Abstract
Objective
To examine whether pre-abuse rates and patterns of emergency department (ED) visits between children with supported child abuse and age-matched controls are useful markers for abuse risk.
Study design
A population-based case-control study using probabilistic linkage of four statewide data sets. Cases were abused children <13 years, identified between 1/1/01–12/31/02. For each case, a birth date matched population-based control was obtained. Outcome measures were rate ratios of ED visits in cases compared with controls.
Results
9795 cases and 9795 controls met inclusion criteria. 4574 cases (47%) had an ED visit; thus linked to the ED database versus 2647 controls (27%). The crude ED visit rate per 10 000 person-days of exposure was 8.2 visits for cases compared with 3.9 visits for controls. Cases were almost twice as likely as controls (adjusted rate ratio = 1.8, 95% CI:1.5, 1.8) to have had a prior ED visit. Leading ED discharge diagnoses were similar for both groups.
Conclusions
Children with supported child abuse have higher ED use prior to abuse diagnosis, when compared with the general pediatric population. However, neither the rate of ED use nor the pattern of diagnoses offers sufficient specificity to be useful markers of risk for abuse.
Child abuse is the fourth leading cause of childhood death in the United States.(1) Current evidence suggests that many children who die from child abuse are seen by a health care provider for medical conditions related to abuse prior to the diagnosis, possibly resulting in a missed opportunity for intervention. (2–12) For example, King studied a cohort of fatally abused children and found that almost 20% of the children had documented contact with the health care community for reasons other than routine care within a month before death. (7) Similarly, Jenny et al found that 31% of children with abusive head trauma had been seen by a health care provider prior to recognition of their head injury, with a mean time to correct diagnosis in these children of seven days. (2)
These studies suggest that the ED may be a clinical setting where there is an opportunity for earlier identification of both physical and sexual child abuse; 12 however, there is little information on whether abused children are evaluated in the ED setting prior to the diagnosis of child abuse more than the general pediatric population.
The aim of this study was to examine whether there are specific patterns of ED use unique to children later found by child protective services to be abused compared with the general ED population. We hypothesized that children who experienced abuse would use ED services at a higher rate than the general population prior to the event resulting in the diagnosis of child abuse. In addition, we hypothesized that certain diagnostic spectrums would be associated with specific abuse types, and would vary from the diagnostic spectrum of the general pediatric population. The recognition of diagnostic patterns of ED use might then enable screening for children in the ED who are at higher risk of abuse, before serious or fatal injuries occur.
METHODS
This population-based case-control study compares ED utilization patterns between Utah-born children with a supported Division of Child and Family Services (DCFS) child abuse report for whom the initial disclosure of abuse occurred between January 1, 2001 and December 31, 2002 and age-matched controls. This study was approved by the University of Utah Institutional Review Board and Division of Child and Family Services Institutional Review Board. A Waiver of Informed Consent was obtained from both boards.
Definitions
Cases
Cases were defined as children less than 13 years of age who were born in Utah and who had an abuse event supported by the State of Utah DCFS. Cases of physical abuse, sexual abuse, neglect, emotional abuse or exposure to domestic violence as defined by state and federal statutes were included (Appendix 1; available at www.jpeds.com). Children in the DCFS dataset for fetal addiction or alcohol exposure, living in a house where abuse had occurred for another victim (but was not witnessed by the child), or abandonment were excluded. A supported case of abuse is a case in which an investigation was performed and a DCFS worker found abuse, neglect, or dependency occurred. A subset of child cases whose parent had a valid Utah driver license during the study period was selected for additional analysis.
Population-based, age-matched controls
A control child matched by birth date was randomly selected from the Utah birth certificate database for each case. In order to assure that controls were resident in Utah during the study period a linkage was performed between the driver license database and either parent listed in the birth registry. Only children whose mother or father had an active Utah driver license during the study period were eligible for selection as a control. In addition, Utah birth records that linked to either a Utah death certificate prior to 2002 or to a DCFS case were excluded from birth certificates eligible for selection.
