Abstract
Background
Heart failure (HF) patients’ knowledge about their disease may improve short-term outcomes and may be related to their level of education. However, the effects of patients and spousal education on long-term outcomes in ambulatory chronic HF are unknown. .
Methods
Of the 571 patients enrolled in the quality of life sub-study of the Digitalis Investigation Group trial, 159 patients or their spouses reported having higher (>12 years) education. Propensity score for higher education, calculated for each patient using a logistic regression model, was used to match 112 (70% of 159) higher education patients with 215 patients with high school (≤12 years) education. Matched Cox regression analyses were used to estimate associations of high school education with mortality and hospitalizations.
Results
All-cause hospitalizations occurred in 56% (rate, 3233/10,000 person-years) of higher education and 65% (rate, 4558/10,000 person-years) of high school education patients (hazard ratio {HR} for high school, compared with higher education=1.52; 95% confidence interval {CI}=1.06–2.16; p=0.022). Hospitalizations due to cardiovascular causes occurred in 42% (rate, 2067/10,000 person-years) of higher education and 50% (rate, 4558/10,000 person-years) of high school education patients (HR=1.55; 95% CI, 1.05–2.30; p=0.029). All-cause mortality occurred in 20% (rate, 746/10,000 person-years) of higher education and 30% (rate, 1204/10,000 person-years) of high school education patients (HR=1.52; 95% CI=0.89–2.58; p=0.124).
Conclusions
Compared with >12 years of education, lower education was associated with increased hospitalizations among ambulatory chronic HF patients. Patient and spousal education levels may be used to risk stratify HF patients at high risk for hospitalizations.
Keywords: Education, heart failure, mortality, hospitalization
1. Introduction
Systematic and tailored health education to improve heart failure (HF) patients’ knowledge and understanding about their disease symptoms and treatment has been shown to improve short-term outcomes [1–5]. Patients’ understanding of their chronic medical conditions and their ability to learn about them may be influenced by their education level, and that of their spouses [6]. Higher levels of education have also been shown to be associated with higher levels of disease-specific knowledge, healthy lifestyle, and improved outcomes [7–11]. However, the effects of education levels of patients and their spouses on long-term outcomes in ambulatory chronic HF have not been well studied. In the current analysis, we examined the association between education and long-term outcomes in a propensity score matched cohort of chronic HF patients enrolled in the quality of life sub-study of the Digitalis Investigation Group (DIG) trial.
2. Methods
We conducted a post-hoc propensity-matched study of a public-use version of the DIG dataset obtained from the National Heart, Lung and Blood Institute. During 1991–1993, 7788 ambulatory chronic HF patients (6800 systolic HF, with left ventricular ejection fraction ≤45%) were recruited from 302 centers in the United States and Canada, and were randomized into digoxin and placebo groups [12]. Of these, 93% patients were receiving angiotensin-converting enzyme inhibitor and 78% were receiving diuretics. The median follow-up time for DIG participants were 38 months. Vital status was collected up to December 31, 1995 and was ascertained for 99% of the patients [13].
A subgroup of 581 patients, who participated in the DIG Quality of Life sub-study, responded to questions about their and their spouses’ educational background. We categorized patients into high school (≤12 years) and higher (>12 years) education groups based on the education of patients or their spouses. Of the 571 patients (10 patients with missing education data were excluded from this analysis), 159 (28% of 571) patients had higher education. Next, we estimated propensity scores for higher education for all 571 patients, using a non-parsimonious multivariable logistic regression model (c statistic=0.73), and used that to match 112 (70% of 159) patients with higher education and 215 patients with high school education (1 patient with higher education were matched with up to 2 patients with high school education) in order to reduce the imbalance in baseline covariates. All baseline patient characteristics displayed in Table 1 and clinically plausible interactions [14–16] were included in the model as covariates. The propensity score is the conditional probability of receiving an exposure (e.g. higher education) given a set of measured covariates, and can be used to adjust for selection bias when assessing causal effects in observational studies [17, 18]. Pre-match mean propensity scores for patients with higher education and high school education were respectively 0.36765 and 0.24440 (absolute standardized difference, 83%; t-test p, <0.0001). After matching, mean propensity scores for higher and high school education were respectively 0.31797 and 0.30616 (absolute standardized difference, 8%; t-test p, 0.485). We also used Pearson chi-square and Student’s t test to compare the baseline characteristics of HF patients with higher education versus high school education before and after matching.
