Abstract
Objective
Complete obstetrical brachial plexus palsy remains a difficult situation for the child and his/her family. The quality of spontaneous reinnervation is rarely good and always leads to a non-sensitive and non-functional hand, even if abduction of the shoulder and elbow flexion do spontaneously recover. The aim of this study was to assess the results from nerve reconstruction in cases of complete palsy and to demonstrate the effect of a change in surgical technique on the outcome of hand function.
Methods
Thirty pediatric patients with complete obstetric brachial plexus palsy were operated on in our department between 1987 and 2003. Twenty-five of these patients were clinically reviewed and evaluated by a physiotherapist and a surgeon (not the surgeon who performed the surgery). Functional assessment was based on the Gilbert shoulder score, the Gilbert–Raimondi score for elbow function and the Raimondi hand score. All children underwent a nerve reconstruction as graft and/or intra- or extra-plexual neurotization. Our neural surgical strategy changed between 1995 and 1996 to one that addresses the function of the hand and the wrist. A secondary surgical intervention was required in 18 cases. The most frequent procedures were a radial rotation osteotomy and a tendon transfer restoring wrist extension.
Results
Mean follow-up was 7 years and 10 months. Among children operated on with the first surgical strategy—the pre-1995–1996 period—hand function was good in three cases, satisfactory in four cases and unsatisfactory in one case. Among children for whom the second surgical strategy was used—1995–1996 and later—hand function was good or very good in eight cases, satisfactory in four cases and unsatisfactory in two cases. When the 25 patients were assessed for shoulder function, the functional result was good or very good in 12 cases, satisfactory in seven cases and unsatisfactory in six cases. In terms of elbow function, the results were good or very good in 14 cases, satisfactory in eight cases and unsatisfactory in three cases. All hands recovered sensation to a certain degree.
Conclusion
The surgical results are encouraging in terms of shoulder and elbow function, but not as good for hand function. With the change in neural surgical strategy in 1995–1996, when more focus was placed on the hand (second surgical strategy), the results on hand function improved relative to those obtained with the first surgical strategy. It must also be noted that hand recovery requires more time, which may partially explain why functional results are not as good for the hand as for the shoulder and elbow. These results demonstrate that early surgical exploration is useful in complete obstetrical brachial plexus palsies and that there is a need for neural reconstruction of the lower trunk.
Keywords: Hand palsy, Nervous reconstruction, Obstetric brachial plexus palsy
Introduction
The incidence of obstetrical brachial palsy reported in the literature varies between 0.5 [1] and 4.6 per thousand births [2]. Surgery is still considered an option for infants with proximal palsies [3], in contrast to infants with complete palsies who show no sign of recovery after 3 months [4]. There have been very few reports of surgical results on complete obstetrical brachial plexus palsies. The aim of our study was to assess the results following the surgical treatment of lesions associated with the nervous system from C5 to D1 and to report a change of surgical approach implemented by our orthopaedic department with the aim of improving hand function.
Materials and methods
Between 1987 and 2003, 35 patients were operated on for complete obstetrical brachial plexus palsy in the orthopaedic department of Trousseau Hospital, Paris (France). The same surgeon carried out each intervention. A clinical review was carried out on 25 of these patients by a surgeon other than the one who operated and a physiotherapist. The other ten children had been lost to follow-up. The patient cohort consisted of 14 boys and 11 girls. The right side was involved in 19 cases and the left side in six. We did not note any bilateral lesions. The average birthweight of the patient cohort was 4303.6 g (range 3500–5180 g) and that of the mothers at delivery was 80.3 kg (range 53–105 kg). All births were vaginal deliveries, and only one breech presentation was reported. Twenty-two patients presented with a Claude Bernard Horner syndrome.
The mean patient age at the time of surgery was 4.8 months (range 3–11 months). The only infant operated on who was older than 7 months was a tertiary referral and, consequently, a late referral to our department. Most patients were operated on between the age of 3 and 4.5 months.
