Abstract
Context:
For athletes in disciplines with weight categories, it is important to assess body composition and weight fluctuations.
Objective:
To evaluate the accuracy of measuring body fat percentage with a portable ultrasound device possessing high accuracy and reliability versus fan-beam, dual-energy X-ray absorptiometry (DEXA).
Design:
Cross-validation study.
Setting:
Research laboratory.
Patients or Other Participants:
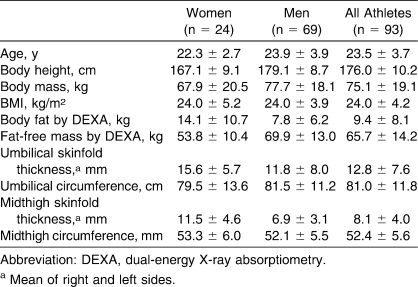
A total of 93 athletes (24 women, 69 men), aged 23.5 ± 3.7 years, with body mass index = 24.0 ± 4.2 and body fat percentage via DEXA = 9.41 ± 8.1 participated. All participants were elite athletes selected from the Institut National des Sports et de l'Education Physique. These participants practiced a variety of weight-category sports.
Main Outcome Measure(s):
We measured body fat and body fat percentage using an ultrasound technique associated with anthropometric values and the DEXA reference technique. Cross-validation between the ultrasound technique and DEXA was then performed.
Results:
Ultrasound estimates of body fat percentage were correlated closely with those of DEXA in both females (r = 0.97, standard error of the estimate = 1.79) and males (r = 0.98, standard error of the estimate = 0.96). The ultrasound technique in both sexes had a low total error (0.93). The 95% limit of agreement was −0.06 ± 1.2 for all athletes and did not show an overprediction or underprediction bias. We developed a new model to produce body fat estimates with ultrasound and anthropometric dimensions.
Conclusions:
The limits of agreement with the ultrasound technique compared with DEXA measurements were very good. Consequently, the use of a portable ultrasound device produced accurate body fat and body fat percentage estimates in relation to the fan-beam DEXA technique.
Keywords: body composition, DEXA, anthropometry
Key Points.
Assessing athletes' body composition accurately is beneficial as an indicator of health and performance status.
Compared with dual-energy X-ray absorptiometry testing, the new portable ultrasound device provided very accurate estimates of body fat percentage.
In sport disciplines with weight categories, assessing individual weight fluctuations and their consequences on body composition is important to optimize the performances of athletes during competitions.1–3 Just before a competition, some athletes need to lose a large quantity of body weight in a short period of time. This weight loss is difficult for many athletes because it often results in poorer performances.4,5 It is, therefore, necessary to determine each athlete's ideal weight category. For that purpose, knowledge of body composition in relation to total body fat (BF) and fat-free mass (FFM) is required. Optimizing these components is essential for improving physical training for each athlete.
To evaluate BF percentage (BF%), a noninvasive portable ultrasound device that measures the thickness of subcutaneous fat and has been validated on sedentary participants can be used. Pineau et al6 cross-validated the portable ultrasound technique (UT), air-displacement plethysmography, and bioelectric impedance (BIA) with fan-beam, dual-energy X-ray absorptiometry (DEXA) in 89 healthy volunteers. Body fat percentage estimates by UT were more accurate than those obtained with air-displacement plethysmography or BIA, regardless of sex.
A cross-validation study between UT and the DEXA reference was carried out and the results compared on 93 athletes. The portable UT measures the thickness of subcutaneous fat. These measurements were taken at specific points on all participants for the estimation of BF, BF%, and FFM. This technique has also been used to measure subcutaneous fat thickness and to determine total body density and total BF%.7,8
It should be noted that, until now, the UT has often been used for local measurements, specifically for the quantification of visceral fat in order to study android obesity.9–14 However, none of these authors have compared the technique with fan-beam DEXA.
Our purpose, therefore, was to determine total BF using the portable UT device. We wished to extend the application of our device by establishing a new predictive model to measure body composition of top athletes.
