Abstract
Background
We describe a new method for corrective osteotomy and the fixation of lower limb deformities in children.
Methods
Following osteotomy, the desired position is obtained and temporarily stabilized using an external fixator. Definitive fixation is performed with a plate and locking screws inserted percutaneously under fluoroscopic guidance. The procedure was performed in 18 segments in 11 patients. Corrections were performed in all planes.
Results
The mean follow up was 18 months (range 6–36 months). All patients were corrected to within 2° of that which was planned. Union was obtained in 16 segments in ten patients within 6–16 weeks.
Conclusions
The method was found to be effective for the correction of deformity in the pediatric population. Advantages compared to conventional methods include minimal soft tissue dissection and the ability to adjust the position before definitive fixation.
Keywords: Limb deformity, Osteotomy, External fixation, Locking plate
Introduction
Corrective osteotomies are commonly used in pediatric orthopedics for a wide range of indications. Corrections can be performed acutely or gradually. Fixation can be internal, external, or a combination of both, with each method having advantages and disadvantages. External fixators enable further correction after the initial surgery, but carry an inherent incidence of pin tract infection. Internal fixators usually require extensive dissection for insertion [1–5].
The purpose of this study is to present a technique for corrective osteotomy combining temporary external fixation during the procedure, with definitive fixation using a locking plate inserted through a small incision. The technique is applicable for correction in any plane in a long bone.
Patients and methods
The study design was a retrospective case series. After institutional review board approval, all children treated by the described method between January 2005 and December 2007 in our institution were included in the study. All charts and radiographs were reviewed.
During the study period, the method was used to correct deformities in 18 limb segments in 11 patients. All patients treated by this method during this period were included in the study and none were excluded. Patients who required concomitant lengthening were treated by different means and were not included in the study.
Patient demographics, underlying pathologies, and location and type of deformities are described in Table 1. Sagittal and transverse plane deformities were measured clinically using a goniometer: flexion and extension at the knee were measured by the knee range of motion with the hip in extension. Foot progression angles were measured during ambulation, hip rotation was measured in the prone position with the knee in flexion, and tibial torsion was estimated by the thigh–foot angle. Coronal plane deformities were measured radiographically on erect anterior posterior long leg films as described by Paley [2]. Correction was performed as close as possible to the center of rotation of angulation (CORA). When the correction was not at the CORA, displacement was performed to obtain a straight mechanical axis of the limb, measured intra-operatively by C-arm fluoroscopy with the electrocautery cable used as a marker. The plates used were Synthes™ 4.5/5.0-mm locking compression plates (LCP). Straight narrow plates were used for diaphyseal corrections both in the femur and the tibia. Distal femoral plates were utilized for osteotomies performed in the distal femoral metaphysis. As these latter plates cross the growth plate, they were utilized in patients with closed growth plates (Patients 5, 6, 8, and 9).
Table 1.
Patient demographics
| No. | Pt. | Diagnosis | Age (years) | Segments | Bone | Deformity |
|---|---|---|---|---|---|---|
| 1 | K.O. | CP | 6.4 | 2 | Femur | Internal torsion |
| 2 | M.A. | CP | 7.7 | 2 | Femur | Internal torsion |
| 3 | S.E. | Microcephaly | 6.9 | 2 | Tibia | Internal torsion |
| 4 | A.E. | Giant axonal neuropathy | 8.4 | 2 | Tibia | External torsion |
| 5 | K.O. | CP | 15.8 | 2 | Femur | Flexion |
| 6 | N.D. | Post-fracture | 13.2 | 1 | Femur | Valgus + flexion |
| 7 | G.G. | Behr syndrome | 14.5 | 1 | Femur | Internal torsion |
| 8 | S.M. | Developmental genu valgus | 16.7 | 2 | Femur | Valgus + external torsion |
| 9 | S.O. | Achondroplasia | 15.5 | 2 | Femur | Varus |
| 10 | S.G. | Developmental genu valgus overcorrection by epiphysiodesis | 14.5 | 1 | Femur | Varus |
| 11 | G.A. | Renal osteodystrophy | 11.0 | 1 | Femur | Valgus |
Smaller 3.5-mm plates are available but were not utilized in our series.