Covariates
Child characteristics included sex, age, and abuse type. Maternal characteristics, obtained from the birth certificate file, included race and ethnicity (white versus non-white, Hispanic versus non-Hispanic), education level (< high school, high school graduate, > high school), and grouped age (< 18 years, 18–24 years, ≥ 25 years). Race and ethnicity were included as minority children may be over-represented in the DCFS database compared with the general population in Utah.
Outcome Measures
The primary outcome of interest was the rate of ED visits in the study period prior to the ascertainment of the confirmed abuse. To determine the rate of ED visits, all ED visits between January 1, 1999 (or the child’s birth date for children born after January 1, 1999) and the end date (where end date is defined as the date of DCFS investigation initiation for each case and matched control) were counted. ED visits that occurred on the same date as the DCFS report was filed were excluded, as we were interested in only those ED visits in which the diagnosis of abuse was not made. The total exposure period (in days) was calculated from either the child’s birth date (for children born after January 1, 1999) or January 1, 1999 through the date prior to DCFS investigation.
Several secondary outcomes were explored. These included: rates of ED visits that were temporally related to the abuse investigation, specifically visits in the seven day period prior to the start of the DCFS investigation; rates of ED visits by type of abuse; and rates by insurance type among those with ED visits prior to the ascertainment of the supported abuse.
Finally, in order to describe diagnostic patterns of ED use, the top six ICD-9 (13) diagnosis codes from discharge data were examined to determine whether specific patterns existed for cases compared with controls. All ICD-9 codes from each ED visit were then grouped into broad categories including injury, illness, poisoning, psychological and other. Cases with physical abuse, neglect and sexual abuse were then analyzed separately to explore whether or not there were differences in categories of visits: injury visits for children with physical abuse or neglect and psychiatric visits in children who were victims of sexual abuse.
Procedures
Utah DCFS, birth certificate, death certificate and emergency department state-wide databases (Appendix 2; available at www.jpeds.com) were probabilistically linked pair-wise using LinkSolv.(14) Methods of data linkage have been described previously. (15–17) An additional linkage was made from the mother or the father’s name on the birth certificate to the driver license database. For each linkage performed, only matches with high probabilities (> 0.9) of being actual pairs were kept. The linked database was maintained in Microsoft SQL Server 8 (Microsoft Corp, Redmond, WA).
Statistical Analysis
Demographics of cases and controls were described using frequencies and percents. Frequencies of ICD-9 codes were described for both cases and controls. The rate of ED visits per 10 000 person days for cases and controls were calculated. Adjusted rate ratios (aRR) with 95% confidence intervals (CI) were calculated using negative binomial regression, keeping all covariates including maternal characteristics, child sex, and case/control status.
Sub-analyses of rates of ED use adjusted for maternal characteristics and child sex were performed for each abuse type using negative binomial regression.
To examine whether using control families with driver licenses biased the results, rates were calculated using the sub-group of cases who had a parent with a valid Utah driver license and compared with cases whose parents did not have a valid driver license.
Statistical analysis was performed using SAS 9.0 (SAS Institute, Cary, NC). Significance was set at 0.05 and 95% CI are reported.
RESULTS
Cases
There were 19 005 children in the state of Utah with supported abuse during the study period. Of these, 52% (n= 9795) met study inclusion criteria. Of those children who were excluded, 46% (n=4459) were due to age ≥ 13 years, 40% (n=3888) for not having a Utah birth record, and 9% (n=863) for ineligible abuse type.
The majority (79%) of the cases were white, reflecting the general population of Utah (89.2% white),(18) 58% (n=5718) had a parent with a valid Utah driver license during the study period and 73% (n =7106) experienced a single type of abuse. Domestic violence exposure accounted for the largest number (41%) of the supported cases. (Table I).
Table I.