Methods
Participants
This study was conducted at the Institut National des Sports et de l'Education Physique (INSEP), Paris, France. Ninety-three athletes (24 women, 69 men), ranging in age from 18 to 33 years, were selected for the study. The athletes were recruited through INSEP via athletic trainers. Participants' characteristics are shown in Table 1. The sample included 15 tae kwon do, 14 wrestling, 35 judo, 17 boxing, and 12 rowing athletes. After being informed about the purpose of the study, all athletes signed a written consent form. The study protocol was approved by the regional ethics committee for healthy volunteers.
Table 1.
Participants' Characteristics (Mean ± SD)
Data Collection Procedures
For each athlete examined, total body composition was measured with DEXA and UT on the same day, in the morning before training. All athletes were at rest, had breakfast before the measurements, and were properly hydrated, having ingested about 10 oz (296 mL) of water 20 minutes before the DEXA measurement.
Dual-Energy X-Ray Absorptiometry
The BF% measurements were obtained with a Hologic device (model QDR 4500W; Hologic, Inc, Bedford, MA). The DEXA method uses an X-ray tube with a filter to generate low-energy (40-kV) and high-energy (70- or 100-kV) photons. Scan time for a total body measurement is approximately 7 minutes. Participants are asked to lie down and are exposed to weak irradiation. Hologic software (version 11.2.5) produces highly accurate BF and BF% estimates (to about 1%).15 The mass of the participant can also be calculated very accurately by DEXA (to about 1%).
Ultrasound Device
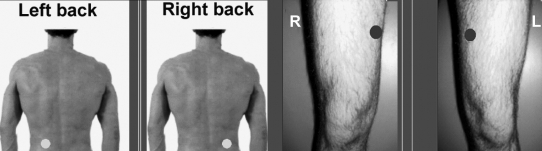
Ultrasound measurements were taken using a sonographic GEM in A mode (TEA Company, Vandoeuvre-les-Nancy, France). The ultrasonic technique can be used to measure the thickness of fat between the skin and the muscle. A transducer probe emits, through the skin, an ultrasonic wave, part of which is reflected in the fat-muscle interface. We selected 2 preferred anatomical areas: the intra-abdominal area, which is often associated with metabolic risk factors,16–18 and the midthigh area (Figure 1). Subcutaneous fat was located in a horizontal plane with an approximately 45° vertebral axis at the umbilical level, in the middle of the knee, and at the top of the thigh anteriorly. Abdominal and midthigh subcutaneous fat was measured using a 5.0-MHz linear array probe. A probe diameter of 0.75 in (1.90 cm) is the most suitable in terms of positioning, location, orientation, contact, and pressure. We obtained highly reliable, repeated measurements of fat thickness with 2 examiners working with the same 10 athletes, using an ultrasonic technique: the intraclass correlation coefficient was above 0.98.
Figure 1. Measurement points at umbilical level (right and left back) and midthigh level. Skinfold thickness was measured at the umbilical level using a 5.0-MHz linear array probe. L indicates left; R, right.
We used a 2-compartment model of BF and FFM. For all athletes, BF was measured by the same investigator using a UT GEM device associated with anthropometric values. Height (cm), mass (kg), body mass index (BMI, kg/m2), and umbilical and midthigh circumferences on the left and right sides were recorded using a standard anthropometric technique.19 Height was measured without shoes to the nearest 0.1 cm, using a floor-standing stadiometer (Seca Corp, Semur-en-Auxois, France). Body mass was measured to the nearest 0.01 kg using a calibrated scale (model HD-372; Tanita France SA, Neuilly-Sur-Seine, France).
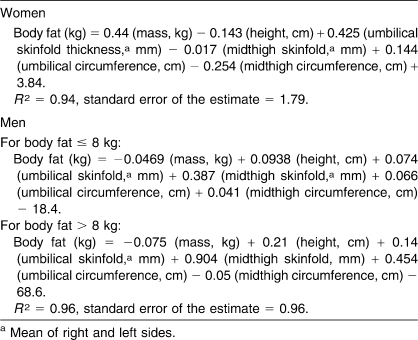
We developed new models to produce BF estimates with ultrasound and anthropometric dimensions versus DEXA. Because sex differences in body composition are apparent during adolescent and persist through adulthood,20 we used separate models for men and women. For men, the model used to estimate BF was a stepwise linear regression with a breakpoint using BF (DEXA) as a dependent variable (Table 2). The breakpoint was automatically calculated. For each athlete, a multiple linear regression analysis provided an estimate of BF, which was used to determine which of the linear regressions was appropriate. For women, the model used to estimate BF was a multiple linear regression analysis.
