Abstract
Background
Tibial tuberosity fractures in adolescents are uncommon. We retrospectively reviewed all tibial tuberosity fractures in adolescents (10–19) who presented to our level 1 pediatric trauma center over a 7-year period to review fracture morphology, mechanism of injury, fracture management including return to play, as well as complications. Additionally, we present a review of the literature and treatment algorithm.
Methods
We reviewed the clinical charts and radiographs of consecutive patients with tibial tuberosity fractures between 01 January 2000 and 01 January 2007. Data parameters included the following: patients age and gender, involved side, injury classification, co-morbidities, mechanism of injury, treatment, return to activity and complications. Data were extracted and reviewed, and a treatment algorithm is proposed with some additional insights into the epidemiology of the injury. Nineteen patients met the inclusion criteria.
Results
There were 19 patients with 20 tibial tuberosity fractures. The mean age was 13.7 years. There were 18 males and 1 female patient. There were nine left-sided injuries and eleven right-sided including one patient with bilateral fractures. Mechanism of injuries included basketball injury (8), running injury (5), football injury (3), fall from a scooter (2), high jump (1) and fall (1). Co-morbidities included three patients with concurrent Osgood–Schlatter disease and one with osteogenesis imperfecta. All were treated with ORIF, including arthroscopic-assisted techniques in two cases. Complications included four patients with pre-operative presentation of compartment syndrome all requiring fasciotomy, one post-operative stiffness and one painful hardware requiring removal. Range of motion was started an average of 4.3 weeks post-operatively and return to play was an average of 3.9 months post-operatively.
Conclusion
Although uncommon, tibial tuberosity fractures in adolescents are clinically important injuries. Early recognition and treatment (closed or open as appropriate) gives good results. All the patients in our series had surgical fixation as per different indications that have been elaborated. It is important for clinicians to recognize that compartment syndrome remains a significant concern post-injury and in the perioperative period. Close monitoring and timely intervention is recommended. A simple treatment algorithm is presented for clinicians to help manage these injuries.
Keywords: Tibial tuberosity, Avulsions, Fractures, Complications, Management
Introduction
Avulsion fracture of the tibial tubercle is a relatively uncommon injury, with a reported incidence ranging from 0.4% to 2.7%, usually seen in adolescent males approaching skeletal maturity [1–7] with well developed quadriceps musculature. Typically, these fractures present with marked displacement of the entire proximal apophysis, with or without intra-articular extension, and variable associated soft tissue injury. The majority of these injuries are incurred during athletic activity involving jumping, most commonly basketball, and are the result of one of two possible mechanisms of injury [1, 3, 5, 7–10]: (1) violent knee flexion against a tightly contracting quadriceps, as in landing from a jump [11] or (2) violent quadriceps contraction against a fixed foot, as in jumping [12].
Classification of tibial tubercle fractures has gone through an evolution. The original classification system was provided by Sir Reginald Watson-Jones which defined three types. Type I was an avulsion of a small part of the tibial tubercle, distal to the proximal tibial physis. Type II extended across the physis but did not enter the knee joint. Type III was an avulsion which extended proximal to the physis into the knee [11]. This classification was modified by Ogden et al. to more accurately define specific fracture patterns and to establish treatment for different fracture types by including displacement and comminution [7]. Ryu and Debenham then suggested the addition of a Type IV which is a fracture of the tibial tuberosity that extends posteriorly along the proximal tibial physis creating an avulsion of the entire proximal epiphysis [13]. Next, the addition of a type C was proposed by Frankl et al. for fractures with associated patella ligament avulsions [14]. Finally, a Type V was suggested by McKoy and Stanitski [9], also described by Curtis [15], which consists of a Type IIIB fracture with an associated Type IV fracture creating a ‘Y’ configuration.
We retrospectively reviewed all the tibial tuberosity fractures in adolescents (10–19 years) that were managed in our tertiary level 1 pediatric trauma center. Our study includes 19 adolescents with 20 tibial tuberosity fractures, the largest single series to date, and attempts to review fracture morphology, mechanism of injury, management including return to play and complications. We offer epidemiological insight to this injury and propose a treatment algorithm based on our experience with these injuries.
