Abstract
Purpose
Idiopathic congenital talipes equinovarus (CTEV) is a relatively common complex deformity of the foot that can be successfully managed by the Ponseti method. The purpose of this study was to see if the latter can be effectively administered by non-medical specialists outside a specialist or teaching hospital setting.
Method
Retrospective review of 24 children (39 feet) with idiopathic congenital talipes equinovarus managed by a physiotherapist-led service in a district general hospital.
Results
The median Pirani score at presentation was 4.5 (mean 4.2, range 1.5–6). The median Pirani score for feet requiring tenotomy was 6 (4.5–6), whereas feet not requiring tenotomy had a median Pirani score of 2.5 (1.5–5). A total of 18 feet (46%) underwent an Achilles tenotomy. Foot correction was achieved with an average of 3.4 (2–6) cast changes in the non-tenotomy group, and an average of 7.5 (5–13) in the tenotomy group. Successful initial correction of the deformity was achieved in 37 (95%) of the feet studied. One patient (2 feet, 5%) failed local conservative management, requiring tertiary referral. Two children (2 feet) have relapsed, requiring further serial casting. No children required open surgical release. Follow-up was for a mean of 31 months (17–50).
Conclusions
Early results suggest that a combined consultant/physiotherapist-delivered Ponseti service can be effectively and successfully administered in a district general hospital.
Keywords: Congenital talipes equinovarus, Ponseti, Multi-disciplinary, District general hospital
Introduction
Idiopathic congenital talipes equinovarus (CTEV) is a relatively common complex three-dimensional deformity of the foot affecting approximately 1–2/1,000 newborns. The long-term aims of treatment are a pain-free, flexible, functional foot, with good mobility and tolerating normal footwear. Treatment remains controversial as initial correction can be achieved by surgical or non-surgical means or a combination of both. The traditional treatment for clubfoot may involve a combination of initial casting, extensive posterior medial soft tissue releases and bony procedures, followed by further casting [1]. This treatment is associated with significant risks, complications, and a potential for poorer prognosis with patients developing weak, stiff and scarred feet [2, 3]. Follow-up studies have also shown that these feet have a higher incidence of pain and their gait is affected [2–4].
A more conservative technique pioneered by Ignacio Ponseti at the University of Iowa involves serial corrective manipulation and casting to reduce the deformity, with subsequent splinting in a foot abduction splint [5]. A percutaneous Achilles tenotomy is also often required. Ponseti's method has a success rate of over 90% and results in fewer complications than traditional surgical methods [6]. Current literature has emphasised the reproducibility of these excellent results, outside its centre of origin, among multiple centres throughout the world [7–9].
Ponseti’s method, however, is a time-intensive treatment modality associated with a significant learning curve. Paediatric orthopaedic consultants, assisted by junior doctors, physiotherapists, nurses, plaster technicians or orthotists, traditionally lead the Ponseti method, applying the weekly casts. Two recent studies have shown good results have been achieved when the Ponseti method is performed by trained clinical specialists in either a teaching hospital setting or in a developing country [10, 11].
It has already been shown that a physiotherapist-led service in a large teaching hospital can successfully manage CTEV [10]. In our study, we looked at whether similar results could also be achieved by our physiotherapy-delivered Ponseti service in a medium-sized district general hospital (DGH).
Materials and methods
A Ponseti service was set up at our DGH in March 2004 and the results were collated prospectively and reviewed. All congenital talipes equinovarus deformities referrals were made to the senior author (C.J.C.) who informed the extended scope practitioner (ESP) (K.B. or M.D.). The latter are senior paediatric physiotherapists, who attended the 2nd and 3rd Manchester International Club Foot Conference in 2003 and 2005, and have been working closely with the senior author for over 4 years.
An outline of the physiotherapist-delivered pathway is seen in chart 1. Patients referred as structural talipes ante-natally are seen within 2 weeks of referral, post-natal referrals are seen either on postnatal wards or as an outpatient within a week. At initial consultation parents are given an explanation of the treatment options, information leaflets, Steps DVDs and shown the stages with representative casting models. No parents declined enrolment in the program. Ideally treatment is commenced at 2 weeks of age (post ideal term). This allows the parents to establish feeding and get to know their baby. The baby is also assessed by a paediatrician to ensure the clubfoot is not associated with any other condition.
