Abstract
Purpose
Severe Blount’s disease results in a multiplanar deformity of the lower limb. The mechanical axis is disrupted, there is a rotational deformity, and also shortening of the limb. A depression of the medial tibial plateau causes joint incongruity and instability. The purpose of this study is to review the results of treatment addressing all the aspects of the deformity.
Methods
Four patients were treated for severe Blount’s disease. The index procedure consisted of a medial tibial plateau elevating osteotomy, a lateral tibial and proximal fibular epiphysiodesis, a proximal tibial metaphyseal osteotomy, and the application of the Taylor Spatial Frame programmed for correction of varus, rotation and shortening, and preemptive lengthening to compensate for growth arrest.
Results
Mechanical axis was corrected from a mean 23° (13°–30°) to 0° in three patients and 6° valgus in 1. Tibias were lengthened by 1–4 cm. At follow-up, the mechanical axis was 0° in two patients and 7° varus in two. The overlengthening was diminishing as planned.
Conclusions
The double osteotomy and Taylor Frame correction was found to be accurate, safe, and effective for multiplanar deformity correction in severe Blount’s disease.
Keywords: Blount’s disease, Tibia vara, Osteotomy, Plateau elevation, External fixator, Taylor Spatial Frame
Introduction
The treatment of Blount’s disease varies with the age of the patient as well as the stage of the disease. In the early stage of the disease, the process is reversible and a correction of the mechanical axis by a metaphyseal osteotomy can restore normal physeal growth.
However, in the advanced stage of the disease, there is a bony bridge formation with medial plateau depression, joint instability, and leg length inequality, all of which have to be addressed by the proposed treatment.
We present our experience in the treatment of four cases of severe early onset Blount’s disease by an elevation of the medial tibial plateau to restore joint congruity, a lateral hemiepiphysiodesis to prevent recurrence and a proximal tibial metaphyseal osteotomy using the Taylor Spatial Frame™ (Smith and Nephew Richards, Memphis TN, USA) to correct the mechanical axis of the limb and address future leg length discrepancy.
Materials and methods
Four patients with severe early onset Blount’s disease were treated at our institution between July 2004 and December 2005. After approval from our institutional review board, all patients' charts and radiographs were reviewed. Patient demographics are given in Table 1. Mean age was 8.1 years (6.9–9.1). Three patients had bilateral disease. Clinically, all four patients complained of knee pain preoperatively. Upon examination, all patients demonstrated a progressive varus deformity of the knee (Fig. 1a). All walked with a thrust and had a degree of medial–lateral knee instability. Three patients had no previous surgical treatment. The fourth patient had undergone a corrective metaphyseal osteotomy with recurrence of the deformity within 1 year.
Table 1.
Patient demographics and preoperative deformity
| No. | Patient | Gender | Age | Mechanical varus (°) | MPTA (°) | Internal torsion (°) | Leg length discrepancy |
|---|---|---|---|---|---|---|---|
| 1 | MY | F | 6.9 | 13 | 60 | 0 | 0 |
| 2 | IE | F | 7.3 | 30 | 42 | 10 | 0 |
| 3 | BM | M | 9.1 | 26 | 50 | 0 | 1 cm |
| 4 | SE | M | 9.1 | 22 | 43 | 10 | 2 cm |
Fig. 1.
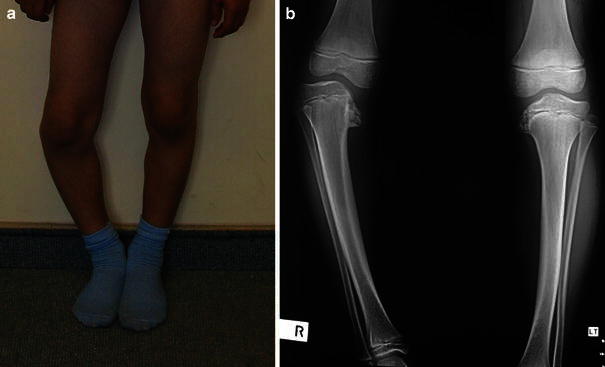
a Case 4: preoperative clinical picture. b Case 4: preoperative radiograph
Radiographically, all patients had Langenskiold stage V and VI disease (Fig. 1b). Mechanical varus averaged 23° (13–30°) and medial axis deviation was a mean 5 cm [1–4]. Medial proximal tibial angle (MPTA) was a mean 49° (42°–60°) (N = 85–90°). Two patients had internal tibial torsion and two had a leg-length discrepancy with a relative shortening of 1–2 cm on the affected side (Table 1).
