Abstract
Purpose
Many surgical techniques have been published on how to treat congenital pseudoarthrosis of the tibia (CPT). We combined Ilizarov’s fixator with intramedullary nailing of the tibia and developed a procedure which combines the advantages of both methods: Ilizarov’s high fusion rate with alignment control and the protection against refracture provided by the intramedullary nail. The results of this approach are presented and discussed.
Material and methods
Seven boys and three girls aged 3–14 years (mean age 8 years 2 months) were treated using our combined technique. In six cases, the CPT was associated with neurofibromatosis. Two strategies were adopted: in six cases, a compression was applied on the bone defect, and in four cases, segmental bone transportation was performed before the compression procedure. The final follow-up (1.2–6.6 years) included a clinical and radiological examination.
Results
Tibial union was achieved in nine cases without bone grafting. In one case, tibial union still remains uncertain, despite intertibiofibular bone grafting and additional compression procedures. Thirteen overall complications were noted, including three valgus deformity of the ankle. Bone transportation failed to achieve complete limb lengthening in three cases. One deep infection occurred 4 years after removal of the external fixator. The treatment for this included nail removal and antibiotic therapy for 3 months. Despite a permanent protection of orthosis, a refracture occurred 2 years after nail removal, reverting to the initial level of pseudarthrosis. Another surgical attempt using the same method was then performed with a satisfactory result.
Conclusions
The association of Ilizarov’s technique and intramedullary nailing achieved and maintained tibial union in nine of ten patients at final follow-up. It also allowed correction of axial deformities and prevented refracture. Despite the short duration of the follow-up and a high rate of complications in our series, this method can be useful in many cases of CPT in which healing has failed to occur despite many previous surgeries.
Keywords: Congenital pseudoarthrosis of the tibia, Ilizarov technique, Intramedullary nailing
Introduction
The surgical treatment of congenital pseudoarthrosis of the tibia (CPT) remains a challenge for the orthopedic surgeon. Many surgical techniques have been published in the literature [1–13], with most aiming at salvaging the limb using conventional techniques of bone grafting and internal fixation. Unfortunately, when multiple procedures fail to achieve union, amputation may be the consequence [6]. Treatment goals of achieving and maintaining union with joint alignment and symmetrical limb length may be compromised by refracture, residual deformity, limb length discrepancy or valgus deformity of the ankle [14, 15]. For the last three decades electromagnetic or low-intensity pulsed ultrasound stimulation of the non-union, vascularized bone grafts, intramedullary nails and Ilizarov’s fixator have all been used with variable degrees of success [6]. Most recently, osteogenic proteins were used to stimulate bone growth after all other treatments had failed [13]. Among these procedures, the Ilizarov technique has a high rate of fusion, allowing for the correction of axial malalignment and leg shortening at the same time [1–5]. The drawback of this technique is its lack of protection against refractures after removal of the fixator [14]. To address this issue, we have developed an original surgical technique that combines Ilizarov’s fixator with intramedullary nailing of the tibia. Our objective was to combine the advantages of both procedures: Ilizarov’s high fusion rate with alignment control and the protection against refracture provided by the intramedullary nail.
The purpose of the retrospective study reported here was to evaluate the clinical and radiological results of this technique for the treatment of CPT.
Material and methods
Population data
Between 1996 and 2005, six girls and three boys aged 3–14 years (mean age 8 years 2 months) were treated in our department for CPT with the combination of Ilizarov’s technique and intramedullary nailing. In six cases, the CPT was associated with neurofibromatosis. The CPT was unilateral in eight cases and bilateral in one case. According to Crawford’s classification [16], all patients were type IV. There were four pseudarthrosis of the tibia associated with a pathological fibular bowing, and six pseudarthrosis of the tibia and fibula. The non-union was always located on the distal third of the leg. According to Apoil’s classification [17], four pseudarthrosis were atrophic (type I), and six were hypertrophic or normotrophic (type II). Five cases of pseudarthrosis were associated with axial deviations, one was associated with isolated limb length discrepancy (LLD) and four were associated with both deformities. The initial LLD was measured after intraoperative reaxation using the Ilizarov apparatus. All patients underwent various surgical procedures before the Ilizarov’s technique with tibial nailing (Table 1), but none of these previous treatments achieved tibial union. The demographic data on the patient cohort are summarized in Table 2.