Methods
After IRB approval, we retrospectively reviewed all tibial tuberosity fractures in adolescents registered in the trauma database at our tertiary care level 1 pediatric trauma center. All fractures treated between January 2000 and January 2007, with a minimum of 12-month post-treatment follow-up were identified. Clinical records and radiographs were reviewed. Data parameters included: patient age and gender, involved side, injury classification (modified Ogden), co-morbidities, mechanism of injury, treatment, return to activity and complications. Data were extracted, compiled and is presented.
Results
There were 19 patients with 20 tibial tuberosity fractures. Mean age at the time of injury was 13.7 years (range 11 years 5 months–17 years 6 months). Mean follow-up period was 24 months. There were 18 males and 1 female patient. There were nine left-sided injuries and eleven right-sided, including one patient with bilateral fractures. Mechanism of injuries included: basketball injury (8), running injury (5), football injury (3), fall from a scooter (2), high jump injury (1) and fall (1). One patient had a co-morbidity of osteogenesis imperfecta (Type I), while three had concurrent symptomatic Osgood–Schlatter disease.
Using the modified Ogden classification, we found two Type IB fractures, one Type IC, three Type IIA, three Type IIB, five Type IIIA, five Type IIIB and one Type IV. There were no Type IA or Type V fractures. All but one of the patients had a surgical intervention using cannulated screws, with or without washers. One had supplemental suture anchors and one was fixed solely with tension band wiring using heavy suture material (No. 5 Ethibond). Arthroscopic-assisted technique was used in two of the type III cases, rather than open arthrotomy, to assess the adequacy of articular cartilage restoration, as per surgeon preference (Fig. 1).
Fig. 1.
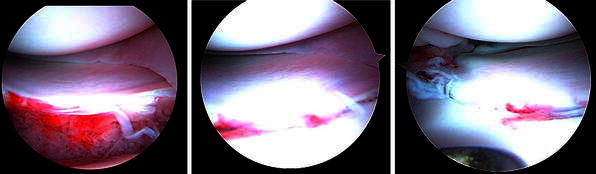
Arthroscopic images demonstrate ability to judge joint restoration, meniscal movement and assess joint cartilage
Four of these patients (4/20:20%) had clinical symptoms of compartment syndrome pre-operatively and underwent fasciotomy during fixation. Post-operative complications included one patient with stiffness that eventually required an adhesiolysis and another patient with tendonitis requiring a removal of hardware that led to eventual resolution of symptoms. Range of motion was started at average of 4.3 weeks post-operatively (3.4–6.3 weeks) and return to play occurred at an average of 3.9 months post-operatively (2.5–6.5 months). None of these patients exhibited symptoms of missed compartment syndromes including muscle atrophy, contractures or nerve damage. None of the patients had any evidence of growth disturbance of the proximal tibia or recurvatum at final follow-up.
Discussion
The tibial tuberosity develops from a secondary ossification center in the proximal aspect of the tibia. In contrast to the proximal tibial epiphysis, which develops in compression, the tibial tuberosity is an apophysis and develops in traction [16]. Development of the tubercle has been divided into four stages: cartilaginous, apophyseal, epiphyseal, and bony [17]. Closure of the proximal tibial epiphysis, which extends distally toward the tubercle apophysis, may leave a mechanically vulnerable period which predisposes the tuberosity to avulsion injury [9]. This is also likely the reason genu recurvatum is not commonly associated with this injury, although possible, especially in the pre-adolescent patient population (9–12 years old).
Blount [18] proposed genu recurvatum as a potential complication of tibial tuberosity fracture; however, reports of this complication exist only as a single case report. Thus, genu recurvatum is usually not considered a complication often associated with this fracture due to the time in which the fracture occurs relative to physiologic physiodesis [2, 4, 7, 19]. However, leg length discrepancy and/or genu recurvatum would most likely be associated with young physiologic age or improper surgical technique. Evidence-based criteria defining physiologic age and/or tanner staging, for which leg length discrepancy or genu recurvatum are at increased risk, are yet to be determined. Fortunately, we have no complications of leg length discrepancy or genu recurvatum to report despite treating four pre-adolescent patients with surgical fixation. Although no definitive conclusion can be drawn from this, perhaps careful surgical technique, and care to avoid crossing the physis helped prevent these complications.