Assessment of the results of upper limb palsy in children remains difficult. We therefore used scores employed in other surgical series to enable a comparison of our results with those of these earlier studies. We chose the Gilbert shoulder score for the shoulder [4] (Table 1), the Gilbert–Raimondi score [4] for elbow function for the elbow (Tables 2, 3), and the Raimondi hand score [4] for the hand (Table 4). The physiotherapist used the muscle strength score according to British Medical Council to assess muscle strength. The scale spans values of 0 to 3 for the non-cooperative child and from 0 to 5 for the cooperative one [5]. Electromyographic and imaging studies (cervical myelography at the beginning of our surgical series, with magnetic resonance imaging now being used) were performed preoperatively; however, the operative decision was based on the results of a clinical examination of the palsied hand in association with the absence of contraction of the biceps and deltoid muscles after the age of 3 months.
Table 1.
Score of the shoulder according to Gilbert [4]
| Score and criteria | Number of patients |
|---|---|
| 0: Stiff shoulder | 0 |
| I: Active abduction and antepulsion until 45°; no active external rotation | 3 |
| II: Active abduction < 90°; no active external rotation | 3 |
| III: Active abduction = 90°; weak active external rotation | 7 |
| IV: Active abduction < 120°; incomplete active external rotation | 11 |
| V: Active abduction > 120° active external rotation | 1 |
Table 2.
Scale of evaluation of the elbow (active movements)
| Movement assessed | Evaluation | Points |
|---|---|---|
| Flexion | No contraction or inefficient | 0 |
| Partial flexion | 2 | |
| Complete flexion | 3 | |
| Extension | No | 0 |
| Weak | 1 | |
| Good | 2 | |
| Lack of extension | 0–30° | 0 |
| 30–50° | −1 | |
| >50° | −2 |
Table 3.
Score of the elbow according to Gilbert and Raimondi [4]
| Description of scale | Points | Number of patients |
|---|---|---|
| I: Poor recovery | 0–1 | 3 |
| II: Satisfactory recovery | 2–3 | 8 |
| III: Good recovery | 4–5 | 14 |
Table 4.
Score of hand and wrist according to scale of Raimondi [4]
| Description of scale | Number of patients |
|---|---|
| I: Complete Palsy. Little but inefficient flexion of the fingers, inefficient thumb, no pinch, little or no sensitivity | 4 |
| II: Active but limited flexion of the fingers. No active extension of the fingers and of the wrist, lateral pinch of the thumb | 9 |
| II bis: Active extension of the wrist with passive flexion of the fingers (tenodese effect), lateral passive pinch of the thumb (in pronation) | 2 |
| III: Active flexion of the fingers and the thumb. Mobile thumb with partial abduction and opposition, intrinsic balance, no active supination, good possibilities for palliative surgery | 6 |
| IV: Active complete flexion of the fingers and the wrist, active extension of the wrist. No or weak extension of the fingers, good opposition of the thumb with ulnar intrinsic muscles + partial prono-supination | 4 |
| V: Hand of IV with extension of the fingers and complete prono-supination | 0 |
The surgical technique consisted of a preliminary injury exploration and assessment, followed by the reconstruction of nerves. Injuries were classified on the basis of surgical findings as either root avulsion or rupture with neuroma. Reconstruction of nerve injuries is performed by either grafts and/or neurotizations for the same infant, depending on the surgeon’s assessment of the quality of the section of the nerve roots. Our initial operative strategy, which reflected the state-of-the-art approach of the time [4], tended to favour shoulder and elbow function recuperation to the detriment of hand function. However, we modified our surgical strategy between 1995 and 1996, again in accordance with accepted surgical practices [4], and thereafter focussed on the distal part of the upper limb. Following surgery, standard protocol calls for the upper limb to be immobilized for 3 weeks after which physiotherapy is started. Secondary surgical interventions on the shoulder, elbow, forearm, and/or wrist were necessary in 18 children of our patient cohort. The most frequently required interventions were a rotation osteotomy of the radius and a tendon transfer to restore wrist extension. The mean age of the patient at the time of the secondary surgery was 4 years.