Demographic and emergency department visits characteristics of 0cases and controls (N=19 590)
| Demographics | Cases n=9795 | Birth Certificate Controls n=9795 |
|---|---|---|
| Age in years, median (Q1, Q3) | 5 (2, 8) | 5 (2, 8) |
| Children ≤ 36 months (%) | 2751 (28.1%) | 2751 (28.1%) |
| Sex (% male) | 4748 (48.5%) | 5101 (52.1%) |
| Mother/Father with Valid Driver License (%) | 5718 (58.4%) | 9795 (100%) |
| Abuse Types n (%)* | ||
| Physical | 1314 (13.4%) | NA |
| Sexual | 1734 (17.7%) | NA |
| Neglect | 2865 (29.3%) | NA |
| Emotional | 1146 (11.7%) | NA |
| Domestic violence | 3967 (40.5%) | NA |
| Counts of Abuse n (%) | ||
| One | 7106 (72.5%) | NA |
| Two | 1769 (18.1%) | NA |
| Three or more | 920 (9.4%) | NA |
| Maternal Characteristics At Birth | ||
| Maternal Race/Ethnicity n (%) | ||
| White Non-Hispanic | 7739 (79.0%) | 8813 (90.0%) |
| Hispanic | 1402 (14.3%) | 629 (6.4%) |
| Other Non-Hispanic | 617 (6.3%) | 328 (3.4%) |
| Maternal Education level n (%) | ||
| Less than high school | 3793 (38.7%) | 1038 (10.6%) |
| High school graduate | 3990 (40.7%) | 3460 (35.3%) |
| Greater than high school | 1894 (19.3%) | 5215 (53.2%) |
| Maternal Age n (%) | ||
| Less than 18 years | 932 (9.5%) | 240 (2.5%) |
| 18–24 years | 5046 (51.5%) | 3647 (37.2%) |
| 25 years and older | 3817 (39.0%) | 5907 (60.3%) |
| Leading Emergency Department Discharge Diagnosis by ICD-9 Code (for last ED visit) | ||
| First | Unspecified Otitis Media (ICD-9:382.9) n= 662 (8.4%) | Unspecified Otis Media (ICD-9: 382.9) n= 373 (7.3%) |
| Second | Fever (ICD-9: 780.6) n=379 (4.8%) | Fever (ICD-9: 780.6) n=250 (4.9%) |
| Third | Upper Respiratory Infection (ICD-9: 465.9)n=373 (4.8%) | Upper Respiratory Infection (ICD-9: 465.9) n=184 (3.6%) |
| Emergency Department Visit Type for Last ED Visit n (%) | ||
| Diagnostic Categories | n=7830 | n=5100 |
| Illness | 3355 (42.9) | 1973 (38.7) |
| Injury | 2197 (28.1) | 1621 (31.8) |
| Other | 2086 (26.6) | 1429 (28.0) |
| Poisoning | 120 (1.5) | 60 (1.2) |
| Psychiatric | 70 (0.9) | 17 (0.3) |
Controls
There were a total of 594 639 live births in Utah between the years 1989 and 2002, from which 9795 population-based controls matched on date of birth were randomly selected after successful linkage to the driver license database. Compared with cases, a higher percentage of control mothers had greater than a high school education and were 25 years or older. (Table I).
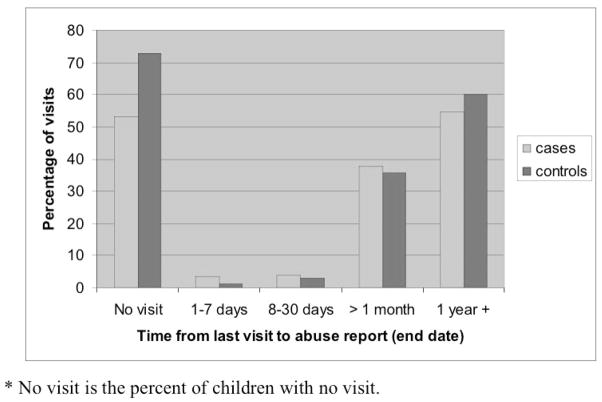
Cases and controls with an ED visit
The majority of cases (53.3%) and controls (73.0%) had no ED visit. The median number of visits among those children who were seen in the ED was 1.0 (IQR: 1.0, 1.0) for cases and 1.0 for controls (IQR: 1.0, 1.0). The percent of ED visits differed statistically between cases and controls at 7 days (3.6% versus 1.1% respectively, p < 0.001) and at one month (4.0% versus 3.0% respectively, p < 0.05); however, this represented only 6.4% of all visits for cases and controls combined to the ED. The majority of ED visits occurred > 1 month from the diagnosis of abuse or end date (Figure). Payer information was examined for each child who had an ED visit. Cases were more likely than controls to be uninsured or have government insurance (59.0% versus 24.1%, respectively, p< 0.001).
