (1981) Clubfoot. Current Problems in Orthopaedics. Churchill Livingstone
- 21.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics. 2004;113(2):376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 22.Gravev AM, Boal DK, Wallach DM, Segal LS. Metaphyseal fractures mimicking abuse during treatment for clubfoot. Pediatr Radiol. 2001;31(8):559–563. doi: 10.1007/s002470100497. [DOI] [PubMed] [Google Scholar]
- 23.Thacker MM, Scher DM, Sala DA, van Bosse HJ, Feldman DS, Lehman WB. Use of the foot abduction orthosis following Ponseti casts: is it essential? J Pediatr Orthop. 2005;25(2):225–228. doi: 10.1097/01.bpo.0000150814.56790.f9. [DOI] [PubMed] [Google Scholar]
- 24.Chen RC, Gordon JE, Luhmann SJ, Shoenecker PL, Dobbs MB. A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop. 2007;27(5):522–528. doi: 10.1097/bpo.0b013e318070cc19. [DOI] [PubMed] [Google Scholar]
- 25.Bensahel H, Kuo K, Duhaime M. the International Clubfoot Study Group: Outcome evaluation of the treatment of clubfoot: the international language of clubfoot. J Pediatr Orthop B. 2003;12(4):269–271. doi: 10.1097/01.bpb.0000078720.48512.a5. [DOI] [PubMed] [Google Scholar]