Results
Surgical exploration revealed 22 neuromas and three avulsions of the C5 root, 20 neuromas and five avulsions of C6, 14 neuromas and 11 avulsions of C7, three neuromas and 22 avulsions of C8 and five neuromas and 19 avulsions of D1 (Fig. 1). The D1 root was macroscopically normal in three cases, although as it did not respond to electrical stimulation during the operation, neurolysis only was performed. One patient presented with an avulsion of all roots.
Fig. 1.
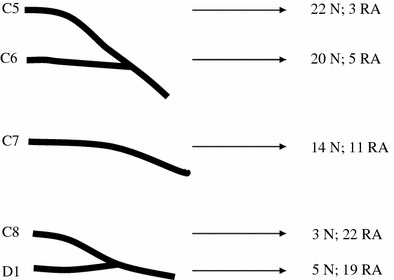
Anatomo-pathology of the injuries. N Neuroma, RA root avulsion
In four cases, neurotization only was performed without any grafts. In two cases, the spinal accessory nerve alone was used to neurotize the suprascapular nerve because all of the roots could not be used: in one child, the length of the C5 root was sufficient to directly neurotize the upper trunk; in the second child, a neuroma in continuity with the C5 root and a thin D1 root did not respond to direct electrical stimulation and, therefore, a neurolysis only was performed.
The first surgical strategy, which gives priority to the upper part of the limb, was used in eight patients. In six of these, the C5 root was used to reconstruct the musculo-cutaneous nerve, while in all eight of these patients, reconstruction of the suprascapular nerve was performed. The second surgical strategy was used on 14 children; the priority of this strategy is to improve hand function. In all of these children but one, a graft between the C5, C6 and/or C7 root was performed to reconstruct the lower trunk, C8 and/or D1. In the one exception, only C7 was available for nerve reconstruction of the upper trunk. A D1 neurolysis was performed in the remaining three patients.
Secondary nerve surgery was necessary in six patients. Intercostal nerves were used in three cases to neurotize the sensitive branch of the median nerve in order to improve hand sensitivity and the three remaining cases to neurotize the musculocutaneous nerve in order to provide elbow flexion.
A secondary surgery for shoulder function was necessary in two children. This surgery took the form of a subscapularis release aimed at improving external rotation of the shoulder. Restoration of elbow flexion was achieved once by a latissimus dorsi muscle transposition and three times by a teres minor transfer on the biceps tendon. Ten rotation osteotomies of the radius were used to correct supination stiffness of the forearm. Ten patients needed a tendon transfer (usually a flexor carpi ulnaris tendon transfer) to restore wrist extension. In one of these patients, wrist arthrodesis was eventually performed by another surgical team.
Prior to1995–1996, the goal of the surgical intervention was to give the child a stable shoulder, elbow flexion and a sensitive hand before; thereafter, the goal was to obtain maximal functional recovery of the hand. Here, we present the results of the shoulder and the elbow of both strategies together, but we report the results of the hand surgery according to the surgical strategy used.
The results for shoulder function were very good in one case, good in 11 cases, satisfactory in seven cases and unsatisfactory in six cases (Fig. 2). The results in both patients who underwent a subscapularis release were satisfactory. None of the shoulders were stiff, while unsatisfactory results corresponded to an abduction < 45°. All shoulders were stable.
Fig. 2.
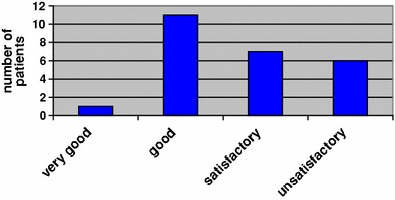
Outcome of the surgical strategies in terms of shoulder function
Recovery of elbow function according to the Gilbert–Raimondi score for elbow function was very good in 14 cases, good in eight cases and unsatisfactory in the other three cases (Fig. 3). Ten children were assessed as having complete active elbow flexion (3 points), 13 with partial flexion (2 points), and only two children with no active elbow flexion (0 points) (Table 2). For the three patients who underwent a neurotization of the musculocutaneous nerve by intercostal nerves, two had a very good result in terms of elbow function and one had a satisfactory result. Following tendon transfer to restore elbow flexion, the results were very good for two children, and satisfactory and unsatisfactory, respectively for two other children.
Fig. 3.