Chart 1.
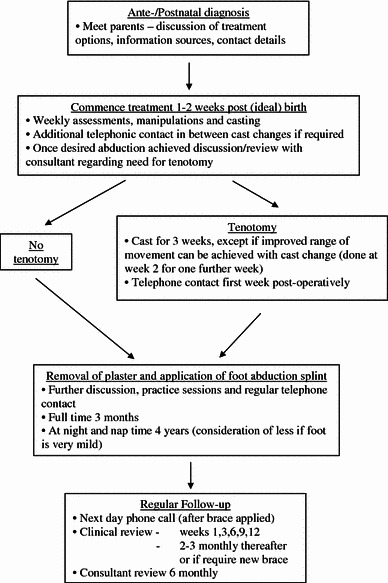
ESP Physiotherapist-delivered pathway for management of CTEV
Between March 2004 and December 2006, 25 children (42 feet) were referred to and assessed by K.B. and/or M.D. All feet had idiopathic congenital talipes equinovarus with no syndromic association. One patient (premature triplet) had an idiopathic fixed flexion deformity of an elbow and a developmental dysplasia of the hip, that failed to reduce with conservative management and a closed hip reduction, and is currently awaiting an open hip procedure. Of the referrals, one patient had already undergone serial casting and an Achilles tenotomy at two other centres and was thus excluded from the study. In another patient referred with “bilateral” CTEV, one foot which only had a midfoot deformity (Pirani score 1) that had failed to respond to stretching, was also excluded as it was not considered a case of true CTEV. This left 24 patients (39 feet) for analysis. Two patients, referred from external sources, had failed prior serial casting or stretching. As their Pirani scores had not improved from initial presentation, we decided to include them in our study.
Pirani scoring [12] was performed by the physiotherapist on all feet at presentation and repeated weekly at subsequent reviews. All manipulations and serial casting were performed by an ESP physiotherapist and in the majority of cases both ESPs were present. In the event of absenteeism, a trained paediatric physiotherapy colleague assisted. For casting material, Webril® (Kendall, Covidien LP, Mansfield, MA, USA) was used as undercast padding, followed by 5 cm Gypsona (Smith & Nephew) plaster of Paris. For the older child, the plaster was further enforced with 3MTM soft cast (3M Health Care, Loughborough, UK).
Once foot abduction to 50–60° had been achieved, a joint decision between ESP and consultant regarding the need for tenotomy was made. A tenotomy was performed if dorsiflexion was ≤10° (measured with goniometer) with the knee extended. In the complex foot, the foot was not abducted beyond 40° prior to the tenotomy [13]. All tenotomies were performed under a brief general anaesthetic (inhalational, paediatric consultant anaesthetist) in the anaesthetic room by the senior author (C.J.C.) or orthopaedic registrar under supervision. Using a size 15 scalpel blade, a small stab incision on the medial aspect of the Achilles tendon was made and the tenotomy performed. The wound was closed with steristrips and a cast applied. Parents were warned about the risk of blood-staining on the plaster and given advice.
In our hospital, we have been using the Markell abduction braces. If the foot was considered to be complex or tolerance was an issue, the Mitchell abduction brace was used instead. The children wear the boots and bars for 23 h a day for 3 months and then at night and nap times until they are 4 years of age to maintain the correction.
All families had contact details of the paediatric physiotherapy department and open access to book an appointment at the paediatric orthopaedic clinic. Apart from formal consultant involvement pre initial casting, at tenotomy and orthopaedic review at certain follow-up intervals (6 monthly), all patient and parent contact was with the physiotherapist.
Results
Patient cohort demographics are summarised in Table 1. Treatment was commenced at a mean of 27.2 days (median 21, range 7–114) post-referral. The wide range was as a result of delays in initiating treatment secondary to a high number of prematurely born patients (7 patients, 9 feet), patients being incorrectly referred as “positional talipes equinovarus” (2 patients, 2 feet) and hence being seen in outpatients at 4–6 weeks post birth, delay from external source referral (1 patients, 2 feet—referred age 105 days), or patients being unwell and delaying treatment for medical reasons (1 patient, 1 foot). For the pre-term patients, treatment was delayed until the baby was post ideal term, stable, for purposes of the (potential) tenotomy, and to allow for the size of the “boots and bars” when it came to fitting.