Surgical technique
The osteotomy is pre planned and an appropriate locking plate is selected. The plate outline is marked on the skin.
Two Schanz pins are placed on either side of the planned osteotomy site. The direction of the pins is such that they will be in line in the corrected position following the osteotomy, taking into consideration all planes of the planned correction (Fig. 1). An attempt is made to place the pins proximal and distal to the planned plate location, but if this is not possible (mainly in the distal femur), the pins are placed anterior or posterior to the planned plate location.
The osteotomy is performed through a 2–3-cm-long incision. Any osteotomy method is acceptable.
The deformity is corrected and an external fixator rod is placed, stabilizing the osteotomy in the desired position, which is checked clinically and radiographically, making adjustments as necessary.
The plate is inserted in the submuscular–extraperiosteal plane, first in the direction of the longer fragment and then in the direction of the shorter fragment (Fig. 2).
Two to three locking screws are inserted on each side of the osteotomy (Fig. 3). Insertion can be through the osteotomy incision with additional percutaneous separate incisions. The number of screws placed in each fragment varies with the size of the patient and the quality of the osteotomized bone. A minimum of two screws per segment is recommended [1].
The external fixator is removed and all incisions are closed.
Fig. 1.

Plate planning and Schanz pin insertion
Fig. 2.

Correction, external fixation, and submuscular insertion of the locking plate
Fig. 3.

Percutaneous insertion of locking screws
Aftercare
Postoperatively, partial weight-bearing ambulation using a walker or crutches was started as soon as possible, usually on the second or third postoperative day.
Full weight-bearing was permitted at 6 weeks postoperatively.
Results
Surgery was performed on 14 femurs and four tibias. The osteotomy site was in the diaphysis in ten segments (Fig. 4) and in the metaphysis in eight (Fig. 5a). Multiple drill holes and an osteotome were used in 16 segments and a Gigli saw in two. The number of screws placed in each segment varied from two to four. This was determined by the size of the patient and the quality of the bone.
Fig. 4.
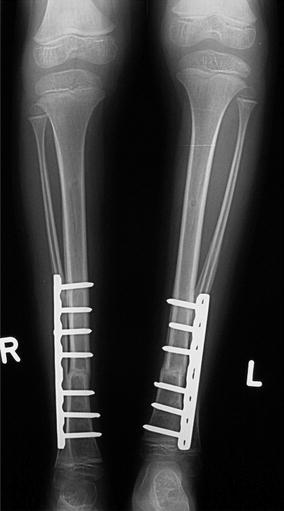
Patient no. 3: 10 weeks after tibial derotation osteotomies showing advanced union
Fig. 5.
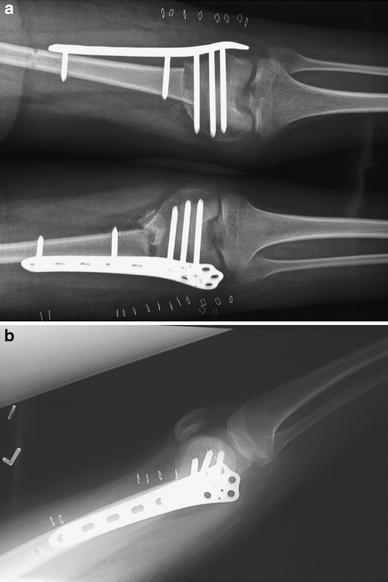
Patient no. 5: extension osteotomy in the distal femur of a patient with closed growth plates using a distal femoral locking compression plate (LCP)
Correction was performed in one plane in 15 segments: transverse plane derotation was performed in nine segments (Fig. 4), coronal plane correction was performed in four, and sagittal plane in two segments (Fig. 5b). A multiplanar correction was performed in three segments, combining varus and derotation in two patients and varus and extension in one. In the patients undergoing transverse plane correction, the indication was severe rotational deformity compromising gait efficiency, with the derotation goal being between 30° and 45°. This was achieved in all cases. The mean coronal plane correction goal was 14° (range 10°–18°) and the sagittal correction goal was 15°–40° Postoperatively, all patients’ alignment was within 2° of the planned correction (Tables 2 and 3).