Surgical procedure
An arthrogram is performed, which gives information regarding the true joint surface orientation and stability.
A peroneal nerve release was performed in three of the four cases. An epiphysiodesis of the proximal fibula is performed through the same incision and a hemiepiphysiodesis of the lateral tibia is performed through the same incision or through a percutaneous additional incision. Through another more-distal incision, a fibulectomy is performed, removing a 1.5-cm fibular segment.
The first osteotomy of the medial tibial plateau is started proximal or distal to the insertion of the medial collateral ligament depending on its tightness or attenuation. The osteotomy is curved towards the intercondylar eminence without violating the joint surface. The plateau is elevated and supported by a bone graft utilizing the resected fibula with an addition of a tricortical iliac crest graft if necessary. Fixation is performed utilizing one or two 3.5-mm screws (Fig. 2a). A regular radiograph is then obtained in both planes. This is important since the deformity parameters for the spatial frame program have been changed by the intra-articular osteotomy.
The Taylor Frame is applied. Struts are dismantled, a proximal metaphyseal osteotomy is performed using a Gigli saw, the skin is closed and the struts are reapplied (Fig. 2b).
A radiograph is obtained orthogonally to the proximal ring and mounting parameters are measured. The data is entered into the Spatial Frame Web site using the Total Residual Program with a proximal reference ring and a planned overlengthening according to age. Correction is started between day 5 and 7.
Fig. 2.
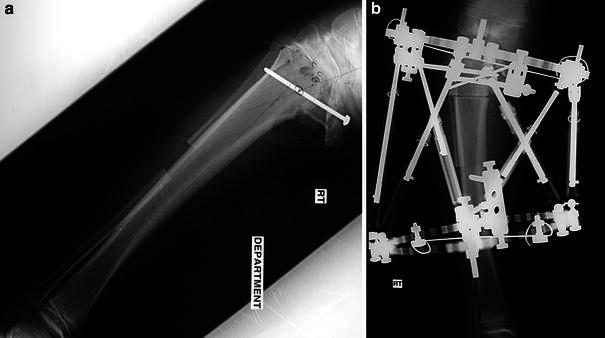
a Case 4: intraoperative radiograph after tibial plateau elevation. b Case 4: postoperative radiograph
Concomitant surgery
Three of the four patients had contralateral involvement. One patient had a concomitant contralateral epiphysiodesis of the lateral proximal tibia and the proximal fibula. In the other two patients the disease was mild and we elected not to treat it at this stage.
Results
Three of the patients had the full procedure performed in one sitting. In one patient the surgery was staged. Following the tibial plateau elevation, it was felt that due to the large correction, a second osteotomy may cause skin closure problems and it was elected to stage the procedure. This patient also had a concomitant lateral hemiepiphysiodesis of the tibia and fibular epiphysiodesis of the contralateral knee. The TSF application and lengthening were therefore performed 7 months later. The mean correction time was 21 days (15–27) with consolidation taking between 6 and 13 weeks (mean 10 weeks) for a total treatment time of 11–16 weeks—mean 14, and a lengthening index of 35 days/cm (22–83) (Fig. 3). Three of the four patients were fully ambulatory with the frame.
Fig. 3.

Case 4: at end of correction and 4-cm lengthening
At frame removal, the mechanical axis was corrected to 0° in three patients and to 6° valgus in one patient. Tibial Torsion was 0° in three patients and 15° external in one.