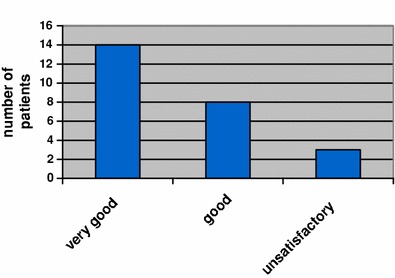
Outcome of the surgical strategies in terms of the elbow
Wrist and hand function were very good in four cases, good in six cases, satisfactory in 11 cases and unsatisfactory in four cases. Lack of wrist extension remains one of the main problems of such surgery. Ten of our patients did not have any wrist extension, and a tendon transfer to restore wrist extension was performed in these patients. This procedure proved successful in six patients. In one case, wrist arthrodesis was necessary to allow improved finger function and improve the cosmetic appearance of the fingers. In another case, a tendon transfer to improve finger extension was attempted; however, the outcome was poor due to a lack of muscle strength in the transferred and partial reinnervated muscles. In terms of neurotization of the sensitive branch of the median nerve by intercostal nerves, the results were satisfactory in two cases and unsatisfactory in the third case. According to the Gilbert–Raimondi score for elbow function, patients with very good and good results (scores of II to V) have a useful and functional hand. All children recovered hand sensitivity. With respect to hand and wrist function, the results were better if one considers a surgical strategy focusing on distal roots (C8 and D1) (Fig. 4). Among patients who underwent the latter strategy, we found two very good, six good, four satisfactory and two unsatisfactory results. Both of the unsatisfactory results involved children under the age of 4 years. Among the patients who underwent a previous surgical strategy, we observed three good, four satisfactory and one unsatisfactory result. Again, the unsatisfactory score was for children older than 4 years. In the three other patients, D1 root neurolysis alone was performed, resulting in one very good, one good and one satisfactory results.
Fig. 4.
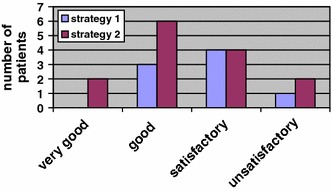
Results of the hand and the wrist according to the used surgical strategy. Strategy 1: repair of proximal roots favoured. Strategy 2: repair of distal roots favoured
Table 5 provides an overview of the patient cohort and surgical strategies and outcomes.
Table 5.
Surgical techniques, nerve injuries and reconstruction and outcomes of the surgery on the patients of this series
| Surgery | Long-term follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| Cases/ strategy used | Date of surgery | Postoperative follow-up | Nerve injuries | Nerve reconstruction | Complementary surgery | Score of shoulder (from 0 to V) | Score of elbow (from I to III) | Score of hand and wrist (from I to V) |
| 1/1st strategy | 10/01/1996 | 10 years 10 months | N C5-C6; RA C7; N C8-D1 | C5 → MC, C5 → UT, C8 → MN, D1 → UN, AS → SSN | Forearm osteotomy | IV | I | IV |
| 2/1st strategy | 01/09/1993 | 13 years 1 months | N C5-C6-C7; RA C8-D1 | C5 → SSN, C5 → MC, AS → MC | IC → MN, subscapularis release, wrist tendon transfer, forearm osteotomy | III | III | I |
| 3/1st strategy | 10/03/1995 | 11 years 5 months | N C5-C6-C7; RA C8-D1 | C5 → MC, C6 → MN, C7 → RN, AS → SSN | _ | III | III | II |
| 4/2nd strategy | 13/08/2003 | 3 years 3 months | N C5-C6; RA C7-C8-D1 | C5 → C8, C5/AS → UT | _ | I | II | I |
| 5/2nd strategy | 17/11/1998 | 7 years 9 months | N C5-C6; RA N C5-C6; | C5 → C8, C6 → D1, C6 → LC, AS → SSN | Forearm osteotomy | IV | III | II bis |
| 6/1st strategy | 17/03/1995 | 11 years 7 months | N C5-C6; RA C7-C8-D1 | C5 → MC, C5/C6 → MN, C5 → SSN, C6 → RN, C6 → AN | Wrist tendon transfer, forearm osteotomy | I | II | III |