Table 2.
Planned and achieved correction
| Pt. no. | Planned correction | Achieved correction |
|---|---|---|
| 1 | 30° derotation | 30° derotation |
| 2 | 30° derotation | 30° derotation |
| 3 | 45° derotation | 45° derotation |
| 4 | 40° derotation | 40° derotation |
| 5 | 30°/40° extension | 30°/40° extension |
| 6 | 10° varus; 15° extension | 10° varus; 15° extension |
| 7 | 40° derotation | 40° derotation |
| 8 | 14°/11° varus; 30° derotation | 14°/10° varus 30° derotation |
| 9 | 18°/15° valgus | 18°/15° valgus |
| 10 | 14° valgus | 13° valgus |
| 11 | 15° varus | 13° varus |
Table 3.
Preoperative and postoperative rotation profile in patients undergoing derotation osteotomies
| Pt. no. | Segment | Preoperative Rt/Lt | Postoperative Rt/Lt |
|---|---|---|---|
| 1 | Femur Rt + Lt | FPA = −40/−40, IR = 80/80, ER = 20/20 | FPA = 0/0, IR = 45/45, ER = 45/45 |
| 2 | Femur Rt + Lt | FPA = −30/−30, IR = 85/85, ER = 30/30 | FPA = 0/0, IR = 45/45, ER = 60/60 |
| 3 | Tibia Rt/Lt | FPA = −40/−40, TFA = −40/−40 | FPA = 0/0, TFA = 0/0 |
| 4 | Tibia Rt/Lt | FPA = −40/−40, TFA = −45/−45 | FPA = 0/0, TFA = 0/0 |
| 7 | Femur Lt | FPA = −40/−40, IR = 90/80, ER = 30/45 | FPA = 0/0, IR = 45/45, ER = 45/70 |
FPA: foot progression angle; TFA: thigh–foot angle; IR: internal rotation; ER: external rotation
Union was achieved in 16/18 segments in a mean time of 12 weeks [6–16].
At mean follow up of 23 months (range 6–42), correction was maintained in all patients.
Plates were removed uneventfully in five patients. This was done as a day surgery procedure removing the screws through percutaneous incisions and the plate through the original incision or through an additional small incision at the tip of the plate.
Complications
There was one superficial wound infection which resolved after intravenous antibiotic treatment. One patient experienced a hypotrophic non union of bilateral tibial derotations. This may have been due to the fact that a fibular osteotomy was not performed at the time of initial surgery. One year postoperatively, the plates were removed and a fibulotomy was performed. Six months later, there were signs of union on the left side, and on the right side, the patient underwent a replating with bone graft due to persistent non union. Six months postoperatively, there was full union in both tibias.
One patient fell 6 weeks postoperatively and sustained a fracture through the proximal screw of the plate. She was treated by replating to include both the osteotomy site (which was united) and the fracture (Fig. 6).
Fig. 6a–d.

Patient no. 11. a 15° mechanical axis valgus deformity of the right femur due to renal osteodystrophy. b Following a diaphyseal varus corrective osteotomy with correction of the mechanical axis to 2° valgus. c Fracture through proximal screw 6 weeks postoperatively. d Following replating, the osteotomy is united
Discussion
Corrective osteotomies can be performed and fixed using various methods and fixation devices. Correction can be performed acutely or gradually, and fixation can be external or internal. Gradual correction using external fixators has the advantage of lessening the risk of neurovascular damage and enables limb lengthening. However, it is cumbersome, causes muscle impingement by the pins, and will cause infectious episodes in a high percentage of patients. It does enable position adjustments postoperatively as well as secondary corrections. Internal fixation does not have these disadvantages; however, traditional open fixation methods require wide exposure and do not enable any change in position once initial fixation is obtained [2, 14–16].
