Abstract
Objective:
To critically assess original research addressing the effect of creatine supplementation on exercise heat tolerance and hydration status.
Data Sources:
We searched the electronic databases PubMed, Scopus, Web of Science, SPORTDiscus, and Rehabilitation & Physical Medicine, without date limitations, for the following key words: creatine, exercise, thermoregulation, dehydration, hyperthermia, heat tolerance, exertional heat illnesses, and renal function. Our goal was to identify randomized clinical trials investigating the effect of creatine supplementation on hydration status and thermoregulation. Citations from related articles also were identified and retrieved.
Data Synthesis:
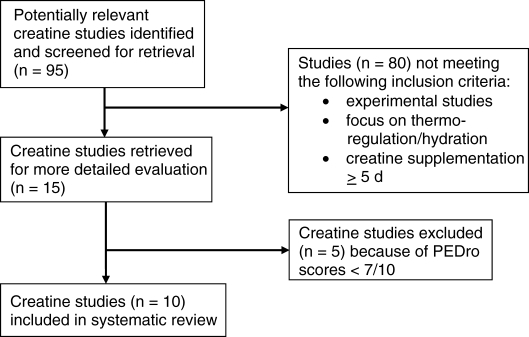
Original research was reviewed using the Physiotherapy Evidence Database (PEDro) Scale. One author initially screened all articles. Fifteen of 95 articles examined the effects of creatine on thermoregulation or hydration status (or both). Two independent reviewers then reviewed these articles. Ten studies were selected on the basis of inclusion and exclusion criteria. The PEDro scores for the 10 studies ranged from 7 to 10 points (maximum possible score = 10 points).
Conclusions:
No evidence supports the concept that creatine supplementation either hinders the body's ability to dissipate heat or negatively affects the athlete's body fluid balance. Controlled experimental trials of athletes exercising in the heat resulted in no adverse effects from creatine supplementation at recommended dosages.
Keywords: thermoregulation, dehydration, hypohydration, exertional heat illness, renal function
Key Points.
When recommended amounts were consumed, creatine supplementation did not appear to hinder the body's ability to dissipate heat or negatively affect body fluid balance.
Future researchers should evaluate the use of creatine during longer supplementation periods, exercise bouts that simulate games and practices, and more controlled field studies.
Many athletes have turned to nutritional supplements marketed as ergogenic aids to maximize athletic performance. Creatine is a naturally occurring element in the diet; it is also synthesized within the body, primarily by the liver.1 As a dietary supplement, creatine monohydrate is believed to enhance the resynthesis of adenosine triphosphate and to improve performance in short bouts of exercise. Creatine supplementation has been used by athletes for nearly 20 years, but speculation remains regarding its efficacy, as well as its potential side effects.
When creatine first gained media attention, many adverse events were attributed to its use, including the deaths of 3 National Collegiate Athletic Association wrestlers in 1997.2 Authors2–4 from several media reports on these fatalities and scientific review papers speculated on the possibility that creatine was a key factor leading to death. However, autopsy results determined that exertional heat stroke, not creatine, was responsible for these deaths.5 Creatine has also been implicated as possibly contributing to the deaths of several football players in recent years,6 but this suspicion has never been confirmed. Speculation that creatine may have influenced exertional heat stroke has resulted in an examination of its role in exercise heat intolerance.
Aside from the aforementioned media reports on creatine, most anecdotal reports of side effects have described muscle cramping or gastrointestinal distress.1 Other side effects potentially linked to creatine use include but are not limited to renal damage, susceptibility to muscle strains or cramps, and impairment of thermoregulation.1,3 The main concern involves its potential impairment of exercise heat tolerance and hydration status. These anecdotal reports, however, were never supported by clinical evidence.
After the media reports in the late 1990s, the American College of Sports Medicine sponsored a roundtable discussion entitled “The Physiological and Health Effects of Oral Creatine Supplementation.”1 Roundtable participants advised athletes to avoid creatine supplementation if they were “wishing to control weight” or “subjected to strenuous exercise and/or hot environments.”1 They also recommended avoiding high dosages of creatine “during periods of increased thermal stress, such as sports activities performed under high ambient temperature/humidity conditions.” These recommendations stemmed from the premise that supplementing with creatine can lead to a potentially impaired thermoregulation and altered fluid balance. To our knowledge, however, no scientific evidence existed at that time to support or refute these statements or any of the anecdotally reported side effects.