Table 1.
Previous surgical procedures
| Surgical procedure | Number of cases |
|---|---|
| Ilizarov technique | 4 |
| Intertibiofibular bone graft | 3 |
| Intramedullary rodding and osteotomy | 2 |
| Elastic intramedullary nailing | 3 |
| Cortical bone graft and external fixator | 3 |
| Periosteal flap | 1 |
| Vascularized fibular graft and external fixator | 1 |
| Treatment of tibial osteomyelitis | 1 |
Table 2.
Demographic data of the patient series
| Case | Gender | Side | Neuro- fibromatosis | Type (Apoil) | LLD (cm) | Age at treatment (years + months) | Ilizarov strategy | Intramedullary rodding | Duration of Ilizarov (months) | Secondary bone grafting |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | L | Yes | II | No | 14 + 8 | Compression | Antegrade | 13 | Yes |
| 2 | F | R | Yes | I | 2 | 3 + 7 | Transport | Telescopic | 9 | Yes |
| 3 | M | L | Yes | I | No | 7 + 6 | Transport | Transplantar | 7 | Yes |
| 4 | F | R | Yes | II | No | 4 + 8 | Compression | Antegrade | 4 | Yes |
| L | 4 | 4 + 9 | Transport | Telescopic | 9 | Yes | ||||
| 5 | F | R | Yes | II | No | 3 + 10 | Compression | Telescopic | 5 | Yes |
| 6 | F | R | No | II | 5 | 11 + 9 | Compression | Antegrade | 6 | No |
| 7 | F | R | Yes | I | 6 | 9 + 10 | Transport | Antegrade | 12 | Yes |
| 8 | M | L | No | I | 10 | 10 + 10 | Transport | Transplantar/Telescopic | 11 | No |
| 9 | M | L | No | II | No | 8 + 9 | Compression | Antegrade | 7 | No |
LLD, Limb length discrepancy; F, female; M, male; L, left; R, right
Surgical procedure
All surgeries were performed by one single surgeon (JPD). First, excision of the fibrous tissue at the pseudarthrosis site was performed to allow alignment of the two bone segments. This was followed by the intramedullary nailing. Four telescopic nails (no. 20; Medicalex, Bagneux, France), four titanium elastic nails (TEN; Synthes, Paoli, PA) and two large Kirschner wires were used. Telescopic nails were implanted in the proximal and distal epiphyses and were mainly used in cases of LLD associated with ankle stiffness because a surgical approach of the ankle joint was necessary to insert the distal part of the nail. An antegrade nailing was performed in eight patients to preserve the ankle joint. After nailing, the Ilizarov’s fixator was installed with two whole rings above the non-union site and one below. A transplantar nailing was used in two patients because of a short distal tibial segment less than 3 cm in length. In these cases, a calcaneal half-ring was added to increase distal stability (Fig. 1c). At the end of the lengthening procedure, the transplantar nail was removed.
Fig. 1.

Schematic representation of the two therapeutic strategies. a Dynamic compression and rodding, b dynamic bone transportation and compression, c illustrations of the first strategy (dynamic distal compression) combined with calcaneal fixation
Two different strategies were used for applying the Ilizarov’s technique. In five cases, a simple compression was applied on the bone defect (Figs. 1a, 2). In the five remaining cases, because the resection of the dystrophic part of the bone was responsible for tibial shortening, segmental bone transportation was performed before the compression procedure to avoid a LLD (Figs. 1b, 3).
Fig. 2.
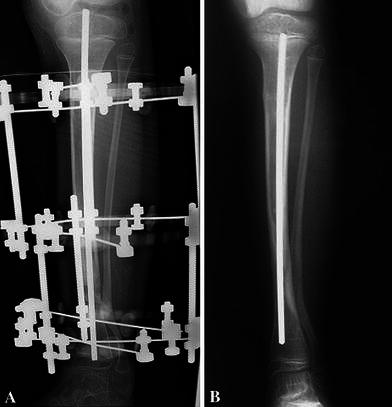
Initial (a) and final (b) frontal radiographs of a dynamic compression procedure in patient 5
Fig. 3.