| 7/2nd strategy | 19/02/1999 | 7 years 6 months | N C5-C6-C7; RA C8-D1 | C5/C7 → LC, C5/C7 → D1 | Wrist tendon transfer, forearm osteotomy | V | III | II |
| 8/1st strategy | 07/07/1993 | 13 years 3 months | N C5-C6; RA C7-C8-D1 | C5 → MC, C5/C6 → MN, AS → SSN | Wrist tendon transfer, forearm osteotomy | III | III | II |
| 9/2nd strategy | 10/07/2001 | 5 years 3 months | N C5; RA C6-C7-C8-D1 | C5 → C8, C5 → D1, AS → SSN | IC → MC, wrist tendon transfer | III | II | II |
| 10/– | 11/06/2003 | 3 years 2 months | N C5; RA C6-C7-C8; thin D1 | C5 and D1 neurolysis | Subscapularis release, wrist tendon transfer | III | II | III |
| 11/2nd strategy | 29/05/1995 | 11 years 2 months | N C5-C6-C7; RA C8-D1 | C5/C6 → MC, C5/C6 → C8, C5 → AN, C6 → D1 | Wrist tendon transfer | IV | III | III |
| 12/– | 12/05/1998 | 8 years 5 months | N C5-C6-C7; RA C8; N D1 | C5 → AN, C7 → LC, C7 → RN, D1 neurolysis, AS → SSN | IC → MN, radial head reduction, forearm osteotomy | IV | I | II |
| 13/1st strategy | 17/11/1992 | 13 years 8 months | N C6-C7; RA C5-C8-D1 | C7 → UT, AS → SSN | Elbow tendon transfer | IV | III | II bis |
| 14/2nd strategy | 26/03/2003 | 3 years 8 months | N C5-C6; RA C7; N C8-D1 | C5 → C8, C6 → D1, C6 → MC, AS → SSN | – | II | III | II |
| 15/1st strategy | 22/05/1996 | 10 years 5 months | N C5-C6-C7-C8-D1 | C5 → MC, C5 → MC, C8 → UT, AS → SSN | Elbow tendon transfer, forearm osteotomy | IV | I | II |
| 16/2nd strategy | 14/05/2003 | 3 years 2 months | N C5-C6-C7; RA C8-D1 | C5/C6/C7 → UT, C5/C6 → C8, C5 → D1 | – | III | III | I |
| 17/2nd strategy | 06/09/2000 | 6 years 1 months | N C5-C6-C7; RA C8-D1 | C7 → LT, C7 → MC, AS → SSN | – | IV | III | II |
| 18/1st strategy | 16/04/1991 | 15 years 6 months | RA C5-C6-C7-C8-D1 | AS → SSN | Elbow tendon transfer, wrist and digits tendon transfers, forearm osteotomy, wrist arthrodesis | IV | II | III |
| 19/2nd strategy | 09/06/1999 | 7 years 4 months | N C5-C6-C7-C8-D1 | AS → SSN | IC → MN, forearm osteotomy | I | II | I |
| 20/2nd strategy | 25/09/2002 | 4 years 2 months | N C5-C6-C7; RA C8-D1 | C5 → D1, AS → SSN | IC → MC | IV | III | III |
| 21/2nd strategy | 27/10/1995 | 11 years | N C5-C6-C7; RA C8-D1 | C5 → LC, C6 → D1, C7 → MT | Wrist and elbow tendon transfers | III | III | IV |
| 22/2nd strategy | 21/10/2003 | 3 years 1 month | N C5-C6-C7; RA C8-D1 | C5 → LT, AS → SSN | IC → MC | IV | III | III |
| 23/2nd strategy | 14/08/2002 | 4 years | N C5-C6-C7; RA C8-D1 | C5/C6 → LT, C6 → UT, AS → SSN | – | IV | II | II |
| 24/– | 28/02/2001 | 5 years 10 months | N C5-D1; RA C6-C7-C8 | C5 → UT, AS → SSN, D1 neurolysis | Wrist tendon transfer | II | II | IV |
| 25/2nd strategy | 15/09/2003 | 3 years 4 months | N C5-C6-C7; RA C8; thin D1 | C7 → C8 | – | II | III | IV |
N, Neuroma; RA, root avulsion; UT, upper trunk; MT, middle trunk; LT, lower trunk; LC, lateral cord; MC, medial cord; MCN, musculo-cutaneous nerve; MN, median nerve; AN, axillary nerve; RN, radial nerve; SA, spinal accessory nerve; SSN, suprascapular nerve; IC, intercostal nerves
Strategy 1, Repair of proximal roots favoured; strategy 2, repair of distal roots favoured
From a cosmetic point of view, the upper limb involved was always shorter than the opposite one. This shortening most frequently concerned the forearm (19 patients in our study). Length discrepancy was greater than 15% in only five children, and it did not worsen limb function.