Table 1.
Patient demographics
| Number of patients:feet | 24:39 |
| Diagnosis—prenatal:postnatal (patients) | 10:14 |
| Males:females (patients) | 16:8 |
| Involvement (feet)—unilateral:bilateral | 9:15 |
| Left:right (feet) | 21:18 |
| Non-complex:complex (feet) | 34:5 |
Overall foot correction was achieved with a mean of 6.3 casts (range 2–13) and an Achilles tenotomy was required in 18 feet (46%). The median Pirani score at presentation was 4.5 (mean 4.2, range 1.5–6). The median Pirani score for those feet requiring tenotomy was 6 (4.5–6), whereas those feet not requiring tenotomy had a median Pirani score of 2.5 (1.5–5). Children who did not need a tenotomy required a mean of 3.4 (2–6) cast changes, while those that did need a tenotomy required an average of 7.5 (5–13) cast changes (including post-tenotomy casts) . Our Pirani score pre- and post-treatment is tabulated in table 2.
Table 2.
Summary of median (and range) Pirani scores during our Ponseti protocol
| At presentation | No tenotomy group (n = 21 feet) | Tenotomy group (n = 18 feet) | Pre-tenotomy | Post-tenotomy | At time of bracing | At latest follow-up |
|---|---|---|---|---|---|---|
| 4.5 (1.5–6) | 2.5 (1.5–5) | 6 (4.5–6) | 2.5 (2–3) | 1 (0–1.5) | 0.5 (0–1.5) | 0 (0–1.5) |
Function
Children were followed up for a mean of 31 months (range 17–50). Walking age for patients was a mean of 14 months (range 8–21). At latest follow-up, the median Pirani score is 0 (mean 0.4, range 0–1.5). We found that, after tenotomy and satisfactory correction, feet have a residual empty heel sign or slight old medial marks which diminish over time and weight-bearing.
Compliance and relapses
To date, compliance with the foot abduction brace has been 100%. Two relapses (2 feet, with initial Pirani scores of 5 and 6, both requiring tenotomies) have occurred; both required further casting for 1–2 weeks. All presented after growth spurts. One child required two re-casts on separate occasions as he was not tolerating his boots and bars. The second child had drifted into mild heel varus and had a very active tibialis anterior affecting gait. He may require an anterior tibialis tendon transfer at a later date.
Complications
One cast was removed over concerns for circulation, and one cast broke and needed to be changed early. Out of 246 applied casts, 5 slipped (4 in patient with complex feet, who needed tertiary referral). One patient had a week out of plaster due to a pressure area over the head of the talus. In the event of redness we now apply DuoDERMTM (ConvaTec, Bristol-Myers Squibb, Victoria, Australia) over the affected area.
Failures
One patient with atypical complex clubfeet required tertiary referral for repeated plaster slippages and failure to progress with our standard Ponseti management. At the tertiary centre, under an ESP physiotherapist, he underwent further serial casting with a tenotomy. He did not require more aggressive surgery.
Discussion
In 2004, a combined consultant/physiotherapy-led Ponseti service was set up at our DGH, to try to alleviate the time and financial pressures of specialist consultant led medical care. Prior to this, the senior author (C.J.C.) managed all referrals directly and the deformity was managed initially by physiotherapists using strapping or medial slabs, but in the majority of cases they required an operative postero-medial release. The role of ESPs in orthopaedic outpatients has already been established [14, 15] and shown to be effective in managing CTEV [10, 11].
Ponseti’s method has excellent both short- and long-term outcomes, with the result that its practice is expanding worldwide [3, 6, 16, 17]. Although our study is small, with short follow-up, the early results (success rate of 95%) are encouraging and compare favourably with those achieved by other centres [6–10].
Being a DGH, we are likely to see milder cases than tertiary referral centres, and our wide range (1.5–6) of Pirani scores at presentation reflects this. However, a median score of 4.5 also indicates a significant number of more severely deformed feet. With the experience gained, and as our service becomes more established and expands, we hope to solely manage all clubfeet that are referred without the need for involvement of a tertiary referral centre. We do, however, maintain good links for discussion and problem solving with the latter, should the need arise.