Table 2.
Body Fat Estimate Using Ultrasound and Anthropometric Dimensions Calculated With a Stepwise Linear Regression
Statistical Analysis
The relationships between BF% estimates by DEXA and UT were examined using paired-samples t tests. We created a regression equation for the first 47 athletes and then evaluated that regression with the remaining athletes. The accuracy of BF prediction with the regression analysis was evaluated using the coefficient of determination (r2), the standard error of the estimate (SEE), and the total error (TE) (∑[Ŷ − Y]2/n)1/2 as described by Lohman,21 where Ŷ is BF% estimated by UT, Y is BF% by DEXA, and n is the number of participants. Agreement between body composition estimates was examined by calculating the 95% limits of agreement, as described by Bland and Altman.22 Additionally, potential bias between BF% estimates by DEXA and UT was examined using residual plots. For all analyses, the α level used for statistical significance was .05. All results are expressed as mean ± SD unless otherwise indicated. Statistical analysis was carried out with Statistica software (version 6; StatSoft France, Maisons-Alfort, France).
Results
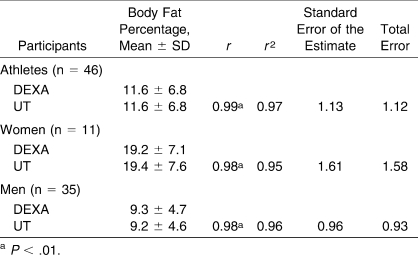
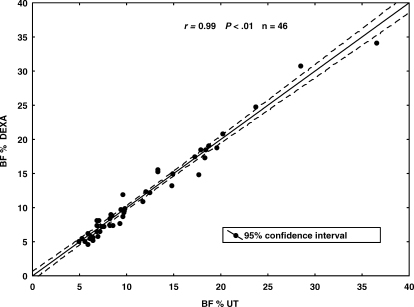
A summary of the results relating to the accuracy of and bias in measurement of BF% as assessed by UT is given in Table 3. When comparing the remaining athletes (n = 46), BF% determined by UT showed a nonsignificant difference compared with DEXA. All BF% estimates by UT were correlated with BF% estimates by DEXA, regardless of sex. Figure 2 illustrates the variation around the regression line (SEE).
Table 3.
Summary of the Association Between Dual-Energy X-ray Absorptiometry (DEXA) and Portable Ultrasound (UT) Body Fat Percentage Estimates (n = 46)
Figure 2. Regression between body fat (BF) percentage estimates using dual-energy X-ray absorptiometry (DEXA) and portable ultrasound (UT) on 46 athletes.
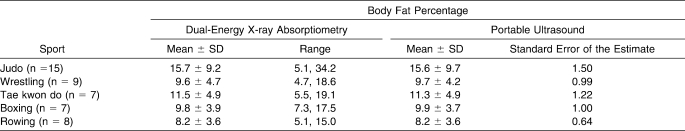
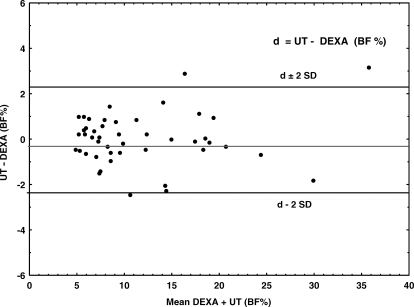
The actual mean difference of the TE between BF% as measured by DEXA and UT confirmed the regression findings for the remaining athletes. The TE was small for the UT technique, regardless of sex. Moreover, the SEE was small for all disciplines, despite the range of BF% (Table 4). Residual comparisons plotting differences between DEXA and UT estimates of BF% (Figure 3) revealed no bias across the range of fatness (r = 0.12, P > .41).
Table 4.
Standard Error of the Estimate of the Body Fat Percentage Determined Using Dual-Energy X-ray Absorptiometry and Portable Ultrasound by Sport (n = 46)
Figure 3. Bland-Altman plots comparing body fat (BF) percentages estimates using dual-energy X-ray absorptiometry (DEXA) and portable ultrasound (UT) on 46 athletes. SD indicates standard deviation.