Figure 1.
A comparison of the distribution of ED visits, by percentage, between cases and controls from the start of the study to diagnosis of abuse or end date.
Type of ED visits by ICD-9 discharge data
Table I shows that the leading three types of discharge diagnoses from ED visits did not differ importantly between the cases and controls. When grouped by visit category, controls (31.8%) were more likely to have been seen in the ED setting for injury than cases (28.1%) (p < 0.001) compared with all other visit categories. In addition, when analyzed separately by specific abuse type, children who were victims of neglect had a slightly lower chance of an injury visit (RR = 0.8, 95% CI: 0.7, 0.9), and children who were victims of physical abuse had an equal risk of an injury visit (RR = 0.9, 95% CI: 0.8, 1.1) compared with the general population. Children who went on to be supported for sexual abuse did have more psychiatric visits than controls (RR = 3.8, 95% CI: 1.9, 7.7) which represented a difference of 1.3% of visits in cases and 0.3% of visits in controls.
Rates of ED use
Overall rates of ED use
The crude rate of ED visits for cases was 8.2 visits per 10 000 days of exposure (95% CI: 8.0, 8.3) compared with a rate of 3.9 ED visits per 10 000 days of exposure (95% CI: 3.7, 4.0) for age-matched controls (Table II). In the negative binomial model, cases were almost twice as likely than the general population (aRR = 1.8, 95% CI: 1.5, 1.8) to have had a prior ED visit, controlling for sex, race, maternal age and maternal educational level. When only cases in which one parent had a valid driver license were included in the analysis, the adjusted rate ratio (aRR=1.7, 95% CI: 1.5, 1.8) remained similar. The rate of ED visits in the 7 days prior to the report of abuse was low in both cases [0.17 (95% CI: 0.15, 0.20)] and controls [0.03 (95% CI: 0.02, 0.04)]. Among those who made a visit to the ED, cases and controls with commercial insurance had a similar ED visit rate (Rate ratio = 1.1, 95% CI: 1.0, 1.1). Cases with government or no insurance had a slightly higher rate of ED visits than similarly insured controls (Rate ratio = 1.2, 95% CI: 1.1, 1.2).
Table II.
Number of visits and crude rates of emergency department visits per 10 000 exposure days prior to abuse diagnosis (end date).
| All Children | Cases | Controls | p-value |
|---|---|---|---|
| Number (%) with prior visit | 4575 (46.7%) | 2647 (27.0%) | p<0.0001 |
| Range of prior visits | 1 – 30 | 1–17 | |
| Number of Prior visits (Median, Q1, Q2) | 1 (1,1) | 1 (1,1) | |
| Days between ED visit and diagnosis of abuse/end date (Median, IQR) | 410 (164, 725) | 469 (210, 773) | p<0.0001 |
| Number (%) seen within 7 days of diagnosis of abuse/end date for those with ED visit | 164 (3.6%) | 30 (1.1%) | |
| Rate with 95% confidence interval | 8.2 (8.0–8.3) | 3.9 (3.7–4.0) |
Rates of ED use by type of abuse
Rates of ED use were examined by type of abuse documented in the DCFS report. Neglect and domestic violence exposure had the highest rate of ED visits (9.6 visits per 10 000 days). Table III shows that sexual abuse had the lowest rate of ED visits (5.1 visits per 10 000 days) compared with other abuse types. Rates of ED use did not differ significantly by type of abuse among the cases (negative binomial test, p= 0.1).
DISCUSSION
This study has three major findings. First, most children with supported abuse are not seen in the ED prior to the diagnosis of abuse. Specifically, although there is a two times greater number of visits in cases than in controls, this only changes the visit rate from a median of one to two visits prior to the diagnosis of abuse. In addition this difference in ED visits decreases even further when stratified by insurance status. Second, most visits occur one month or more prior to the finding of abuse. Third, the diagnostic spectrum seen in those who visit the ED are similar.