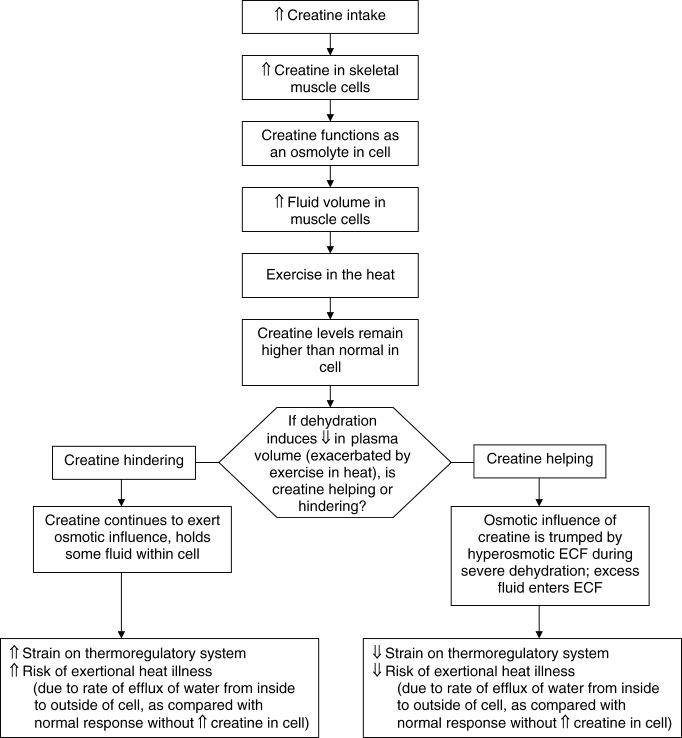
Theoretically, creatine uptake by the muscles results in an increase in fluid volume within skeletal muscle cells. Whether this increase helps, hinders, or does not influence thermoregulation has not been determined (Figure 1). Yet as a result of anecdotal reports and precautions regarding the potential detrimental effects of creatine supplementation, various researchers7–22 investigated the effects of creatine on hydration status and thermoregulation. The studies varied in methods, such as creatine dosages, exercise protocols, and ambient temperatures, making it difficult for a clinician to determine the best evidence-based clinical practice regarding creatine supplementation for athletes. Therefore, the purpose of our systematic review was to assess the evidence regarding the influence of creatine supplementation on exercise heat tolerance and hydration status.
Figure 1. Does creatine hinder or help? Hypothetical considerations for influence of creatine on hydration status during rest and exercise in the heat. ECF indicates extracellular fluid.
Methods
Data Sources
We searched the following electronic databases with no date limitations: PubMed, Scopus or Web of Science, SPORTDiscus, and Rehabilitation & Physical Medicine. These databases were searched in April 2007 using the following key words: creatine, exercise, thermoregulation, dehydration, hyperthermia, heat tolerance, exertional heat illnesses, and renal function. The search included human studies in English and Spanish but excluded articles pertaining to surgery and alcoholism.
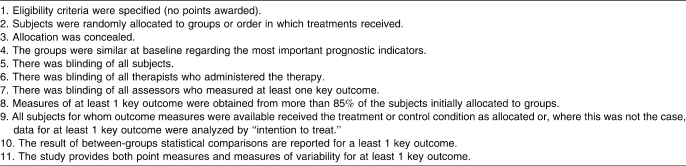
Research articles pertaining to the effects of creatine supplementation on hydration status and thermoregulation were identified. All controlled clinical trials were initially examined. References from these articles and references from past review articles were then cross-referenced to identify additional articles for possible inclusion. Inclusion criteria were experimental studies with washout periods of 28 or more days (crossover experimental design) and dependent variable(s) of hydration or thermoregulatory status with the purpose related to evaluating the effects of creatine supplementation on hydration or thermoregulation or both. Only studies with physically active male or female participants were included. Articles were excluded if they were reviews, addressed nonactive individuals, or used a creatine dosage that was less than 2 g · d−1 or that was administered for fewer than 5 days. Articles receiving a score of less than 7 on the Physiotherapy Evidence Database Scale (PEDro) Scale23 (Table 1) were also excluded, because a lower score indicated that internal validity or blinding of participants was lacking.