The severity of the deformity of our feet was graded according to Pirani’s scoring system, which is based on a six-point scale of clinical signs of contracture relating to the hind and midfoot. The Pirani score has been shown to have a good predictive value with regards to need for tenotomy and number of casts [18, 19]. We found this to be true in our study with the more severely deformed feet requiring a tenotomy and greater number of cast changes.
Of note, our tenotomy rate is significantly lower than that quoted by Ponseti and some other series [7, 8, 20]. This may merely reflect the greater severity of deformity seen in the centre of excellence and tertiary referral centres, whereas in our centre we also had a greater number of mild deformities. Also, our service has only been running for several years, and in the early stages there may have been a natural hesitancy to perform a tenotomy, although we realise the importance of a tenotomy and our greater experience has reinforced the exact application of the Ponseti method. Ponseti performs his tenotomies within the outpatient department, whereas we currently perform ours under a general anaesthetic. Although this setting provides us with a controlled environment and optimises the safety of the procedure, it may delay the tenotomy as it is dependent on the availability of a paediatric anaesthetist. At times, this delay necessitated additional cast changes to “hold” the foot until the tenotomy could be performed. It is likely that this will now become an outpatient procedure performed under local anaesthetic. Also of note is that we required on average approximately 8 cast changes to correct the more severely affected feet. This is slightly higher than the more experienced centres, and reflects not only the natural learning curve of the Ponseti method that would be expected in a service in its early stages, some older patients and delay in performing the tenotomy, but may also have been skewed by the patient with atypical complex feet who had 4 plaster slippages and eventually required referral to a tertiary centre. With time and acquired experience, we expect our mean number of cast changes to lessen.
As discussed, only one of our patients failed local conservative management and required tertiary referral. He had atypical complex feet and required treatment with the modified Ponseti protocol [13]. We only had a small number (5) of complex feet in our series, and thus our experience with this newer protocol is somewhat limited. The complex foot presents as a short, stiff foot with a deep medial crease and is being recognised now as a foot that typically behaves very differently, and this needs to be respected [20]. However, since then, both ESPs and the senior author (C.J.C.) have attended a tertiary referral centre and have spent a week with Professor Ponseti and his team in Iowa, and we are now managing these feet in-house.
Regardless of the method of treatment, CTEV has a tendency to relapse. This most commonly occurs until 2 years of age, although it can occur later [13, 20, 21]. The primary risk factor for recurrence after correction is related to poor or non-compliance with bracing, and these recurrences may require more extensive surgery than Achilles tenotomy and anterior tibial tendon transfer [6, 7]. By providing a personalised closer contact service, we feel better continuity of care, education and empowerment of parents, and therefore compliance, can be ensured. This is particularly important in such a prolonged management protocol. Our results are still early, and later recurrences and relapses may still occur.
With a physiotherapy-led service, the team approach also ensures patient care is less affected by absenteeism (holidays, sickness) providing there is more than one trained ESP. The service reduces the workload of the local consultant, avoids unnecessary overloading of tertiary referral centres and lessens parents’ excess travel and inconvenience. We found consistency of note keeping and recording is also improved. Although the orthopaedic consultant is thus available to see more orthopaedic patients, but there is a risk of becoming de-skilled.
In summary, our early results show that a physiotherapist-led Ponseti service can be successfully transferred to a DGH setting. It is important that the physiotherapists are appropriately trained, accept a learning curve, acknowledge limitations and have supervision by a paediatric orthopaedic consultant. Continued auditing of services provided by non-medical specialists, to ensure safe and effective delivery, is important.