In our study, children with supported child abuse had almost two times the rate of ED visits compared with population-based controls. This increased utilization was seen among all abuse types. However, when rates among those who visited the ED were examined more closely, there was an elevated visit rate in both cases and controls among those with government or no insurance, while all children with commercial insurance had similar visit rates. Thus, the higher visit rate among children who were abused are likely multi-factorial and may include overlapping social indicators that have been shown to predict increased ED use for both primary care problems(19–21) and child maltreatment(22) such as poverty, membership of a racial or ethnic minority group, and insurance status.(23–27)
Among all children with ED visits, most occurred > 1 month from the abuse (end date) report. We did find that the timing of ED visits differed statistically between cases and controls. Rates of visit were higher for cases in the 7 days preceding the report, but were low for both cases and controls. Interestingly, the majority of cases and controls had no ED visit and most cases and controls had only one visit. Thus, although the timing of visits differs statistically between the two groups, the difference is not adequate to identify the majority of children who will go on to have an abuse finding.
Finally, there was no unique spectrum of diagnoses that differentiated children who went on to have an abuse diagnosis from those who did not. The top six ED discharge diagnoses were similar both between cases and controls and among abuse types. Children who went on to have supported neglect or physical abuse did not have more injury visits than controls. This finding differs from previous studies which have reported that children at risk for abuse present more frequently to the ED with specific complaints such as injuries,(28) chronic pain,(29) and headaches,(30) among others. Consequently, this study did not find any “red flags” from either the frequency or pattern of a child’s ED visits, which would allow early identification of children at risk for abuse by the emergency department physician.
The ED is a setting where children who will experience abuse may have contact with the healthcare system prior to the abuse being detected. This has led to the suggestion that the ED is an appropriate setting to screen for child abuse. (11) Although we found that children who go on to experience abuse are seen more frequently in the ED than population based controls, the majority of case children in our study who had any ED visit, had one visit or less and did not have a pattern of visits that would distinguish them from the general ED patient population. Therefore, these markers would not allow one to choose a “high risk” population for screening. Our inability to identify a high risk population in children presenting to the ED, however, does not imply that health care providers in the ED setting should ignore signs of abuse. Instead, health care providers must maintain high vigilance in all children presenting to the ED for possible abuse. Future prevention programs targeted at abuse should be available to families of all children seen in an ED.
There were several limitations to our study. First, it is possible that this study may have under-ascertained abused children because we studied only children who had identification of abuse that resulted in DCFS involvement. Thus, some of the children in the population-based controls may have experienced unreported or non-supported abuse leading to misclassification bias. In addition, fatalities not classified as abuse would not have resulted in DCFS involvement. If either of these occurred, it would have tended to decrease the observed difference between cases and controls in ED utilization. Second, the administrative statewide databases include the discharge diagnoses. If the presenting complaint and discharge diagnosis differ significantly by case status, detailed medical patterns that may be associated with abuse could have been missed. Third, we may have introduced bias by including only cases and controls whose parents had a Utah driver license. However, an analysis performed to detect this bias (using the sub-group of cases who had a parent with a valid Utah driver license and compared with cases whose parents did not have a valid driver license) did not find substantive differences. Fourth, Utah is one of five states to define exposure to domestic violence as child abuse which may limit the generalizability of this study. Finally, our only proxy for socioeconomic status was insurance status. This is an imperfect proxy and was available only for those children with an ED visit.
This study has several strengths. First, the use of probabilistic linkage enabled the evaluation of facility-based health care statewide, permitting us to study patients who may have been seen in more than one institution. Second, we included a population-based control group matched to each case by day of birth, assuring similar exposure time. This allowed us to calculate rates of ED use in both the general pediatric population of Utah and for the separate subtypes of abuse. Third, our study examined all types of child abuse. Fourth, by linking our databases to the driver license database, we were able to establish residency of the cases and controls in the state of Utah during the time of the study. Finally, all of the child abuse cases for the state of Utah are handled through the State of Utah Department of Child and Family Services. We therefore have population complete databases and access to all of the cases supported in our state.