Table 1.
Physiotherapy Evidence Database (PEDro) Scale23
Quality Assessment
Authors of 15 of the 95 identified articles examined the effects of creatine on thermoregulatory measures or hydration measures or both. After meeting our inclusion criteria, these 15 articles were reviewed by 2 independent reviewers using the PEDro Scale23 (Figure 2). This scale consists of a checklist to determine 2 aspects of a study's quality: (1) the internal validity of the trial and (2) whether information is sufficient to interpret the results.23 The PEDro Scale contains 11 items, 10 of which contribute to the score (Table 1). Each yes response is worth 1 point, whereas a no response is worth 0 points, for a maximum possible of 10 points. The PEDro Scale or variations of this scale have been used in other systematic reviews as a means of determining the quality of controlled trials.24–27
Figure 2. Criteria for selection of articles for review.
The PEDro scores for the 15 articles ranged from 3 to 10 points. Scores were recorded, and the 2 investigators met to review any discrepancies. The interrater agreement for the PEDro scores of the 2 investigators was initially moderate28 (κ = 0.530); however, after the investigators reviewed the scores, they reached full consensus (κ = 1.00). Five articles were excluded because of their low PEDro scores (less than 7 of 10 points), resulting from lack of participant blinding or lack of focus on thermoregulatory measures. The PEDro scores for the 10 selected articles ranged from 7 to 10 points.
Statistical Analysis
We quantified the effect of creatine ingestion on thermoregulation by performing a meta-analysis of the body temperature data using RevMan software (version 5.0; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). RevMan was used for calculating the χ2 distribution to determine heterogeneity and to test for overall effect, weighted averages, mean differences, effect estimates, and 95% confidence intervals. Weighted percentages were based on the studies' sample sizes. We used SPSS software (version 16.0; SPSS Inc, Chicago, IL) to determine interrater agreement for the PEDro scores.
Results
Data Synthesis
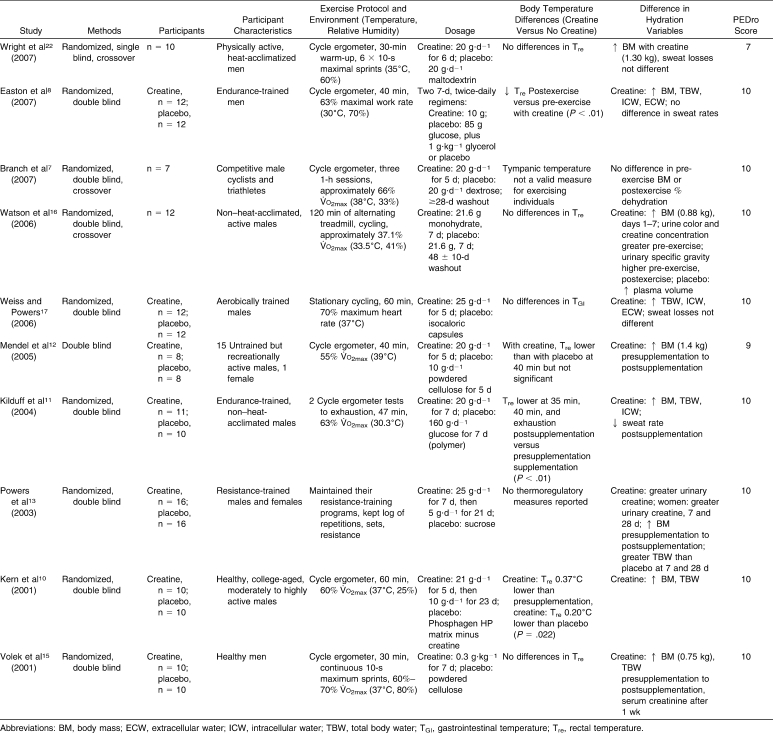
The focus of our search was to determine what differences, if any, were present between participants supplementing with creatine and those supplementing with placebo with regard to the following dependent variables: a valid body temperature assessment (eg, rectal [Tre] temperature or gastrointestinal [TGI]), body mass, total body water (TBW), intracellular water (ICW), extracellular water (ECW), heart rate, and urinary and plasma measures (Table 2).
Table 2.