The age range for the mechanically vulnerable period in males is approximately 13–16 years. Five of our 19 patients (26%) fell outside of this range with two 11 years old, two 12 years old, and one 17 years old. There have been 11 previous reports of pre-adolescents with this injury (ages 9–12 years) [2, 3, 6, 7, 14, 20].
There is a strong predominance towards males with this injury. This is believed to be a result of a greater number of males participating in athletics, as well as, the later age in which males experience physiologic physiodesis of the proximal tibia [9]. Because males experience physiodesis at a later age, they are larger and heavier, and their quadriceps are stronger. Consequently, the tibial tubercle is likely subject to higher traction stresses. There have been nine tibial tuberosity avulsion fractures in females previously reported in the literature [1, 3, 6, 8, 10, 21]. Of our 19 patients, one was female and coincidentally, she was also our youngest patient (11 years 5 months).
There has been a preponderance of left-sided injuries in the literature. In five studies, which included sidedness, 49 of 70 (70%) injuries were left-sided [2, 3, 6, 10, 12]. Bolesta and Fitch postulated that this may be a result of individuals leading with the left extremity [2]. In our series there were eight left- and ten right-sided injuries and we did not find any specific correlation with the sidedness. We also had one bilateral injury. There are 13 previous reports of bilateral injuries in the literature [19, 22–25]. There has not been a definitive correlation between Osgood–Schlatter disease and tibial tuberosity fractures, as suggested by Ogden and Southwick [16]. However, Osgood–Schlatter disease has been reported as an associated finding with tibial tubercle fractures in nearly every study. Vichard et al. recommend restricting athletics in all boys with severe Osgood–Schlatter disease until approximately age 14 years old [1, 10]. Our results revealed 3 of 19 (15.7%) patients with pre-existing symptomatic Osgood–Schlatter disease (Fig. 2a–d). Complications with tibial tubercle fractures are relatively uncommon; however, compartment syndrome is a potentially severe complication which must be considered upon initial presentation of injury. In his paper on the Hauser procedure from 1979, Wall described a fan shaped group of vessels originating from the anterior tibial recurrent artery, on the lateral aspect of the tibial tubercle which retract under the fascia when sectioned [26]. Compartment syndrome has since been reported in five patients in three series of tibial tuberosity fractures [27–29]. Our results had four patients requiring fasciotomy; two for active compartment syndrome (anterior compartment pressures of 55 and 62 mmHg) and two for impending compartment syndromes as determined by associated clinical symptoms. Although we would not recommend prophylactic fasciotomies, we recommend careful consideration of compartment syndrome as a possible complication of tibial tubercle fractures and therefore recommend a high level of vigilance and close monitoring in the perioperative period. This may also be a select group of patients where regional anesthesia/ blocks may be avoided during surgery to facilitate close observation and detailed evaluation.
Fig. 2.

a Plain radiograph AP view of a 14-year-old with type IIIB tibial tuberosity fracture. b Lateral radiograph of the same patient demonstrating a fragment comminution. c Six-month post-op AP radiograph of the same patient demonstrating fixation. d Lateral radiograph demonstrating union with good remodeling
The goal of treatment for fractures of the tibial tubercle is to restore the extensor mechanism and the joint surface, when disrupted. Closed treatment generally entails closed reduction and immobilization in a long leg or cylinder cast for approximately 4 weeks or until evidence of union is apparent on radiographs. Open reduction with internal fixation which involves fixation with screws, washers, tension band wiring [28] or suture repair of periosteum, as necessary, followed by casting for 3–4 weeks. Arthroscopic-assisted open fixation is also gaining popularity among some surgeons. We have had some experience in treating these cases with arthroscopic-assisted techniques (Fig. 1). The technique is helpful in fractures, such as type III variants that have intraarticular extension to evaluate for joint line/articular cartilage restoration and to also assess for any associated meniscal or osteochondral injuries. Arthroscopic assisted techniques additionally help to reduce the size of the skin incision and need for a large arthrotomy.