Preoperative frontal (a) and lateral (b) radiographs in a patient aged 2 years. Initial (c) and final (d) frontal radiographs of a dynamic bone transportation combined with compression procedure in patient 7. The telescopic nail lengthening was obtained first by the Ilizarov apparatus and, after the transportation–compression treatment, by the physiological growth of the tibia
All patients were referred to a rehabilitation center during the correction phase. Distraction speed for bone transportation procedures was 1 mm/day. Once the transported segment had bridged the gap, end-to-end compression was applied. In seven patients with fibular non-union, an intertibiofibular bone graft was performed with autologous bone from the iliac crest. After bone union was achieved, the Ilizarov’s fixator was removed, and a short leg cast was applied for 3–4 months; this was followed by a protective short leg orthosis until skeletal maturity.
At the final follow-up, (mean 4 years, range 1.2–6.6 years), ten patients were reviewed for clinical and radiological examination. Joint stiffness and LLD were evaluated. The anteroposterior and lateral radiographs were performed to assess frontal and sagittal deformities as well as degenerative changes of the ankle and LLD.
Results
Pseudarthrosis treatment
Tibial union was achieved in nine cases without bone grafting. The duration of the Ilizarov treatment was an average of 8.3 months (range 4–13 months). Fibular union was achieved in only five cases, despite seven intertibiofibular bone grafts performed after removal of the Ilizarov’s fixator. One patient needed two bone graftings at the seventh and fortieth postoperative month. In one case (patient 1) tibial union could not be obtained, despite an intertibiofibular bone grafting and a long treatment with the Ilizarov’s device (13 months). A reoperation was needed because of failure of the nail at 2 years after removal of the Ilizarov’s device (Fig. 4). After a new intramedullary nailing and compression with the Ilizarov’s fixator, the tibial union still remains uncertain (Fig. 5). Among the nine patients for whom tibial union was achieved, two residual anterior bowings and three frontal misalignments of the tibia were noted (Table 3). Three patients developed a valgus deformity of the ankle due to a persistent pseudarthrosis of the fibula (two cases) and a delayed union that required two successive bone grafts (one case). In patient 3, a 13-year-old boy, a corrective supramalleolar tibial osteotomy was performed for a 40° ankle valgus with a favourable outcome at final follow-up (Fig. 6). Five patients had initial LLD after axial correction. After bone transportation, the LLD was corrected in two cases but persisted in three (Table 3). One patient (patient 3) with no limb length discrepancy at the initial phase was diagnosed with a 3-cm shortening of the leg at final follow-up.
Fig. 4.

Four-millimeter diameter titanium nail failure combined with tibial non-union in patient 1
Fig. 5.

After a new intramedullary nailing, and compression with Ilizarov’s fixator, the tibial union still remains uncertain in patient 1
Table 3.
Patient data at final follow-up
| Case | Follow-up interval (years) | Age at follow-up (years + months) | Tibia union | Fibula union | Refracture | Tibial deformities (degrees) | Ankle valgus (degrees) | LLD (cm) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Varus | Valgus | Flexum | ||||||||
| 1 | 2.7 | 17 + 5 | No | No | – | – | – | – | – | No |
| 2 | 4.3 | 7 + 11 | Yes | Yes | No | No | No | No | No | No |
| 3 | 6.2 | 13 + 11 | Yes | No | No | No | 25 | 30 | 40 | 3 |
| 4 | 5.6 | 10 + 3 | Yes | No | No | No | 2 | 12 | 5 | No |
| 5.5 | 10 + 3 | Yes | Yes | No | No | No | 10 | No | 4 | |
| 5 | 6.6 | 10 + 3 | Yes | Yes | Yes | – | – | – | – | No |
| 6 | 4.3 | 16 + 2 | Yes | No | No | No | No | No | 12 | 2 |
| 7 | 1.8 | 11 + 8 | Yes | Yes | No | 14 | No | No | No | 4 |
| 8 | 1.2 | 12 + 1 | Yes | No | No | No | No | No | No | No |
| 9 | 1.5 | 10 + 4 | Yes | Yes | No | No | No | No | No | No |
Fig. 6.