Discussion
As in most patient series, we found that avulsions were the most frequent lesions on distal roots (C8 and D1). The most common lesions were neuroma in continuity with proximal roots (C5, C6 and C7) and avulsion of distal roots (C8 and D1). Avulsion of all roots was reported once. Surgical exploration was determined according to Gilbert and Tassin criteria [6]. In cases of complete obstetrical brachial palsies, the absence of bicipital contraction in an infant older than 3 months is considered to be a sign of poor spontaneous recovery [7]; as such, early neural surgery is proposed. Recovery of the flexion of the elbow before the age 3 of months is frequently a sign of good prognosis for global recovery. Many clinicians agree with this criteria and perform surgery before or at 6 months of age, when there is no antigravity biceps strength [8]. Gilbert et al. [9] and Vekris et al. [10] recommend surgery at age 3 months if there is hand palsy.
The difficult part of this surgery is the assessment of the root’s aspect and quality. It is the surgeon's decision to evaluate whether nerve grafting on this root is indicated or not, thus stressing the importance of the surgeon’s experience.
All patients had a good shoulder stability resulting from neurotization of the suprascapular nerve by the anterior branch of the spinal nerve, grafting of the upper trunk or grafting of the axillary nerve. One of these techniques was performed in all but one of our cases. Terzis [11] also considers suprascapular nerve neurotization to be a valuable procedure for restoration of gleno-humeral joint stability.
Our results for elbow flexion were good. Following surgery, only two patients did not have any active flexion. In these two cases, two roots at most could bear grafting, and priority was given to hand function recovery. When surgical exploration reveals that only a few roots can bear grafting, neurotization of the musculo-cutaneous nerve by the intercostal nerves is an efficient approach by which to recover some elbow flexion. This technique was used six times in our patient series, with three patients recovering complete elbow flexion, two recovering partial elbow flexion and one not recovering any flexion. Chuang [7] obtained similar good results and recommends this technique in children. However, results of neurotization with this latter technique are poorer in adults.
Functional results for the hand and wrist were overall less successful, although hand sensation was always regained. Hand sensitivity is essential to avoid spatial limb neglect and self-mutilation. It is also crucial to consider the hand as a relational organ. As reported by Masse [12], good elbow and shoulder function alone do not lead to incorporation of the limb into bimanual activities when there is insufficient hand sensitivity. These conclusions are confirmed in Dumont’s study [13]. It has been proven that function and sensation of the hand are important factors that affect the development of coordination patterns and body scale perception in infants [14]. In our study, eight patients were younger than 4 years at follow-up; however, as pointed out by Gilbert and Haerle [4], it is known that hand function (the hand being the most distal organ of the upper limb) takes more time to recover than shoulder and elbow function. Consequently, results on hand function may still improve in children up to 8 or 10 years of age. In a more recent study, Gilbert acknowledged early neural surgery for palsied hands to be of great interest. He reports a 35% rate of useful hands 2 years after surgery, with the results increasing to 76% 8 years after surgery [9]. Terzis and Kokkalis [15] recently reported similar results on palsied hands, demonstrating that early neural surgery on infants within 3 months of birth enabled greater functional hand recovery and reduced the need for secondary surgical procedures.
In conclusion, our modification to the surgical approach of complete obstetrical brachial plexus palsies, which is in line with recent recommendations [4,15] and were implemented to improve hand recovery, gives reasonably good results. Our second surgical strategy resulted in more functional hands, which are a very different issue than the “main en breloque”, commonly observed in complete palsies.