In summary, children with supported child abuse have a higher use of the emergency department, prior to diagnosis of abuse, when compared with the general pediatric population. However, neither the frequency of emergency department use nor the pattern of diagnoses offers sufficient specificity to be useful markers of future abuse. ED health care providers must maintain a high level of vigilance for the possibility of abuse in all children.
Table 3.
Emergency department visits by type of child abuse compared to population controls where N = number of children
| # Previous ED Visits | Physical Abuse Only N = 777 | Sexual Abuse Only N = 1486 | Neglect Only N = 2145 | Emotional Abuse Only N= 474 | Domestic Violence Only N= 3111 | Multiple Subtypes of Abuse N= 1385 | Controls N= 9795 |
|---|---|---|---|---|---|---|---|
| 0 | 417 (53.7%) | 831 (55.9%) | 1103 (51.4%) | 255 (53.8%) | 1652 (53.1%) | 748 (54.1%) | 7148 (73.0%) |
| 1 | 286 (36.8%) | 590 (39.7%) | 774 (36.1%) | 180 (38.0%) | 1030 (33.1%) | 515 (37.2%) | 2237 (22.8%) |
| 2 | 37 (4.8%) | 29 (2.0%) | 103 (4.8%) | 15 (3.2%) | 180 (5.8%) | 45 (3.3%) | 228 (2.3%) |
| 3 | 17 (2.2%) | 9 (0.6%) | 64 (3.0%) | 8 (1.7%) | 91 (2.9%) | 26 (1.9%) | 80 (0.8%) |
| ≥4 | 20 (2.6%) | 27 (1.8%) | 101 (4.7%) | 16 (3.4%) | 158 (5.1%) | 51 (3.7%) | 102 (1.0%) |
| Max # visits | 13 | 18 | 29 | 17 | 16 | 30 | 17 |
| Rate of visits per 10 000 days exposed(95% CI) | 7.1 (9.2, 10.0) | 5.1 (6.4, 7.9) | 9.6 (9.2, 10.1) | 7.1 (6.5, 7.7) | 9.6 (4.8, 5.5) | 7.6 (7.2, 8.1) | 3.9 (3.7, 4.0) |
Acknowledgments
This study was partially presented at the national Pediatric Academic Societies/American Academy of Pediatrics meeting in Washington DC, May 2005. This study was supported by a National Institutes of Child Health and Human Development (NICHD) grant for Dr. Guenther (K23HD043145). The[H1] authors declare no potential conflicts of interest.
Appendix 1
Definitions from the State of Utah DCFS, taken from the U.S. Department of Health and Human Services National Clearinghouse on Child Abuse and Neglect1 for each of the abuse types, with the exception of exposure to intimate partner violence, as follows:
Physical abuse: “Any non-accidental physical injury to the child, and can include striking, kicking, burning, or biting the child, or any action that results in a physical impairment of the child.”
Sexual abuse: “The employment, use, persuasion, inducement, enticement, or coercion of any child to engage in, or assist any other person to engage in, any sexually explicit conduct or simulation of such conduct for the purpose of producing a visual depiction of such conduct; or the rape, and in cases of caretaker or interfamilial relationships, statutory rape, molestation, prostitution, or other form of sexual exploitation of children, or incest with children.”
Child neglect: “Acts of omission; specifically the failure of a parent or other person legally responsible for a child’s welfare to provide for the child’s basic needs and proper level of care with respect to food, clothing, shelter, hygiene, medical attention or supervision.
Emotional abuse: “Acts or omissions by the parents or other caregivers that have caused, or could cause, serious behavioral, cognitive, emotional, or mental disorders. In some cases of emotional abuse, the acts of parents or other caregivers alone, without any harm evident in the child’s behavior or condition, are sufficient to warrant DCFS intervention.”
Exposure to domestic violence
Under the Utah statute, “A person is guilty of child abuse if that person commits an act of intimate partner violence in the presence of a child” where “in the presence of a child” means either in the physical presence of a child, or having knowledge that a child is present and may see or hear an act of intimate partner violence.2
- 1. [Accessed August 10, 2005];National Clearinghouse on Child Abuse and Neglect Information: Children and Domestic Violence. Available at: http://nccanch.acf.hhs.gov.