Studies Investigating the Influence of Creatine on Hydration Status and Exercise Heat Tolerance
Wright et al22 examined the effects of 6 days of creatine loading on thermoregulation in a hot, humid environment (35°C, 60% relative humidity) during a sprint performance on a cycle ergometer. Creatine loading resulted in increased body mass (+1.30 kg) compared with the placebo condition (P < .05). Although the exercise bout resulted in increased core temperature, loss of body water, and a change in plasma volume, these measures were not different between the creatine and placebo conditions.22
Easton et al8 investigated the effects of combined creatine and glycerol supplementation on responses to exercise in the heat. Although these authors looked at combining creatine with glycerol supplementation, we focused on the interaction effects between the creatine and placebo conditions only. Body mass, TBW, ICW, and ECW were increased compared with placebo. However, no differences were noted in total sweat losses between the conditions. After supplementation, Tre was lower during exercise in the creatine condition (P < .01).
Branch et al7 examined the effects of creatine supplementation on competitive male cyclists and triathletes while cycling in the heat (38.7°C). No differences were seen between the creatine and placebo groups for heart rate or rating of perceived exertion (RPE). Postexercise, plasma volume decreased in the baseline and placebo conditions compared with the creatine condition (P = .013). Fluid consumed, exercise-induced dehydration, and pre-exercise and postexercise body mass were not different between conditions. Branch et al7 used tympanic temperature, which is not a valid measure of body temperature.29
Watson el al16 examined the effects of 1 week of creatine supplementation on hydration status, thermoregulation, and incidence of heat illness in dehydrated men exercising in a hot environment. Body mass and sweat losses during exercise were not different between conditions; however, an interaction was demonstrated in the body mass change from day 1 to day 7 of creatine supplementation (P = .015). Urine specific gravity was higher for the creatine group before (P = .030) dehydration and pre-exercise (P = .004) and postexercise (P = .009) heat tolerance test. Compared with placebo, plasma osmolality was higher during creatine supplementation before (P = .032) and after (P = .015) dehydration, as well as 20 minutes into recovery (P = .008).
The investigation of Weiss and Powers17 consisted of a 5-day supplementation period followed by a 60-minute bout of exercise in a warm environment. Aerobically trained males exhibited no differences in heart rate or sweat losses. Group × day interactions were observed for TBW (P = .004), ICW (P = .046), and ECW (P = .005), with the creatine group experiencing an increase in each of the 3 body water volumes. No TGI differences were found between groups (P = .87).
Mendel et al12 investigated the effects of creatine on thermoregulatory responses during exercise in a hot environment (39°C). Five days of creatine supplementation resulted in a 1.4-kg increase in body mass postsupplementation (P = .013). Although not different, Tre was lower at 40 minutes of exercise for the creatine group.
Kilduff et al11 examined the effects of creatine on thermoregulatory, cardiovascular, and metabolic responses during exercise in the heat in endurance-trained males. Body mass, TBW, and ICW increased in the creatine group. After supplementation, heart rate was lower in the creatine group from 35 minutes of exercise until exhaustion (P = .044). Compared with presupplementation, postsupplementation Tre was lower at 35 minutes and 40 minutes and at exhaustion (P = .012). Sweat rate also was reduced after creatine supplementation (32.3 ± 7.0 mL · min−1 versus 28.2 ± 3.9 mL · min−1, P = .02).
Powers et al13 examined the effects of 28 days of creatine supplementation on fluid distribution. The creatine group had greater body mass from presupplementation to day 28 (P = .44). Compared with placebo, the creatine group had greater TBW volume on days 7 and 28 (P = .027), with no differences in ECW and ICW (P = .366).
Kern et al10 examined hydration status and indicators of heat tolerance after 28 days of creatine supplementation. In the creatine condition, body mass (P = .034) and TBW increased (P = .050). Compared with presupplementation, postsupplementation Tre for the creatine group was 0.37°C lower; compared with the placebo group, postsupplementation Tre was 0.20°C lower (P = .022 for differences from presupplementation to postsupplementation between the creatine and placebo groups). No differences were noted in heart rate responses to exercise in the heat between conditions.