A pre-emptive overlengthening of 1–4 cm was obtained—as planned. There were two complications: one transient dropfoot and one knee flexion contracture requiring a hamstring release. Both were in the patient who had not undergone a peroneal nerve release and were found to have resolved at final follow-up. Mean latest follow-up was 29 months (24–38) after frame removal. Age at follow-up was 10 years and 3 months to 11 years and 9 months. All four patients were found to be fully active and free of pain. All knees were stable on examination and had full range of motion.
Two patients had a mechanical axis of 0°, and two had a partial recurrence to 7° varus, however, the varus was stable over the preceding 1 year. The relative overlengthening was decreasing as planned and was found to be 0–2 cm (Fig. 4a, b).
Fig. 4.

a Case 4: clinical picture at 2-year follow-up. b Case 4: radiograph at 2-year follow-up; deformity has recurred to 7° but is non-progressive. Residual overlengthening of 1.5 cm
Discussion
Blount’s disease is a growth-plate disorder. In the early stages of the disease (when the medial growth plate is still functional) correction can be obtained by axis realignment [5, 6]. However, in the advanced stages, the growth plate undergoes irreversible changes with formation of a bony bridge. The resultant deformity causes a disruption of the normal mechanical axis of the limb and with further progression—a depression of the medial tibial plateau with resultant joint incongruity and instability. In unilateral or asymmetric cases, a leg-length inequality will develop due to both the growth arrest and the varus deformity.
Restoration of growth plate function in these more advanced cases has been described by resection of the bony bridge and interposition of fat or silastic [1]. However, the results of these procedures are not always predictable, and in addition, they do not address the existing axis and joint deformity.
Previous studies have addressed various aspects of the deformity, with correction being performed either acutely—using internal fixation [2–4, 7], or gradually, using an Ilizarov apparatus [8–11]. Only one previous author has described use of the Taylor Spatial Frame in Blount’s disease [12, 13], however, no intra-articular correction was performed in this series. This is, to our knowledge, the first report combining intra-articular deformity correction using the Taylor Spatial Frame.
The current procedure corrects all aspects of the deformity, both within the knee joint as well as the overall alignment of the limb. It also addresses the leg-length issue. The patients usually have a pre-existing leg-length discrepancy due to both the growth disturbance and the deformity. As we do not restore medial growth plate function, we ablate the lateral growth plate to prevent deformity recurrence, and the future leg-length discrepancy is addressed by a pre-emptive lengthening. Considering a proximal tibial growth of 0.6 cm/year, one can expect an equalization of leg lengths in our patients 4–5 years postoperatively—at age 13–14 years at which time a decision can be made for either a contralateral epiphysiodesis or an ipsilateral relengthening. Regarding the need for a peroneal nerve release, peroneal neuropathy has been shown to occur after both varus and valgus osteotomies [14–16]. The planned lengthening in the present procedure further necessitates a release and the neuropathy encountered in the one patient on whom it was not performed leads us to recommend a peroneal release for all patients undergoing the procedure.
The reason for the partial recurrence we encountered in two patients is unclear. It may have been due to an incomplete lateral epiphysiodesis, or to a mild distal femoral varus [17]. However, after the initial recurrence, this remained constant and did not pose a problem requiring further treatment.
The use of the Taylor Spatial Frame as opposed to the Ilizarov apparatus has the advantage of simultaneous correction of all six parameters of deformity. It is significantly more “user friendly” for the patient or parent performing the correction, and does not necessitate the change of hinges required in the Ilizarov apparatus for correction of the rotational deformity.
We therefore conclude that the method described is safe and effective for the treatment of severe Blount’s disease.
Acknowledgments
No financial support was received for this study.