Discussion
Our primary objective was to compare the accuracy of BF% measurement between UT and DEXA criterion measures. The BF% estimates with UT were correlated with those obtained by DEXA (r > 0.96) for male and female athletes. According to Lohman,23 Sinning et al,24 and Clark et al,25 the validation of new methods of body composition analysis should include an evaluation of mean ± SD, SEE, and TE. In the present study, the SEE calculated by regression analysis for UT is ideal (<2.00) regardless of sex (SEE = 0.96 for men, 1.79 for women), according to the Lohman classification.23 Recently this author indicated that the SEE must be less than 3% for a new method to be accepted as accurate. Lohman23 and Clark et al25 suggested TE as the best single measure for evaluating differences between new and reference measures. In our study, TE ranged from 0.93 to 1.58, indicating a very high level of agreement.
We used the methods described by Bland and Altman22 to examine the level of individual agreement between DEXA and UT BF% estimates. The relatively small limits of agreement, ranging from −2.3 to 2.3 BF%, reflect a high level of accuracy for the UT, with a symmetric dispersion around the mean difference (−0.013). Figure 3 also indicates that no UT bias was present.
The results obtained with our UT GEM device are more accurate than those obtained through traditional techniques used routinely, such as BIA and skinfold thickness. Many researchers have used DEXA to cross-validate field method equations for athletes. DeLorenzo et al26 indicated that results using BIA or skinfold thickness methods were not interchangeable with results using DEXA in 43 trained male athletes. The Bland-Altman analysis showed that the 95% confidence intervals for the higher and lower limits of agreement for DEXA, BIA, and skinfold thickness were quite wide for clinical use. Stewart and Hannan27 pointed out that the BF% measured by DEXA in male athletes was predicted with an SEE of 2.8 kg for BIA and 1.7 kg for skinfolds. Moreover, applying the derived equations to a separate sample of 24 athletes, they predicted a fat mass with a TE of 2.9%. Houtkooper et al28 reported that BIA overestimated the average BF% of elite female heptathletes by 4.4%.
The accuracy of our device is good (SEE < 1.5), despite the range of BF% in the various disciplines (Table 4). Moreover, the model used to estimate BF% is accurate regardless of the size of the sample. The precision of the predictive equation (R2 = 0.97, SEE = 1.29) with the first 47 athletes did not increase with the remaining 46 athletes (R2 = 0.97, SEE = 1.13) or with the total sample of 93 athletes (R2 = 0.97, SEE = 1.21). In this case, the response variable and the predictor variables are highly correlated, and we therefore have a stable equation.29 Consequently, the model used to estimate BF% with the UT should be extended to disciplines with weight categories. Similar to a scan, the UT is noninvasive and harmless. It is cheaper in terms of both acquisition and use and has the advantage of being portable.
Characterizing body composition is useful for achieving optimal physical performance and is an important part of monitoring the athlete's physical and mental health. To optimize performance, the athlete may wish to reduce BF content and increase muscle strength through various training methods. Diets and excessive training often result in a severe energy deficit, with a smaller amount of muscle mass and a relatively higher amount of fat mass. The resulting higher BF% and lower muscle mass inevitably result in a performance reduction that motivates the athlete to follow regimens that produce even greater energy deficit. Radical changes in body composition can indicate serious health concerns.
In sports with weight categories, each athlete competes in a weight category; the categories are determined by each sport federation. Just before the competition, some athletes may need to lose a large quantity of body weight in a short period. Weight loss in lower weight categories often leads to poorer performances. Consequently, it is necessary to determine each athlete's ideal weight category with body composition measurements. During competition, measuring body composition is necessary in order to rehydrate every athlete appropriately, by precisely estimating fat mass and, consequently, FFM. Determining the required amount of rehydration depends on accurately measuring BF and lean body mass.
Our goal is to integrate body composition indicators into physical training and to optimize the weight category for each athlete. Our UT GEM device can be used in different situations. In the short term, just after training or on the same day, weight loss corresponds with water loss. In the middle term or the long term, weight loss without modification of BF should correspond with a change in lean body mass and muscle mass. Moreover, the high accuracy of the BF estimate with our device helps the coach to decide whether to change the athlete's weight category or not.