Frontal (a) and lateral (b) initial radiographs in a patient at the age of 3 years. c Result of a compression procedure around a 4-mm titanium nail inserted down to the ankle to avoid distal misalignment of the tibia in a 6-year-old child (Patient 3). d The same patient at the age of 13 years. Note the proximal nail migration due to the growth of the tibia, which is responsible for a distal tibial deformity. e Final result after corrective supramalleolar tibial osteotomy for a 40° ankle valgus
Function
At final follow-up, the nine patients with achieved tibial union could walk with full weight bearing on the treated limb. although four still had permanent protection orthosis. The two patients treated by transplantar nailing presented ankle stiffness with degenerative changes of the ankle joint on the X-rays, although only one of them complained about ankle pain. None of the patients with axial deformity of the ankle complained about instability. Knee function was normal in eight cases. Two patients presented a knee flexion contracture of 5° and 20°, respectively, after antegrade nailing.
Complications
Thirteen overall complications (including frontal deformities and lower limb shortage) were noted (Table 4). There were no intraoperative complications, such as neurovascular damage or compartment syndrome. Three secondary complications occurred within 1 year. A superficial infection occurred 3 months after removal of Ilizarov’s apparatus and was successfully treated by local care. In another patient, a traumatic fracture of the distal femur occurred. The fracture was treated with a pelvi-femoral plaster cast connected to the external fixator for 6 weeks. One deep infection occurred in another patient (patient 6) 4 years after removal of the external fixator. The treatment included nail removal and antibiotic therapy for 3 months. Despite a permanent protection orthosis, a refracture occurred 2 years after the nail removal, reverting to the initial level of pseudarthrosis. Recently, this patient was re-operated on with the same procedure with a final satisfactory outcome. In another case, the Kirschner wire came out across the knee during the bone transportation procedure.
Table 4.
Complications
| Complications | Number of cases |
|---|---|
| Neurovascular damage | 0 |
| Superficial infection | 1 |
| Intramedullary abscess | 1 |
| Iterative exit of the rod | 1 |
| Stress fracture of the rod | 1 |
| Refracture | 1 |
| Fracture of the distal femur | 1 |
| LLD ≥2 cm | 4 |
| Ankle valgus | 3 |
| Amputation | 0 |
Discussion
The treatment of CPT remains a surgical challenge. Since the condition is fairly rare, with a prevalence rate of 1 in 140,000–250,000 individuals [18, 19], the published series are small and heterogeneous. Despite the numerous surgical techniques described in the literature, clinical outcomes remain uncertain with a high rate of refracture. Furthermore, many surgical procedures are focused on achieving union without any consideration being given to potential residual deformities.
Ilizarov first described his technique to treat CPT in 1971 [1]. It soon became very popular, and many other authors published their experience with this technique in the years following the publication [2–5]. According to the multicentre study of the European Paediatric Orthopaedic Society (EPOS), the Ilizarov technique has become the gold standard in the treatment of CPT [6]. Its review of the 120 published CPT cases using the Ilizarov technique showed satisfactory results with pseudarthrosis healing in 94 patients [6]. However, Kristiansen [14] emphasized the high complication rate, including residual axial deformities and refracture.
This drawback of the Ilizarov technique is the reason why we devised our modified method combining intramedullary nailing and the Ilizarov fixator. Our goals were to improve the control of frontal and sagittal alignment and provide protection against refracture [6, 7].
Our results in achieving and maintaining tibial union are comparable with other series using ilizarov’s technique. Ilizarov and Gracheva achieved bone union in all of their 16 cases without any grafting [1], but five refractures occurred because of residual axial deviation or bowing of the tibia. In a multicenter retrospective study, Paley [2] reports tibial union in 15 of 16 cases, with five cases of refracture. Ghanem [4] successfully treated ten of 14 patients with Ilizarov’s technique. Three out of these ten patients achieved bone union after a second grafting procedure, and one patient presented a refracture. In a long-term follow-up study on 87 patients treated with the Ilizarov technique, Gracheva [8] states that a better prognosis can be expected for tight and hypomobile CPT. Ghanem [4] also noted that the best indications for Ilizarov’s technique were the normotrophic and hypertrophic types (Apoil II). He suggested that resection of the pseudarthrosis site should improve the results, especially for atrophic (Apoil I) pseudarthrosis.