References
- 1.Beck CL, Burke SW, Roberts JM, Johnston CE. Physeal bridge resection in infantile Blount disease. J Pediatr Orthop. 1987;7:161–163. doi: 10.1097/01241398-198703000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Martin SD, Moran MC, Martin TL, Burke SW. Proximal tibial osteotomy with compression plate fixation for tibia vara. J Pediatr Orthop. 1994;14:619–622. doi: 10.1097/01241398-199409000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Sasaki T, Tomonori Y, Monji J, Yasuda K, Kanno Y. Transepiphyseal plate osteotomy for severe tibia vara in children: follow-up study of four cases. J Pediatr Orthop. 1986;6:61–65. doi: 10.1097/01241398-198601000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Gregosiewicz A, Wosko I, Kandzierski G, Drabik Z. Double-elevating osteotomy of tibiae in the treatment of severe cases of Blount’s disease. J Pediatr Orthop. 1989;9:178–181. [PubMed] [Google Scholar]
- 5.Rab GT. Oblique tibial osteotomy for Blount’s disease. J Pediatr Orthop. 1988;8:715–720. doi: 10.1097/01241398-198811000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Langenskiold A. Tibia vara: osteochondrosis deformans tibiae. Blount’s disease. Clin Orthop Relat Res. 1981;158:77–82. [PubMed] [Google Scholar]
- 7.Schoenecker PL, Johnston R, Rich MM, Capelli AM. Elevation of the medial plateau of the tibia in the treatment of Blount disease. J Bone Joint Surg. 1992;74-A:351–358. [PubMed] [Google Scholar]
- 8.Jones S, Hosalkar HS, Hill RA, Hartley J. Relapsed infantile Blount’s disease treated by hemiplateau elevation using the Ilizarov frame. J Bone Joint Surg. 2003;85-B:565–571. doi: 10.1302/0301-620X.85B4.13602. [DOI] [PubMed] [Google Scholar]
- 9.Accadbled F, Laville JM, Harper L. One step treatment for evolved Blount’s disease. J Pediatr Orthop. 2003;23:747–752. doi: 10.1097/01241398-200311000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Hefny H, Shalaby H, El-kawy S, Thakeb M, Elmoatasem E. A new double elevating osteotomy in management of severe neglected infantile tibia vara using the Ilizarov technique. J Pediatr Orthop. 2006;26:233–237. doi: 10.1097/01.bpo.0000218530.59233.ab. [DOI] [PubMed] [Google Scholar]
- 11.Janoyer M, Jabbari H, Rouvillain JL, Sommier J, Py G, Catonne Y, et al. Infantile Blount’s disease treated by hemiplateau elevation and epiphyseal distraction using a specific external fixation: a preliminary report. J Pediatr Orthop B. 2007;16:273–280. doi: 10.1097/01.bpb.0000210591.35652.84. [DOI] [PubMed] [Google Scholar]
- 12.Feldman DS, Madan SS, Koval KJ, van Bosse HJ, Bazzi J, Lehman WB. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop. 2003;23(3):387–391. [PubMed] [Google Scholar]
- 13.Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006;26:794–798. doi: 10.1097/01.bpo.0000242375.64854.3d. [DOI] [PubMed] [Google Scholar]
- 14.Slawski DP, Schoenecker PL, Rich MM. Peroneal nerve injury as a complication of pediatric tibial osteotomies. J Pediatr Orthop. 1994;14(2):166–172. doi: 10.1097/01241398-199403000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Pinkowski JL, Weiner DS. Complications in proximal tibial osteotomies in children with presentation of technique. J Pediatr Orthop. 1995;15(3):307–312. doi: 10.1097/01241398-199505000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Payman KR, Patenall V, Borden P, Green T, Otsuka NY. Complications of tibial osteotomies in children with comorbidities. J Pediatr Orthop. 2002;22(5):642–644. [PubMed] [Google Scholar]
- 17.van Huyssteen AL, Hastings CJ, Olesak M, Hoffman EB. Double-elevating osteotomy for late-presenting infantile Nlount’s disease: the importance of concomitant lateral epiphysiodesis. J Bone Joint Surg. 2005;87-B:710–715. doi: 10.1302/0301-620X.87B5.15473. [DOI] [PubMed] [Google Scholar]