Volek et al15 provided participants with 7 days of creatine supplementation. Body mass increased 1 week postsupplementation (0.75 kg, P ≤ .05). Body mass losses and sweat rate during 35 minutes of exercise in the heat (38°C) were not different between groups (P > .05). Plasma volume changes, Tre, heart rate, and RPE were not different between groups (P > .05). Urinary volumes over 24 hours tended to be greater for the creatine group, but were only significantly greater than placebo on day 3 of supplementation (P < .05).
Meta-Analysis Test Outcomes
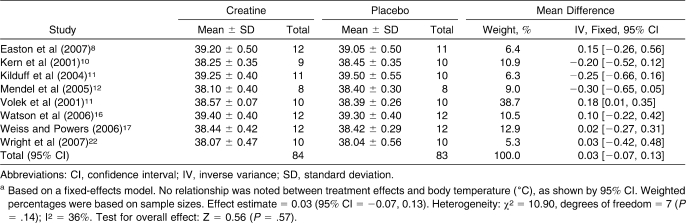
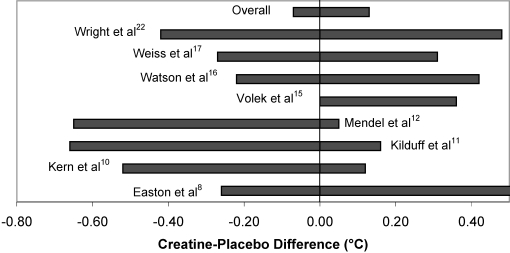
The test for heterogeneity was not significant: χ27 = 10.9, P = .14. Using a fixed-effects inverse variance analysis model, the test for overall effect was not significant (Z = 0.56, P = .57). With the 8 studies (n = 167) included in the meta-analysis, the effect estimate = 0.03 (95% confidence interval = −0.07, 0.13). Weighted averages, mean differences, and 95% confidence intervals are reported in Table 3 and Figure 3.
Table 3.
Differences in Body Temperature (°C) Between Creatine Versus No Creatinea
Figure 3. Differences in body temperature between creatine versus no creatine as described in Table 3. Based on a fixed-effects model, no relationship was noted between treatment effects and body temperature, as shown by 95% confidence intervals. Weighted percentages were based on sample sizes. Effect estimate = 0.03 (95% confidence interval = 20.07, 0.13).
Discussion
Despite anecdotal reports of creatine side effects in athletes exercising in the heat, none of the 10 studies7,8,10–13,15–17,22 showed detriments in thermoregulatory or hydration variables, including body temperature regulation, percentage of dehydration, urinary hydration measures, plasma volume, or sweat losses (Table 2).
Participant Characteristics, Exercise Protocols, Environmental Conditions, and Creatine Dosing
The similarities and differences among participant characteristics, exercise protocols, and environmental conditions are illustrated in Table 2. Variations in methods did not affect the influence of creatine supplementation.
The amount of creatine consumed was similar among trials (20–25 g · d−1), whereas the supplementation duration varied (5–28 days). Despite variations in dosages, the results of the 10 studies were similar with regard to changes in body mass and body temperature. None of the studies included in this review (Table 2) involved creatine supplementation for longer than 28 days. One of the greatest concerns about creatine use is that few authors have examined its long-term effects. Although Kreider et al20 examined the effects of creatine dosages over a 21-month period, they did not focus on markers of hydration or thermoregulation. Further studies involving long-term creatine supplementation and its effects on hydration and thermoregulation are necessary to determine possible adverse effects.
Effects on Body Temperature
Six of the 10 groups reported no differences between creatine and placebo in body temperature while exercising in the heat (Table 3). However, one group29 measured tympanic temperature, which was mentioned as a limitation of the study because it does not validly represent central body temperature in exercising individuals. In 3 of the 10 studies,8,10,11 Tre was lower after creatine supplementation. Although the finding was not significant, one group12 also reported lower Tre for creatine (compared with placebo) after 40 minutes of exercise. The decreased body temperature in these studies could be attributed to factors such as increases in body mass and TBW, because the findings were similar (Table 2), but how an increase in these measures would attenuate a rise in body temperature is unclear. None of these authors8,10,11 found an increase in sweat rate, which might have improved thermoregulation.