The method described in this study combines advantages from both methods. The temporary fixation enables position adjustments after radiographic evaluation but before definitive fixation. This definitive fixation is internal, avoiding the cumbersomeness and infectious complications of external fixators and the percutaneous insertion avoids the wide dissection used in traditional plating.
Similar methods have been previously described combining temporary external fixation and internal devices for the definitive fixation [2–5]; however, most of these authors used either conventional plating necessitating wide exposure or intramedullary nails [2–4]. Insertion of these nails in a retrograde fashion through the distal femur is contraindicated in patients with open growth plates, and proximal insertion carries an increased danger of avascular necrosis of the femoral head in skeletally immature patients. A recent study by Rogers et al. [5] describes a technique using the Taylor Spatial Frame for the correction of deformities in the distal femur of adult patients, with definitive fixation performed using either an intramedullary nail or a locking plate, similar to the one used in the present study for distal femoral corrections.
The use of locking plates in orthopedics is relatively new [1, 6]. Only a few studies have described their use in the pediatric population for fracture fixation [7, 8] and following limb lengthening [9, 10] and tumor resection [11]. This is, to our knowledge, the first study describing locking plate use for corrective osteotomies in children.
The advantages of locking plates include increased stability [1, 12], as well as minimal soft tissue damage due to their insertion in the submuscular–extraperiosteal plane and the percutaneous insertion of both the plates and the screws. Although the stability obtained with traditional compression plates is probably adequate for pediatric patients, the reduction of the soft tissue dissection is a significant advantage and may promote earlier rehabilitation, especially in neuromuscular patients. However, the wide variability in patients and underlying pathologies in the current study precludes evaluation of the clinical course in those treated and comparison to conventional methods.
Plates were removed in five of our patients. In one of them, the indication for removal was non union of the osteotomies, one patient complained of prominence of the plates, and in the three remaining patients, plates were removed as part of our treatment protocol. Although the need for routine plate removal is not a fully resolved question [12], we feel that the system may act as a stress riser and cause fractures as it did in patient no. 11 (Fig. 6). The removal procedure proved to be short and safe in our series, and we, therefore, generally recommend plate removal to our patients.
Locking plates do have several disadvantages. They are less effective than conventional plates in the reduction of the fragments. Although some reduction can be obtained using compression screws, the fragments should be reduced and stabilized before the locking plate is inserted. The method described in the current study directly addresses this problem. The fragments are placed in the desired position and rigidly fixed before locking plate insertion. The rigidity of the system as well as the lack of compression between the fragments may lead to union problems. Screws should be placed at an adequate distance from the osteotomy site in order to increase the flexibility of the system [1]. This rigidity may have been the cause of the problem in the one patient in whom we encountered non union of both tibial osteotomies; however, this may also have been due to the fact that a fibular osteotomy was not performed initially. Cross-threading and cold-welding may occur in locking plates, causing difficulty during hardware removal. We did not encounter these in any of our cases. However, if they do occur, screws can be removed and plates can be cut using metal-cutting instruments.
The study has limitations—the relatively small number of patients, the varied etiologies, deformity types, and bone segments, and the short follow up. However, the purpose of the study was to present the surgical technique and its efficacy and we, therefore, feel that the fact that it was utilized successfully in these varied pathologies demonstrates the wide applicability of the technique. We also felt that, being a technique description, follow up until union was adequate in the present study.
Further studies will be needed to compare the long-term results of the procedure to those using previously described methods.
Footnotes
Level of evidence: Level IV. Retrospective case series.