- 2.Utah Legislature SB0076 2003
Appendix 2 Utah Statewide Databases
Utah DCFS Database
The DCFS data for 2001–2002 (n=19 005) compiled by the State of Utah Department of Human Services contains the records of all patients with a substantiated diagnosis of child abuse. Data include patient demographics and type of child abuse.
Birth Certificate
The birth certificate data were used from 1989 through 2002 (n=594 639) were obtained from the Utah Resource for Genetic Epidemiologic Research at the University of Utah. This database provided maternal age, race, and education.
Death Certificate
The death certificate data for 1999 through 2002 were obtained from the Utah Resource for Genetic Epidemiologic Research at the University of Utah.
Driver’s License Database
The driver’s license data from 1999 through 2002 (n=) were obtained from the Utah Resource for Genetic Epidemiologic Research at the University of Utah. This database provided maternal location of residence during the study period.
Emergency Department and Inpatient
Hospital emergency department (n=2 602 048) and inpatient discharge records (n=976 799) for the years 1999 through 2002 were acquired from the Utah Health Data Committee/Office of Healthcare Statistics. All licensed hospitals in Utah are mandated to report information on ED and inpatient discharges to the state. The ED database contains information on all patients who visited an ED, even if the patient was transferred, admitted as an inpatient or left against medical advice.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hoyert DL, Heron MP, Murphy SL, Kung HC. Deaths: Final data for 2003. Natl Vital Stat Rep. 2006;54:1–120. [PubMed] [Google Scholar]
- 2.Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281:621–6. doi: 10.1001/jama.281.7.621. [DOI] [PubMed] [Google Scholar]
- 3.Alexander R, Crabbe L, Sato Y, Smith W, Bennett T. Serial abuse in children who are shaken. Am J Dis Child. 1990;144:58–60. doi: 10.1001/archpedi.1990.02150250068033. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal I. Shaken baby syndrome. Postgrad Med J. 2002;78:732–5. doi: 10.1136/pmj.78.926.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feldman KW. Patterned abusive bruises of the buttocks and the pinnae. Pediatrics. 1992;90:633–6. [PubMed] [Google Scholar]
- 6.Hornor G. Physical abuse: Recognition and reporting. J Pediatr Health Care. 2005;19:4–11. doi: 10.1016/j.pedhc.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 7.King WK, Kiesel EL, Simon HK. Child abuse fatalities: are we missing opportunities for intervention? Pediatr Emerg Care. 2006;22:211–4. doi: 10.1097/01.pec.0000208180.94166.dd. [DOI] [PubMed] [Google Scholar]
- 8.Oral R, Blum KL, Johnson C. Fractures in young children: are physicians in the emergency department and orthopedic clinics adequately screening for possible abuse? Pediatr Emerg Care. 2003;19:148–53. doi: 10.1097/01.pec.0000081234.20228.33. [DOI] [PubMed] [Google Scholar]
- 9.Paradise JE, Bass J, Forman SD, Berkowitz J, Greenberg DB, Mehta K. Minimum criteria for reporting child abuse from health care settings. Del Med J. 1997;69:357–63. [PubMed] [Google Scholar]
- 10.Sugar NF, Taylor JA, Feldman KW. Bruises in infants and toddlers: those who don’t cruise rarely bruise. Puget Sound Pediatric Research Network. Arch Pediatr Adolesc Med. 1999;153:399–403. doi: 10.1001/archpedi.153.4.399. [DOI] [PubMed] [Google Scholar]
- 11.Olney DB. Patterns of presentation of abused children to the accident and emergency department. Arch Emerg Med. 1988;5:228–32. doi: 10.1136/emj.5.4.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krugman RD. Child abuse and neglect: critical first steps in response to a national emergency. The report of the US Advisory Board on Child Abuse and Neglect. Am J Dis Child. 1991;145:513–5. doi: 10.1001/archpedi.1991.02160050039008. [DOI] [PubMed] [Google Scholar]
- 13.International Classification of Diseases, 9th Revision Clinical Modification. 6. USA: Ingenix; 2007. [Google Scholar]
- 14.LinkSolv. [Last accessed March 29, 2008];Record Linkage Solution. 2006 http://www.codes2000forum.com/
- 15.Jaro MA. Probabilistic linkage of large public health data files. Stat Med. 1995;14:491–8. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 16.Dean JM, Vernon DD, Cook L, Nechodom P, Reading J, Suruda A. Probabilistic linkage of computerized ambulance and inpatient hospital discharge records: a potential tool for evaluation of emergency medical services. Ann Emerg Med. 2001;37:616–26. doi: 10.1067/mem.2001.115214. [DOI] [PubMed] [Google Scholar]
- 17.Cook LJ, Olson LM, Dean JM. Probabilistic record linkage: relationships between file sizes, identifiers and match weights. Methods Inf Med. 2001;40:196–203. [PubMed] [Google Scholar]
- 18.Census US. [Last accessed March 29, 2008];Census 2000 Data for the State of Utah. 2000 http://www.census.gov/census2000/states/ut.html.