These results indicate that creatine supplementation was not a detriment to thermoregulation while exercising in the heat when supplementation took place over the course of 5 to 28 days. Many researchers1–4,6 have questioned whether creatine supplementation hinders thermoregulation and predisposes an athlete to exertional heat stroke (Figure 1). However, this review demonstrates no differences in body temperature with creatine supplementation, and some groups8,10,11 even showed that creatine attenuated the rise in body temperature during exercise in the heat. During severe dehydration, the osmotic influence of creatine could be trumped by hyperosmotic extracellular fluid (ECF), resulting in excess fluid entering the ECF and possibly decreasing the strain on thermoregulation, as depicted in Figure 1.
Effects on Hydration Measures
Previous authors21 have found that acute creatine ingestion elevated TBW and ICF but had no effect on ECW after 3 days of supplementation. These results are similar to those of some of the reviewed studies, in which authors reported increases in TBW,8,10,11,13,15,17 increases in ICW and ECW,8,17 and increases in ICW but not ECW.11 Although other researchers found no differences in sweat rate with creatine supplementation,17,22 only one group11 noted a decrease in sweat rate with creatine supplementation.
The most common effect of creatine supplementation found in the literature has been a change in body mass, but this finding does not seem to alter exercise sweat rates.7,8,14,17,22 Investigators on 9 of the 10 studies in this review reported an increase in body mass as a result of creatine supplementation.8,10–13,15–17,22 Changes in total body mass could be detrimental in sports that depend on specific body weights (ie, wrestling, gymnastics). More importantly, changes in body mass and TBW have been the cause of reservations regarding thermoregulation1 (Figure 1). Several authors8,11,17,21 have found increases in ICW as a result of creatine supplementation; none of these resulted in signs or symptoms of heat illness or impaired thermoregulation. Further, it has been suggested8,10,11 that these increases in TBW and ICW might actually assist in maintaining or improving thermoregulation. Results from earlier researchers21 noted osmotic fluid shifts within as few as 3 days of creatine supplementation. However, Casa et al30 found that after 10 days of supplementation, creatine did not alter fluid distribution or promote an osmotic fluid shift between fluid compartments. Furthermore, authors18 investigating National Collegiate Athletic Association Division I-A college football players found that the incidence of cramping or injury for creatine users was lower than or proportional to that of non–creatine users. The different TBW, ICW, and ECW changes can be attributed to variations in the amount and duration of creatine dosages as well as to differences in methods (Table 2). The variations in hydration outcome measures made it difficult to identify the influence of creatine supplementation on fluid balance; however, based on these studies, creatine does not seem to impair hydration status or thermoregulation. Furthermore, the findings from the objective approach used in this systematic review seem to reiterate the findings reported in a recent review on this topic.31
Pedro Scale
We selected the PEDro Scale to assess the quality of relevant articles. The PEDro Scale is intended to identify controlled, unbiased experimental trials to ensure internal validity and to determine if the results of the research can be interpreted. One can conclude that the higher the PEDro score a study received, the better the study quality and the greater the likelihood that the results are a valid estimate of the truth.24 The scores we generated were relatively high in comparison with PEDro scores of other systematic reviews.24,27 This result could be attributed to (1) a recent increase in higher-quality, randomized, controlled trials in the areas of thermoregulation and hydration, as well as (2) 3 points in the scale reflecting blinding of participants. Authors of controlled studies24,27 in other systematic reviews may have not been able to blind their participants or researchers to the treatment given.
Conclusions
No substantial evidence currently exists showing that creatine supplementation hinders the body's ability to dissipate heat or body fluid balance when appropriate doses are consumed. Controlled experimental trials of athletes exercising in the heat over a short period of time resulted in no adverse effects from creatine supplementation. Future researchers should include longer supplementation periods, exercise bouts that simulate a game or practice situation (ie, greater than 60 minutes in duration), and more controlled field studies.
As clinicians working with athletes on a daily basis, athletic trainers, other allied health professionals, and physicians must ask themselves, “What underlies the anecdotal reports of adverse effects from creatine?” As clinicians, we should be asking how to connect experimental trials and real-life situations. Allied health professionals should use evidence-based medicine to determine clinical applications.
Footnotes
Rebecca M. Lopez, MS, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Douglas J. Casa, PhD, ATC, FNATA, FACSM, contributed to conception and design, analysis and interpretation of the data, and critical revision and final approval of the article. Brendon P. McDermott, MS, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Matthew S. Ganio, MS, contributed to conception and design, analysis and interpretation of the data, and critical revision and final approval of the article. Lawrence E. Armstrong, PhD, FACSM, and Carl M. Maresh, PhD, FACSM, contributed to analysis and interpretation of the data and critical revision and final approval of the article.