References
- 1.Cummings RJ, Lovell WW. Operative treatment of congenital idiopathic club foot. J Bone Joint Surg Am. 1988;70-A:1108–1112. [PubMed] [Google Scholar]
- 2.Dobbs MB, Nunley R, Schoenecker PL. Long-term follow-up of patients with clubfeet treated with extensive soft-tissue release. J Bone Joint Surg Am. 2006;88-A(5):986–996. doi: 10.2106/JBJS.E.00114. [DOI] [PubMed] [Google Scholar]
- 3.Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am. 2003;85-A:1286–1294. doi: 10.2106/00004623-200307000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Karol LA, O’Brien SE, Wilson H, Johnston CE, Richards BS. Gait analysis in children with severe clubfeet: early results of physiotherapy versus surgical release. J Pediatr Orthop. 2005;25(2):236–240. doi: 10.1097/01.bpo.0000150815.56790.b0. [DOI] [PubMed] [Google Scholar]
- 5.Ponseti IV. Treatment of congenital club foot. J Bone Joint Surg Am. 1992;74-A:448–454. [PubMed] [Google Scholar]
- 6.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Paediatrics. 2004;113(2):376–380. doi: 10.1542/peds.113.2.376. [DOI] [PubMed] [Google Scholar]
- 7.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after the use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86-A:22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop. 2002;22(4):517–521. [PubMed] [Google Scholar]
- 9.Goksan SB, Bursali A, Bilgili F, Sivacioglu S, Ayanoglu S. Ponseti technique for the correction of idiopathic clubfeet presenting up to 1 year of age. A preliminary study in children with untreated or complex deformities. Arch Orthop Trauma Surg. 2006;126(1):15–21. doi: 10.1007/s00402-005-0070-9. [DOI] [PubMed] [Google Scholar]
- 10.Shack N, Eastwood DM. Early results of a physiotherapist-delivered Ponseti service for the management of idiopathic congenital talipes equinovarus foot deformity. J Bone Joint Surg Br. 2006;88-B(8):1085–1089. doi: 10.1302/0301-620X.88B8.17919. [DOI] [PubMed] [Google Scholar]
- 11.Tindall AJ, Steinlechner CW, Lavy CB, Mannion S, Mkandawire N. Results of manipulation of idiopathic club deformity in Malawi by orthopaedic clinical officers using the Ponseti method: a realistic alternative for the developing world? J Pediatr Orthop. 2005;25(5):627–629. doi: 10.1097/01.bpo.0000164876.97949.6b. [DOI] [PubMed] [Google Scholar]
- 12.Pirani S (1999) A reliable method of clinically evaluating a virgin clubfoot evaluation. 21st SIDCOT Congress 1999
- 13.Ponseti IV, Zhivkov M, Davis N, Sinclair M, Dobbs MB, Morcuende JA. Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res. 2006;451:171–176. doi: 10.1097/01.blo.0000224062.39990.48. [DOI] [PubMed] [Google Scholar]
- 14.Pearse EO, Maclean A, Ricketts DM. The extended scope physiotherapist in orthopaedic out-patients: an audit. Ann R Coll Engl. 2006;88:653–655. doi: 10.1308/003588406X149183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hockin J, Bannister G. The extended role of a physiotherapist in an out-patient orthopaedic clinic. Physiotherapy. 1994;80:281–284. doi: 10.1016/S0031-9406(10)61050-4. [DOI] [Google Scholar]
- 16.Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital clubfoot. J Bone Joint Surg Am. 1980;62-A:23–31. [PubMed] [Google Scholar]
- 17.Cooper DM, Dietz FR. Treatment of idiopathic clubfoot a thirty-year follow-up note. J Bone Joint Surg Am. 1995;77-A:1477–1489. doi: 10.2106/00004623-199510000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Dyer PJ, Davis N. The role of the Pirani scoring system in the management of club foot by the Ponseti technique. J Bone Joint Surg Br. 2006;88-B(8):1082–1084. doi: 10.1302/0301-620X.88B8.17482. [DOI] [PubMed] [Google Scholar]
- 19.Scher DM, Feldman DS, van Bosse HJ, Sala DA, Lehman WB. Predicting the need for tenotomy in the Ponseti method for correction of clubfeet. J Pediatr Surg. 2004;24(4):349–352. doi: 10.1097/00004694-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Ponseti IV, Smoley EN. Congenital clubfoot: the results of treatment. J Bone Joint Surg Am. 1963;45-A:261–275. [Google Scholar]
- 21.Dobbs MB, Corley CL, Morcuende JA, Ponseti IV. Late recurrence of clubfoot deformity: a 45-year followup. Clin Orthop Relat Res. 2003;411:188–192. doi: 10.1097/01.blo.0000065837.77325.19. [DOI] [PubMed] [Google Scholar]