Refracture can be explained by the persistent malalignment of the tibia and fibula that results in an enhanced stress on a dystrophic bone after healing of the pseudarthrosis. In our study, four patients had a diaphyseal malalignment, but only one had refracture on dystrophic bone after removal of the tibial nail. We believe that the prevention of refracture is based on three principles: (1) the correction of diaphyseal angular deformities that can be obtained by Ilizarov’s fixator combined with a nail; (2) the achievement of fibular union, using tibio-fibular grafting if necessary; (3) the permanent protection of the dystrophic tibia by the intramedullary nail and external orthesis. Indeed, we agree with Apoil [17] that the tibia remains fragile, “united but not solid”, until the end of growth.
Persistent pseudarthrosis of the fibula is known to cause ankle valgus deformity and functional impairment [9, 15]. This condition is due to a high position of the fibular distal epiphysis and because of an asymmetric growth of the distal tibial physis that grows more medially than laterally [2, 10]. In our study, five patients had a persistent pseudarthrosis of the fibula, but only three of these developed ankle valgus. These results are comparable to those of Inan [15] who noted seven cases of persistent fibular pseudarthrosis, with six ankle valgus, among 16 patients treated by intramedullary nailing, bone grafting and various subsequent procedures. Reestablishment of the integrity of the fibula decreases the load passing through the tibia and provides rotatory stress protection [2]. Fibular healing can be achieved by massive bone grafting, leading to a distal tibio-fibular synostosis according to Langenskiöld [11]. The Ilizarov’s method also allows a distal transportation of the lateral malleolus that has been used successfully by Gracheva [8] in 40 congenital pseudarthrosis.
Functional results not only depend on the integrity of the tibia for full weight bearing but also on the limb’s length and alignment. Joseph showed that the longer the pseudarthrosis remains un-united, the greater is the shortening of the tibia [7]. Limb length discrepancies have a variable evolution and may become worse, despite treatment [12]. In our patient series, initial LLD was fully corrected in one patient, partially corrected in two and remained unchanged in one. No pseudarthrosis was observed at the lengthening site, as described by Inan [15].
Transplantar nailing, used twice in the current series for short distal tibial segments, was responsible for stiffness and degenerative changes in the ankle joint. This kind of procedure should be avoided when possible. In the EPOS study, only 17% of the patients who had transcalcaneal nailing kept a normal ankle joint function [6].
Pin-tract infections are well-recognized complications of the Ilizarov technique [5]. The major potential risk of combining this technique with intramedullary nailing is infection caused by the nail. Only one case of such a complication was observed in our series. In our experience, as in osteogenesis imperfecta patients, transphyseal nailing was not responsible for growth disturbances. No growth disturbance was noted at follow-up in our small cohort of patients. However, we recognize that six patients were considered to be being immature at follow-up and that a careful screening of physeal growth is mandatory.
In conclusion, our combined surgical approach consisting of both Ilizarov’s technique and intramedullary nailing achieved and maintained tibial union in nine of our ten patients at final follow-up. It also allowed correction of axial deformities and prevented refracture. However, we fully recognize that the relatively short duration of the follow-up is a weak point of our series and that the risks of progressive limb deformities or mechanical problems need to be taken into account in the non-mature patients of the cohort. This method can be useful in many cases of CPT in which healing has failed to occur despite many previous surgeries. However, the external apparatus is sometimes not well tolerated by the patient, and complications, such as ankle valgus, adjacent joints stiffness or infection, may occur.