References
- 1.Terjung R.L, Clarkson P, Eichner E.R, et al. American College of Sports Medicine roundtable: the physiological and health effects of oral creatine supplementation. Med Sci Sports Exerc. 2000;32(3):706–717. doi: 10.1097/00005768-200003000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Naughton J. NCAA and federal agencies investigate the death of 3 college wrestlers. Chron Higher Educ. 2007. http://chronicle.com/data/articles.dir/eguid-44.dir/18eguide.htm. Published January 9, 1998. Accessed April 8,
- 3.Bailes J.E, Cantu R.C, Day A.L. The neurosurgeon in sport: awareness of the risks of heatstroke and dietary supplements. Neurosurg Online. 2002;51:283–288. http://www.neurosurgery-online.com/pt/re/neurosurg/abstract.00006123-200208000-00002.htmjsessionidHhPKhGPmhMNLgqwJqM3Fpp1rhy8vGGJKlZ0L4NL7JZf6rrxZMyw817599563931811956298091-1. Accessed July 11, 2007. [PubMed] [Google Scholar]
- 4.Field J, Plona K. Wrestler's death evokes grief, spurs training reform. Michigan Daily Online. 2007. http://www.michigandaily.com. Accessed April 6,
- 5.Centers for Disease Control and Prevention (CDC) Hyperthermia and dehydration-related deaths associated with intentional rapid weight loss in three collegiate wrestlers North Carolina, Wisconsin, and Michigan, November–December 1997. MMWR Morb Mortal Wkly Rep. 1998;47(6):105–108. [PubMed] [Google Scholar]
- 6.Kellog A.P, Suggs W. Deaths of 3 college football players worry athletic officials. Chron Higher Educ. 2007. http://chronicle.com/weekly/v47/i49/49a03501.htm. Published August 17, 2001. Accessed April 8,
- 7.Branch J.D, Schwarz W.D, Van Lunen B. Effect of creatine supplementation on cycle ergometer exercise in a hyperthermic environment. J Strength Cond Res. 2007;21(1):57–61. doi: 10.1519/00124278-200702000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Easton C, Turner S, Pitsiladis Y.P. Creatine and glycerol hyperhydration in trained subjects before exercise in the heat. Int J Sport Nutr Exerc Metab. 2007;17(1):70–91. doi: 10.1123/ijsnem.17.1.70. [DOI] [PubMed] [Google Scholar]
- 9.Hile A.M, Anderson J.M, Fiala K.A, Stevenson J.H, Casa D.J, Maresh C.M. Creatine supplementation and anterior compartment pressure during exercise in the heat in dehydrated men. J Athl Train. 2006;41(1):30–35. [PMC free article] [PubMed] [Google Scholar]
- 10.Kern M, Podewils L.J, Vukovich M, Buono M.J. Physiological response to exercise in the heat following creatine supplementation. JEP Online. 2007. 2001. http://www.faculty.css.edu/tboone2/asep/Kern.doc. Accessed April 8,
- 11.Kilduff L.P, Georgiades E, James N, et al. The effects of creatine supplementation on cardiovascular, metabolic, and thermoregulatory responses during exercise in the heat in endurance-trained humans. Int J Sport Nutr Exerc Metab. 2004;14(4):443–460. doi: 10.1123/ijsnem.14.4.443. [DOI] [PubMed] [Google Scholar]
- 12.Mendel R.W, Blegen M, Cheatham C, Antonio J, Ziegenfuss T. Effects of creatine on thermoregulatory responses while exercising in the heat. Nutrition. 2005;21(3):301–307. doi: 10.1016/j.nut.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 13.Powers M.E, Arnold B.L, Weltman A.L, et al. Creatine supplementation increases total body water without altering fluid distribution. J Athl Train. 2003;38(1):44–50. [PMC free article] [PubMed] [Google Scholar]
- 14.Rosene J.M, Whitman S.A, Forgarty T.D. A comparison of thermoregulation with creatine supplementation between the sexes in a thermoneutral environment. J Athl Train. 2004;39(1):50–55. [PMC free article] [PubMed] [Google Scholar]