Surgeon comfort with the fixation technique mostly drives the nature of fixation and at this point literature does not recommend any evidence-based preference for a certain technique over the others. Care must be taken to avoid creating patella infera, to avoid crossing any physis in the physiologically less mature patient, to remove periosteum from the fracture bed which could interfere with reduction and healing, and to address any co-morbidities such as patella ligament avulsion, compartment syndrome or meniscal injury. ROM is initiated at approximately the fourth week followed by resistance training at approximately 6 weeks. Return to play can be expected approximately 2–3 months after injury in Type I and II injuries. For Type III–V injuries return to play can be expected 3–6 months after injury. Our proposed algorithm and approach to these patients is presented in Fig. 3.
Fig. 3.
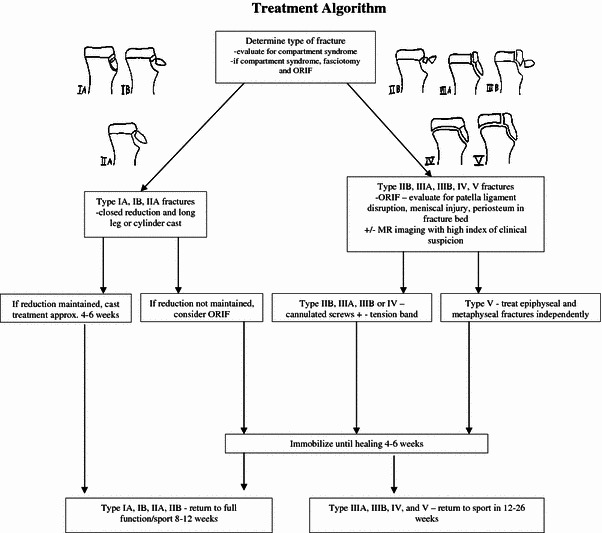
Tibial tuberosity algorithm. Modified Ogden classification of original classification provided by Sir Reginald Watson-Jones
Outcomes have generally been satisfactory in the literature. Henard and Bobo recommended ORIF for all Type I and III fractures (Ogden’s original classification) and closed reduction and casting for Type II fractures [21]. Christie and Dvonch reported excellent results with only one patient having minor decreased flexion in their eight patient study in which they casted Type I injuries and fixed most Type II and III injuries [5]. Chow et al. recommended non-operative management for Type IA and Type IIA fractures as long as the extensor mechanism was intact. They also recommended cast treatment for Type IIB fractures provided reduction could be obtained. They recommended surgical management involving cancellous screws and tension band wiring for all Type III fractures and reported excellent results with only ‘minor’ complications in their series of 16 patients [3]. In their report of 19 cases treated, Moiser and Stanitski reported their Type IA fracture was treated non-operatively. Their Type IB, IIA, and IIB fractures were treated non-operatively or with ORIF and their Type IIIA, IIIB and IV fractures were all treated with ORIF. They reported excellent results on all patients without any complications.
In our series, all fracture types were treated with ORIF (Fig. 4a–d). This could be misleading in terms of surgical indications unless each case is evaluated individually. We had no Type IA fractures. There were two Type IB fractures which were treated operatively because they were bilateral injuries in the same patient. The Type IC fracture (one case) was treated operatively because in addition to the tibial tuberosity fracture, there was a partial patella ligament avulsion from the patella which was also surgically repaired. For this patient, ROM was delayed until 5 weeks post-operatively. This patient did heal without any sequela. The three Type IIA fractures were treated operatively because two had clinical evidence of compartment syndrome, and the third one was the patient with osteogenesis imperfecta where early mobilization and weight-bearing was helpful to prevent metabolic issues. Of the three Type IIB fractures, one had compartment syndrome and the other two had disruption of their extensor mechanisms. All Type IIIA, IIIB and IV were treated operatively as indicated by fracture pattern. We are a tertiary trauma referral center, and therefore, our patient population may be likely skewed as most cases necessitating surgical intervention get referred to our center leading to referral bias.
Fig. 4.