In conclusion, accurate body composition assessment is beneficial for athletes, because it can indicate health and performance status. Our comparison of BF% estimates by looking at UT versus DEXA was very accurate, regardless of the athlete's sex or the range of BF% of athletes in different sports. Consequently, the use of a portable UT device based on a technique associated with anthropometry allowed us to determine BF% with a high level of accuracy in accordance with DEXA. In addition, our device allows identification of body composition characteristics common to elite athletes within a specific sport.
Footnotes
Jean-Claude Pineau, PhD; Jean Robert Filliard, PhD; and Michel Bocquet, PhD, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
References
- 1.Hendler R.G, Welle S.L, Statt M.C, Barnard R, Amatruda J.M. The effects of weight reduction to ideal body weight on body fat distribution. Metabolism. 1995;44(11):1413–1416. doi: 10.1016/0026-0495(95)90139-6. [DOI] [PubMed] [Google Scholar]
- 2.Mourier A, Bigard A.X, de Kerviler E, Roger B, Legrand H, Guezennec C.Y. Combined effects of caloric restriction and branched-chain amino acid supplementation on body composition and exercise performance in elite wrestlers. Int J Sports Med. 1997;18(1):47–55. doi: 10.1055/s-2007-972594. [DOI] [PubMed] [Google Scholar]
- 3.Nindl B.C, Friedl K.E, Marchitelli L.J, Shippee R.L, Thomas C.D, Patton J.F. Regional fat placement in physically fit males and changes with weight loss. Med Sci Sports Exerc. 1996;28(7):786–793. doi: 10.1097/00005768-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Horswill C.A, Hickner R.C, Scott J.R, Costill D.L, Gould D. Weight loss, dietary carbohydrate modifications and high intensity, physical performance. Med Sci Sports Exerc. 1990;22(4):470–476. [PubMed] [Google Scholar]
- 5.Park S.H, Roemmich J.N, Horswill C.A. A season of wrestling and weight loss by adolescent wrestlers: effect on anaerobic arm power. J Appl Sports Sci Res. 1990;4:1–4. [Google Scholar]
- 6.Pineau J.C, Guihard-Costa A.M, Bocquet M. Validation of ultrasound techniques applied to body fat measurement: a comparison between ultrasound techniques, air displacement plethysmography and bioelectrical impedance vs dual-energy X-ray absorptiometry. Ann Nutr Metab. 2007;51(5):421–427. doi: 10.1159/000111161. [DOI] [PubMed] [Google Scholar]
- 7.Fanelli M.T, Kuczmarski R.J. Ultrasound as an approach to assessing body composition. Am J Clin Nutr. 1984;39(5):703–709. doi: 10.1093/ajcn/39.5.703. [DOI] [PubMed] [Google Scholar]
- 8.Yasukawa M, Horvath S.M, Oishi K, Kimura M, Williams R, Maeshima T. Total body fat estimations by near-infrared interactance, A-mode ultrasound, and underwater weighing. Appl Human Sci. 1995;14(4):183–189. doi: 10.2114/ahs.14.183. [DOI] [PubMed] [Google Scholar]
- 9.Stolk R.P, Wink O, Zelissen P.M.J, Meijer R, van Gils A.P.G, Grobbee D.E. Validity and reproducibility of ultrasonography for the measurement of intra-abdominal adipose tissue. Int J Obes Relat Metab Disord. 2001;25(9):1346–1351. doi: 10.1038/sj.ijo.0801734. [DOI] [PubMed] [Google Scholar]
- 10.Wirth A, Steinmetz B. Gender differences in changes in subcutaneous and intra-abdominal fat during weight reduction: an ultrasound study. Obes Res. 1998;6(6):393–399. doi: 10.1002/j.1550-8528.1998.tb00370.x. [DOI] [PubMed] [Google Scholar]
- 11.Armellini F, Zamboni M, Robbi R, et al. Total and intra-abdominal fat measurements by ultrasound and computerized tomography. Int J Obes Relat Metab Disord. 1993;17(4):209–214. [PubMed] [Google Scholar]