References
- 1.Rubin A. Birth injuries: incidence, mechanisms and end results. Obstet Gynecol. 1964;23:218–221. [PubMed] [Google Scholar]
- 2.Hentz VR. Congenital brachial plexus exploration. Tech Hand Up Extrem Surg. 2004;8:58–69. doi: 10.1097/01.bth.0000127363.67917.7f. [DOI] [PubMed] [Google Scholar]
- 3.Strömbeck C, Krumlinde-Sundholm L, Forssberg H. Functional outcome at 5 years in children with obstetrical brachial plexus palsy with and without microsurgical reconstruction. Dev Med Child Neurol. 2000;42(3):148–157. doi: 10.1017/S001216220000027X. [DOI] [PubMed] [Google Scholar]
- 4.Haerle M, Gilbert A. Management of complete obstetric brachial plexus lesions. J Pediatr Orthop. 2004;24:194–200. doi: 10.1097/01241398-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Romana MC, Goubier JN. Paralysie obstétricale du plexus brachial. Encyclopédie méd chir. 2000;15:1–5. [Google Scholar]
- 6.Gilbert A, Tassin J. Réparation chirurgicale du plexus brachial dans la paralysie obstétricale. Chirurgie. 1984;110:70–75. [PubMed] [Google Scholar]
- 7.Chuang DC, Mardini S, Ma HS. Surgical strategy for infant obstetrical brachial plexus palsy: experiences at Chang Gung Memorial Hospital. Plast Reconstr Surg. 2005;116(1):132–142. doi: 10.1097/01.PRS.0000169936.19073.B4. [DOI] [PubMed] [Google Scholar]
- 8.O’Brien DF, Park TS, Noetzel MJ, Wearthely T. Management of birth brachial plexus palsy. Childs Nerv Syst. 2006;22(2):103–112. doi: 10.1007/s00381-005-1261-y. [DOI] [PubMed] [Google Scholar]
- 9.Gilbert A, Pivato G, Kheiralla T. Long-term results of primary repair of brachial plexus lesions in children. Microsurgery. 2006;26(4):334–342. doi: 10.1002/micr.20248. [DOI] [PubMed] [Google Scholar]
- 10.Vekris MD, Lykissias MG, Beris AE, Manoudis G, Vekris AD, Soucacos PN. Management of obstetrical brachial plexus palsy with early plexus microreconstruction and late muscle transfers. Microsurgery. 2008;28(4):252–261. doi: 10.1002/micr.20493. [DOI] [PubMed] [Google Scholar]
- 11.Terziz JK, Kostas I. Outcomes with suprascapular nerve reconstruction in obstetrical brachial plexus patients. Plast Reconstr Surg. 2008;121(4):1267–1278. doi: 10.1097/01.prs.0000305537.74910.bf. [DOI] [PubMed] [Google Scholar]
- 12.Masse P. Obstetrical paralysis of the brachial plexus plexus. II therapeutics:treatement sequelaesurgical possibilities for the elbow and the hand. Rev Chir Orthop Reparatrice Appar Mot. 1972;58(Suppl 1):196–200. [PubMed] [Google Scholar]
- 13.Dumont CE, Forin V, Asfazadourian H, Romana C. Function of the upper limb after surgery for obstetric brachial plexus palsy. J Bone Joint Surg Br. 2001;83-B:894–900. doi: 10.1302/0301-620X.83B6.11389. [DOI] [PubMed] [Google Scholar]
- 14.Bellew M, Kay SPJ, Webb F, Ward A. Developmental and behavioural outcome in obstetric plexus palsy. J Hand Surg [Br] 2000;25-B:49–51. doi: 10.1054/jhsb.1999.0331. [DOI] [PubMed] [Google Scholar]
- 15.Terziz JK, Kokkalis ZT. Outcomes of hand reconstruction in obstetric brachial plexus palsy. Plast Reconstr Surg. 2008;122(2):516–526. doi: 10.1097/PRS.0b013e31817d6139. [DOI] [PubMed] [Google Scholar]