a Plain lateral radiograph of the right knee in a 13-year-old patient with a type IB tibial tuberosity fracture. b Plain lateral radiograph of the left knee in the same patient. c Nine-month follow-up of the same patient demonstrating fixation of the right knee. d Nine-month follow-up of the same patient demonstrating fixation of the left knee
Complications included four patients with active or impending compartment syndromes (Type IIA (2) Type II B (1) and Type IV (1) fractures), all of which were appropriately treated with fasciotomies without sequelae. Additionally, there was one patient with arthrofibrosis who required an adhesiolysis for stiffness and removal of painful hardware with eventual resolution of symptoms. We had no patients with genu recurvatum, leg length discrepancy, malunion, non-union, skin necrosis, patella infera, re-fracture, or deep venous thrombosis. All of which have been reported previously in the literature in relation to this fracture.
Weaknesses in this study are that this is a retrospective review of multiple surgeons; therefore there was not a standardized protocol for treatment or post-operative protocol. Additionally, being a tertiary trauma referral center could have contributed to a referral bias.
In summary, tibial tuberosity fractures in adolescents, although uncommon, are clinically important injuries. Early recognition and treatment, as determined by fracture pattern, displacement, and associated complicating injuries, usually gives good results. All the patients in our series had surgical fixation as per different indications that have been elaborated. It is important for clinicians to recognize that compartment syndrome remains a significant concern post-injury and in the perioperative period. Close monitoring and timely intervention is recommended. Our recommendations for treatment and indications for surgery are as previously stated and outlined in our algorithm (Fig. 3). If surgery is indicated, fixation technique remains a matter of surgeon comfort and preference.
Acknowledgments
We acknowledge Dr. David A. Spiegel of Children’s Hospital of Philadelphia.
References
- 1.Balmat P, Vichard P, Pem R. The treatment of avulsion fractures of the tibial tuberosity in adolescent athletes. Sports Med. 1990;9(5):311–316. doi: 10.2165/00007256-199009050-00005. [DOI] [PubMed] [Google Scholar]
- 2.Bolesta MJ, Fitch RD. Tibial tubercle avulsions. J Pediatr Orthop. 1986;6(2):186–192. doi: 10.1097/01241398-198603000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Chow SP, Lam JJ, Leong JC. Fracture of the tibial tubercle in the adolescent. J Bone Joint Surg Br. 1990;72(2):231–234. doi: 10.1302/0301-620X.72B2.2312561. [DOI] [PubMed] [Google Scholar]
- 4.Christie MJ, Dvonch VM. Tibial tuberosity avulsion fracture in adolescents. J Pediatr Orthop. 1981;1(4):391–394. doi: 10.1097/01241398-198112000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Hand WL, Hand CR, Dunn AW. Avulsion fractures of the tibial tubercle. J Bone Joint Surg Am. 1971;53(8):1579–1583. [PubMed] [Google Scholar]
- 6.Mosier SM, Stanitski CL. Acute tibial tubercle avulsion fractures. J Pediatr Orthop. 2004;24(2):181–184. doi: 10.1097/01241398-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Ogden JA, Tross RB, Murphy MJ. Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg Am. 1980;62(2):205–215. [PubMed] [Google Scholar]
- 8.Kaneko K, Miyazaki H, Yamaguchi T. Avulsion fracture of the tibial tubercle with avulsion of the patellar ligament in an adolescent female athlete. Clin J Sport Med. 2000;10(2):144–145. doi: 10.1097/00042752-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 9.McKoy BE, Stanitski CL. Acute tibial tubercle avulsion fractures. Orthop Clin North Am. 2003;34(3):397–403. doi: 10.1016/S0030-5898(02)00061-5. [DOI] [PubMed] [Google Scholar]