- 12.Tornaghi G, Raiteri R, Pozzato C. Anthropometric or ultrasonic measurements in assessment of visceral fat? A comparative study. Int J Obes Relat Metab Disord. 1994;18(11):771–775. [PubMed] [Google Scholar]
- 13.Ishida Y, Carroll J.F, Pollock M.I, Graves J.E, Leggett S.H. Reliability of B-mode ultrasound for the measurement of body fat and muscle thickness. Am J Hum Biol. 1992;4(4):511–520. doi: 10.1002/ajhb.1310040410. [DOI] [PubMed] [Google Scholar]
- 14.Sabir N, Pakdemirli E, Sermez Y, Zencir M, Kazil S. Sonographic assessment of changes in thickness of different abdominal fat layers in response to diet in obese women. J Clin Ultrasound. 2003;31(1):26–30. doi: 10.1002/jcu.10129. [DOI] [PubMed] [Google Scholar]
- 15.Lohman T.G. Dual Energy X-Ray Absorptiometry. Champaign, IL: Human Kinetics; 1996. pp. 63–78. [Google Scholar]
- 16.von Eyben F.E, Mouristen E, Holm J, et al. Intra-abdominal obesity and metabolic risk factors: a study of young adults. Int J Obes Relat Metab Disord. 2003;27(8):941–949. doi: 10.1038/sj.ijo.0802309. [DOI] [PubMed] [Google Scholar]
- 17.Goran M.I. Visceral fat in prepubertal children: influence of obesity, anthropometry, ethnicity, gender, diet, and growth. Am J Hum Biol. 1999;11(2):201–207. doi: 10.1002/(SICI)1520-6300(1999)11:2<201::AID-AJHB8>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 18.Roemmich J.N, Rogol A.D. Hormonal changes during puberty and their relationship to fat distribution. Am J Hum Biol. 1999;11(2):209–224. doi: 10.1002/(SICI)1520-6300(1999)11:2<209::AID-AJHB9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 19.Lohman T.G, Roche A.F, Martorell R. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics; 1988. pp. 56–68. [Google Scholar]
- 20.Malina R.M, Bouchard C, Bar-Or O. Growth, Maturation and Physical Activity. 2nd ed. Champaign, IL: Human Kinetics; 2004. pp. 527–551. [Google Scholar]
- 21.Lohman T.G. Skinfolds and body density and their relation to body fatness: a review. Hum Biol. 1981;53(2):181–225. [PubMed] [Google Scholar]
- 22.Bland J.M, Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 23.Lohman T.G. Advances in Body Composition Assessment: Current Issues in Exercise Science. Champaign, IL: Human Kinetics; 1992. pp. 3–4. Series Monograph No. 3. [Google Scholar]
- 24.Sinning W.E, Dolny D.G, Little K.D, et al. Validity of “generalized” equations for body composition analysis in male athletes. Med Sci Sports Exerc. 1985;17(1):124–130. [PubMed] [Google Scholar]
- 25.Clark R.R, Kuta J.M, Sullivan J.C. Prediction of percent body fat in adult males using dual energy X-ray absorptiometry, skinfolds, and hydrostatic weighing. Med Sci Sports Exerc. 1993;25(4):528–535. [PubMed] [Google Scholar]
- 26.De Lorenzo A, Bertini I, Iacopino L, Pagliato E, Testolin C, Testolin G. Body composition measurement in highly trained male athletes: a comparison of three methods. J Sports Med Phys Fitness. 2000;40(2):178–183. [PubMed] [Google Scholar]
- 27.Stewart A.D, Hannan W.J. Prediction of fat and fat-free mass in male athletes using dual x-ray absorptiometry as the reference method. J Sports Sci. 2000;18(4):263–274. doi: 10.1080/026404100365009. [DOI] [PubMed] [Google Scholar]
- 28.Houtkooper L.B, Mullins V.A, Going S.B, Brown C.H, Lohman T.G. Body composition profiles of elite American heptathletes. Int J Sport Nutr Exerc Metab. 2001;11(2):162–173. doi: 10.1123/ijsnem.11.2.162. [DOI] [PubMed] [Google Scholar]
- 29.Heymsfield S.B, Lohman T.G, Wang Z.M, Going S.B. Human Body Composition. Champaign, IL: Human Kinetics; 2005. pp. 154–160. [Google Scholar]