- 19.Sills MR, Shetterly S, Xu S, Magid D, Kempe A. Association between parental depression and children’s health care use. Pediatrics. 2007;119:e829–36. doi: 10.1542/peds.2006-2399. [DOI] [PubMed] [Google Scholar]
- 20.Babin SM, Burkom HS, Holtry RS, Tabernero NR, Stokes LD, Davies-Cole JO, et al. Pediatric patient asthma-related emergency department visits and admissions in Washington, DC, from 2001–2004, and associations with air quality, socio-economic status and age group. Environ Health. 2007;6:9. doi: 10.1186/1476-069X-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mistry RD, Hoffmann RG, Yauck JS, Brousseau DC. Association between parental and childhood emergency department utilization. Pediatrics. 2005;115:e147–51. doi: 10.1542/peds.2004-1798. [DOI] [PubMed] [Google Scholar]
- 22.Connell CM, Bergeron N, Katz KH, Saunders L, Tebes JK. Re-referral to child protective services: the influence of child, family, and case characteristics on risk status. Child Abuse Negl. 2007;31:573–88. doi: 10.1016/j.chiabu.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Cots F, Castells X, Garcia O, Riu M, Felipe A, Vall O. Impact of immigration on the cost of emergency visits in Barcelona (Spain) BMC Health Serv Res. 2007;7:9. doi: 10.1186/1472-6963-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinreb L, Goldberg R, Bassuk E, Perloff J. Determinants of health and service use patterns in homeless and low-income housed children. Pediatrics. 1998;102:554–62. doi: 10.1542/peds.102.3.554. [DOI] [PubMed] [Google Scholar]
- 25.Stingone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006;97:244–50. doi: 10.1016/S1081-1206(10)60021-X. [DOI] [PubMed] [Google Scholar]
- 26.Michelen W, Martinez J, Lee A, Wheeler DP. Reducing frequent flyer emergency department visits. J Health Care Poor Underserved. 2006;17(1 Suppl):59–69. doi: 10.1353/hpu.2006.0010. [DOI] [PubMed] [Google Scholar]
- 27.Laursen B. Injury patterns in children with frequent emergency department visits. Emerg Med J. 2006;23:59–60. doi: 10.1136/emj.2004.021469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spivey MI, Schnitzer PG, Kruse RL, Slusher P, Jaffe DM. Association of Injury Visits in Children and Child Maltreatment Reports. J Emerg Med. 2008 Apr 8; doi: 10.1016/j.jemermed.2007.07.025. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Arnow BA. Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization. J Clin Psychiatry. 2004;65(Suppl 12):10–5. [PubMed] [Google Scholar]
- 30.Arnow BA, Hart S, Hayward C, Dea R, Barr Taylor C. Severity of child maltreatment, pain complaints and medical utilization among women. J Psychiatr Res. 2000;34:413–21. doi: 10.1016/s0022-3956(00)00037-6. [DOI] [PubMed] [Google Scholar]