- 10.Mirbey J, Besancenot J, Chambers RT, Durey A, Vichard P. Avulsion fractures of the tibial tuberosity in the adolescent athlete. Risk factors, mechanism of injury, and treatment. Am J Sports Med. 1988;16(4):336–340. doi: 10.1177/036354658801600405. [DOI] [PubMed] [Google Scholar]
- 11.Watson-Jones R. Fractures and joint injuries. 4. Baltimore: Williams & Wilkins; 1955. [PubMed] [Google Scholar]
- 12.Levi JH, Coleman CR. Fracture of the tibial tubercle. Am J Sports Med. 1976;4(6):254–263. doi: 10.1177/036354657600400604. [DOI] [PubMed] [Google Scholar]
- 13.Ryu RK, Debenham JO. An unusual avulsion fracture of the proximal tibial epiphysis. Case report and proposed addition to the Watson–Jones classification. Clin Orthop Relat Res. 1985;194:181–184. [PubMed] [Google Scholar]
- 14.Frankl U, Wasilewski SA, Healy WL. Avulsion fracture of the tibial tubercle with avulsion of the patellar ligament. Report of two cases. J Bone Joint Surg Am. 1990;72(9):1411–1413. [PubMed] [Google Scholar]
- 15.Curtis JF. Type IV tibial tubercle fracture revisited: a case report. Clin Orthop Relat Res. 2001;389:191–195. doi: 10.1097/00003086-200108000-00027. [DOI] [PubMed] [Google Scholar]
- 16.Ogden JA, Southwick WO. Osgood–Schlatter’s disease and tibial tuberosity development. Clin Orthop Relat Res. 1976;116:180–189. [PubMed] [Google Scholar]
- 17.Ehrenborg G, Engfeldt B. The insertion of the ligamentum patellae on the tibial tuberosity. Some views in connection with the Osgood–Schlatter lesion. Acta Chir Scand. 1961;121:491–499. [PubMed] [Google Scholar]
- 18.Blount W. Fractures in children. Baltimore: Williams & Wilkins; 1954. [Google Scholar]
- 19.Mosier S, Stanitski C, Levine R. Simultaneous bilateral tibial tubercle avulsion fracture. Orthopaedics. 2000;23(10):1106–1108. doi: 10.3928/0147-7447-20001001-30. [DOI] [PubMed] [Google Scholar]
- 20.Driessnack RP, Marcus NW. Fracture of an unossified tibial tubercle. J Pediatr Orthop. 1985;5(6):728–730. doi: 10.1097/01241398-198511000-00022. [DOI] [PubMed] [Google Scholar]
- 21.Henard DC, Bobo RT. Avulsion fractures of the tibial tubercle in adolescents. A report of bilateral fractures and a review of the literature. Clin Orthop Relat Res. 1983;177:182–187. [PubMed] [Google Scholar]
- 22.Georgiou G, Dimitrakopoulou A, Siapkara A, Kazakos K, Provelengios S, Dounis E. Simultaneous bilateral tibial tubercle avulsion fracture in an adolescent: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2007;15(2):147–149. doi: 10.1007/s00167-006-0164-0. [DOI] [PubMed] [Google Scholar]
- 23.Hamilton SW, Gibson PH. Simultaneous bilateral avulsion fractures of the tibial tuberosity in adolescence: A case report and review of over 50 years of literature. Knee. 2006;13(5):404–407. doi: 10.1016/j.knee.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 24.McKoy B, Stanitski C, Hartsock L. Bilateral tibial tubercle avulsion fractures with unilateral recurrence. Orthopaedics. 2006;29(8):731–733. doi: 10.3928/01477447-20060801-02. [DOI] [PubMed] [Google Scholar]
- 25.Slobogean GP, Mulpuri K, Alvarez CM, Reilly CW. Comminuted simultaneous bilateral tibial tubercle avulsion fractures: a case report. J Orthop Surg (Hong Kong) 2006;14(3):319–321. doi: 10.1177/230949900601400316. [DOI] [PubMed] [Google Scholar]
- 26.Wall JJ. Compartment syndrome as a complication of the Hauser procedure. J Bone Joint Surg Am. 1979;61(2):185–191. [PubMed] [Google Scholar]
- 27.Pape JM, Goulet JA, Hensinger RN. Compartment syndrome complicating tibial tubercle avulsion. Clin Orthop Relat Res. 1993;295:201–204. [PubMed] [Google Scholar]
- 28.Polakoff DR, Bucholz RW, Ogden JA. Tension band wiring of displaced tibial tuberosity fractures in adolescents. Clin Orthop Relat Res. 1986;209:161–165. [PubMed] [Google Scholar]
- 29.Wiss DA, Schilz JL, Zionts L. Type III fractures of the tibial tubercle in adolescents. J Orthop Trauma. 1991;5(4):475–479. doi: 10.1097/00005131-199112000-00015. [DOI] [PubMed] [Google Scholar]