References
- 1.Ilizarov GA, Gracheva VI. Bloodless treatment of congenital pseudarthrosis of the crus with simultaneous elimination of shortening using dosed distraction. Ortop Travmatol Protez. 1971;32:42–46. [PubMed] [Google Scholar]
- 2.Paley D, Catagni M, Argnani F, et al. Treatment of congenital pseudoarthrosis of the tibia using the Ilizarov technique. Clin Orthop Relat Res. 1992;280:81–93. [PubMed] [Google Scholar]
- 3.Plawecki S, Carpentier E, Lascombes P, Prevot J, Robb JE (1990) Treatment of congenital pseudarthrosis of the tibia by the Ilizarov method. J Pediatr Orthop 10:786–790 [DOI] [PubMed]
- 4.Ghanem I, Damsin JP, Carlioz H. Ilizarov technique in the treatment of congenital pseudarthrosis of the tibia. J Pediatr Orthop. 1997;17:685–690. doi: 10.1097/01241398-199709000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Damsin JP, Ghanem I, Carlioz H. Contribution of Ilizarov’s equipment in the treatment of congenital pseudarthrosis of the lower limb. Rev Chir Orthop Reparatrice Appar Mot. 1996;82:34–41. [PubMed] [Google Scholar]
- 6.Grill F, Bollini G, Dungl P, Fixsen J, Hefti F, Ippolito E et al (2000) Treatment approaches for congenital pseudarthrosis of tibia: results of the EPOS multicenter study. European Paediatric Orthopaedic Society (EPOS). J Pediatr Orthop B 9:75–89 [DOI] [PubMed]
- 7.Joseph B, Mathew G. Management of congenital pseudarthrosis of the tibia by excision of the pseudarthrosis, onlay grafting, and intramedullary nailing. J Pediatr Orthop B. 2000;9:16–23. doi: 10.1097/01202412-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Gracheva VI, Makushin VD, Shevtsov VI, Kuftyrev LM, Degtiarev VE. Ilizarov’s transosseous osteosynthesis in treating congenital pseudoarthroses of the leg. Ortop Travmatol Protez. 1981;7:34–38. [PubMed] [Google Scholar]
- 9.Johnston CE., 2nd Congenital pseudarthrosis of the tibia: results of technical variations in the Charnley–Williams procedure. J Bone Joint Surg Am. 2002;84-A:1799–1810. [PubMed] [Google Scholar]
- 10.Grill F. Treatment of congenital pseudarthrosis of tibia with the circular frame technique. J Pediatr Orthop B. 1996;5:6–16. doi: 10.1097/01202412-199605010-00002. [DOI] [PubMed] [Google Scholar]
- 11.Langenskiold A. Pseudarthrosis of the fibula and progressive valgus deformity of the ankle in children: treatment by fusion of the distal tibial and fibular metaphyses. Review of three cases. J Bone Joint Surg Am. 1967;49:463–470. [PubMed] [Google Scholar]
- 12.Bitan F, Rigault P, Padovani JP, et al. Congenital pseudarthrosis of the tibia and fibula in children. Results of the treatment of 18 cases with nails and bone grafts. Rev Chir Orthop Reparatrice Appar Mot. 1987;73:552–560. [PubMed] [Google Scholar]
- 13.Lee FY, Sinicropi SM, Lee FS, Vitale MG, Roye DP, Choi IH. Treatment of congenital pseudarthrosis of the tibia with recombinant human bone morphogenetic protein-7 (rhBMP-7). A report of five cases. J Bone Joint Surg Am. 2006;88:627–633. doi: 10.2106/JBJS.D.02201. [DOI] [PubMed] [Google Scholar]
- 14.Kristiansen LP, Steen H, Terjesen T. Residual challenges after healing of congenital pseudarthrosis in the tibia. Clin Orthop Relat Res. 2003;414:228–237. doi: 10.1097/01.blo.0000076800.53006.c9. [DOI] [PubMed] [Google Scholar]
- 15.Inan M, El Rassi G, Riddle EC, Kumar SJ (2006) Residual deformities following successful initial bone union in congenital pseudoarthrosis of the tibia. J Pediatr Orthop 26:393–399. doi:10.1097/01.bpo.0000187999.68966.58 [DOI] [PubMed]
- 16.Crawford AH. Neurofibromatosis in the pediatric patient. Orthop Clin North Am. 1978;9:11–23. [PubMed] [Google Scholar]
- 17.Apoil A. Congenital pseudarthrosis of the leg. 13 cases. Rev Chir Orthop Reparatrice Appar Mot. 1970;56:120–138. [PubMed] [Google Scholar]
- 18.Paterson D. Congenital pseudarthrosis of the tibia. An overview. Clin Orthop Relat Res. 1989;247:44–54. [PubMed] [Google Scholar]
- 19.Andersen KS. Radiological classification of congenital pseudarthrosis of the tibia. Acta Orthop Scand. 1973;44:719–727. doi: 10.3109/17453677308989112. [DOI] [PubMed] [Google Scholar]