- 15.Volek J.S, Mazzetti S.A, Farquhar W.B, Barnes B.R, Gomez A.L, Kraemer W.J. Physiological responses to short-term exercise in the heat after creatine loading. Med Sci Sports Exerc. 2001;33(7):1101–1108. doi: 10.1097/00005768-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Watson G, Casa D.J, Fiala K.A, et al. Creatine use and exercise heat tolerance in dehydrated men. J Athl Train. 2006;41(1):18–29. [PMC free article] [PubMed] [Google Scholar]
- 17.Weiss C.A, Powers M.E. Creatine supplementation does not impair the thermoregulatory response during a bout of exercise in the heat. J Sports Med Phys Fitness. 2006;46(4):555–563. [PubMed] [Google Scholar]
- 18.Greenwood M, Kreider R.B, Greenwood L, Byars A. Cramping and injury incidence in collegiate football players are reduced by creatine supplementation. J Athl Train. 2003;38(3):216–219. [PMC free article] [PubMed] [Google Scholar]
- 19.Greenwood M, Kreider R.B, Melton C, et al. Creatine supplementation during college football training does not increase the incidence of cramping or injury. Mol Cell Biochem. 2003;244(1–2):83–88. [PubMed] [Google Scholar]
- 20.Kreider R.B, Melton C, Rasmussen C.J, et al. Long-term creatine supplementation does not significantly affect clinical markers of health in athletes. Mol Cell Biochem. 2003;244(1–2):95–104. [PubMed] [Google Scholar]
- 21.Ziegenfuss T.N, Lowery L.M, Lemon P.W.R. Acute volume fluid changes in men during three days of creatine supplementation. JEP Online. 1993;2006;1 http://faculty.css.edu/tboone2/asep/jan13d.htm. Accessed August 30, [Google Scholar]
- 22.Wright G.A, Grandjean P.W, Pascoe D.D. The effects of creatine loading on thermoregulation and intermittent sprint exercise performance in a hot humid environment. J Strength Cond Res. 2007;21(3):655–660. doi: 10.1519/R-22186.1. [DOI] [PubMed] [Google Scholar]
- 23.PEDro Scale. 2007. http://www.pedro.fhs.usyd.edu.au/. Accessed April 8,
- 24.Hubbard T.J, Aronson S.L, Denegar C.R. Does cryotherapy hasten return to participation? A systematic review. J Athl Train. 2004;39(1):88–94. [PMC free article] [PubMed] [Google Scholar]
- 25.Thacker S.B, Gilchrist J, Stroup D.F, Kimsey C.D., Jr The impact of stretching on sports injury risk: a systematic review of the literature. Med Sci Sports Exerc. 2004;36(3):371–378. doi: 10.1249/01.mss.0000117134.83018.f7. [DOI] [PubMed] [Google Scholar]
- 26.O’Brien K.O, Nixon S, Tynan A.M, Glazier R.H. Effectiveness of aerobic exercise in adults living with HIV/AIDS: systematic review. Med Sci Sports Exerc. 2004;36(10):1659–1666. doi: 10.1249/01.mss.0000142404.28165.9b. [DOI] [PubMed] [Google Scholar]
- 27.Wasielewski N.J, Kotsko K.M. Does eccentric exercise reduce pain and improve strength in physically active adults with symptomatic lower extremity tendinosis? A systematic review. J Athl Train. 2007;42(3):409–421. [PMC free article] [PubMed] [Google Scholar]
- 28.Viera A.J, Garrett J.M. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–363. [PubMed] [Google Scholar]
- 29.Casa D.J, Becker S.M, Ganio M.S, et al. Validity of devices that assess body temperature during outdoor exercise in the heat. J Athl Train. 2007;42(3):333–342. [PMC free article] [PubMed] [Google Scholar]
- 30.Casa D.J, Fiala K.A, Roti M.W, et al. Influence of 10 days of creatine loading on hydration status [abstract] J Athl Train. 2004;39(2 suppl):S32. [Google Scholar]
- 31.Dalbo V.J, Roberts M.D, Stout J.R, et al. Putting the myth of creatine supplementation leading to muscle cramps and dehydration to rest. Br J Sports Med. 2008;42(7):567–573. doi: 10.1136/bjsm.2007.042473. [DOI] [PubMed] [Google Scholar]