References
- 1.Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003;34(Suppl 2):B63–B76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 2.Paley D. Principles of deformity correction. New York: Springer; 2002. pp. 300–302. [Google Scholar]
- 3.Gugenheim JJ, Jr, Brinker MR. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J Bone Joint Surg Am. 2003;85:1229–1237. doi: 10.2106/00004623-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Eralp L, Kocaoglu M, Cakmak M, Ozden VE. A correction of windswept deformity by fixator assisted nailing. A report of two cases. J Bone Joint Surg Br. 2004;86(7):1065–1068. doi: 10.1302/0301-620X.86B7.14923. [DOI] [PubMed] [Google Scholar]
- 5.Rogers MJ, McFadyen I, Livingstone JA, Monsell F, Jackson M, Atkins RM. Computer hexapod assisted orthopaedic surgery (CHAOS) in the correction of long bone fracture and deformity. J Orthop Trauma. 2007;21(5):337–342. doi: 10.1097/BOT.0b013e3180463103. [DOI] [PubMed] [Google Scholar]
- 6.Smith WR, Ziran BH, Anglen JO, Stahel PF. Locking plates: tips and tricks. J Bone Joint Surg Am. 2007;89:2298–2307. doi: 10.2106/JBJS.F.00615. [DOI] [PubMed] [Google Scholar]
- 7.Sink EL, Hedequist D, Morgan SJ, Hresko T. Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Pediatr Orthop. 2006;26:177–181. doi: 10.1097/01.bpo.0000218524.90620.34. [DOI] [PubMed] [Google Scholar]
- 8.Hedequist D, Bishop J, Hresko T. Locking plate fixation for pediatric femur fractures. J Pediatr Orthop. 2008;28:6–9. doi: 10.1097/bpo.0b013e31815ff301. [DOI] [PubMed] [Google Scholar]
- 9.Uysal M, Akpinar S, Cesur N, Hersekli MA, Tandoğan RN. Plating after lengthening (PAL): technical notes and preliminary clinical experience. Arch Orthop Trauma Surg. 2007;127:889–893. doi: 10.1007/s00402-007-0442-4. [DOI] [PubMed] [Google Scholar]
- 10.Iobst CA, Dahl MT. Limb lengthening with submuscular plate stabilization: a case series and description of the technique. J Pediatr Orthop. 2007;27:504–509. doi: 10.1097/01.bpb.0000279020.96375.88. [DOI] [PubMed] [Google Scholar]
- 11.Buecker PJ, Berenstein M, Gebhardt MC, Hornicek FJ, Mankin HJ. Locking versus standard plates for allograft fixation after tumor resection in children and adolescents. J Pediatr Orthop. 2006;26:680–685. doi: 10.1097/01.bpo.0000230333.73286.06. [DOI] [PubMed] [Google Scholar]
- 12.Snow M, Thompson G, Turner PG. A mechanical comparison of the locking compression plate (LCP) and the low contact-dynamic compression plate (DCP) in an osteoporotic bone model. J Orthop Trauma. 2008;22:121–125. doi: 10.1097/BOT.0b013e318160c84c. [DOI] [PubMed] [Google Scholar]
- 13.Peterson HA. Metallic implant removal in children. J Pediatr Orthop. 2005;25:107–115. doi: 10.1097/00004694-200501000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006;26:794–798. doi: 10.1097/01.bpo.0000242375.64854.3d. [DOI] [PubMed] [Google Scholar]
- 15.Pinkowski JL, Weiner DS. Complications in proximal tibial osteotomies in children with presentation of technique. J Pediatr Orthop. 1995;15(3):307–312. doi: 10.1097/01241398-199505000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Slawski DP, Schoenecker PL, Rich MM. Peroneal nerve injury as a complication of pediatric tibial osteotomies: a review of 255 osteotomies. J Pediatr Orthop. 1994;14(2):166–172. doi: 10.1097/01241398-199403000-00007. [DOI] [PubMed] [Google Scholar]