Table 1.
Baseline patient characteristics, before and after propensity score matching, by patient and spouse education
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| N (%) or mean (±SD) | High school education (≤12 years) (N=412) | Higher education >12 years (N=159) | P | High school education (≤12 years) (N=215) | Higher education (>12 years) (N=112) | P |
| Age (years) | 65.5 (±11.8) | 62.0 (±11.2) | 0.001 | 63.8 (±12.0) | 63.5 (±11.0) | 0.850 |
| Female | 119 (28.9%) | 33 (20.8%) | 0.049 | 47 (21.9%) | 25 (22.3%) | 0.924 |
| Non-white | 61 (14.8%) | 19 (11.9%) | 0.378 | 26 (12.1%) | 13 (11.6%) | 0.898 |
| Body mass index, kg/sq meter | 27.8 (±5.9) | 27.6 (±5.7) | 0.787 | 27.8 (±5.5) | 27.7 (±5.7) | 0.834 |
| Duration of HF (months) | 21.9 (±32.0) | 25.4 (±38.6) | 0.280 | 22.1 (±34.2) | 22.7 (±34.4) | 0.893 |
| Primary cause of HF | ||||||
| Ischemic | 279 (67.7%) | 106 (66.7%) | 143 (66.5%) | 80 (71.4%) | ||
| Hypertensive | 52 (12.6%) | 18 (11.3%) | 25 (11.6%) | 10 (8.9%) | ||
| Idiopathic | 60 (14.6%) | 27 (17.0%) | 0.892 | 35 (16.3%) | 15 (13.4%) | 0.748 |
| Others | 21 (5.1%) | 8 (5.0%) | 12 (5.6%) | 7 (6.3%) | ||
| Prior myocardial infarction | 267 (64.8%) | 102 (64.2%) | 0.883 | 139 (64.7%) | 76 (67.9%) | 0.562 |
| Current angina | 128 (31.1%) | 41 (25.8%) | 0.215 | 67 (31.2%) | 36 (32.1%) | 0.856 |
| Hypertension | 187 (45.4%) | 72 (45.3%) | 0.982 | 103 (47.9%) | 49 (43.8%) | 0.474 |
| Diabetes | 107 (26.0%) | 47 (29.6%) | 0.386 | 60 (27.9%) | 30 (26.8%) | 0.829 |
| Chronic kidney disease | 182 (44.2%) | 73 (45.9%) | 0.708 | 97 (45.1%) | 55 (49.1%) | 0.492 |
| Medications | ||||||
| Pre-trial digoxin use | 161 (39.1%) | 58 (36.5%) | 0.567 | 84 (39.1%) | 41 (36.6%) | 0.664 |
| Trial use of digoxin | 201 (48.8%) | 89 (56.0%) | 0.124 | 110 (51.2%) | 57 (50.9%) | 0.963 |
| ACE inhibitors | 361 (87.6%) | 137 (86.2%) | 0.640 | 184 (85.6%) | 97 (86.6%) | 0.800 |
| Hydralazine & nitrates | 6 (1.5%) | 4 (2.5%) | 0.476 | 5 (2.3%) | 3 (2.7%) | 1.000 |
| Diuretics | 303(73.5%) | 124(78.0%) | 0.273 | 164 (76.3%) | 86 (76.8%) | 0.918 |
| PS diuretics | 31 (7.5%) | 6 (3.8%) | 0.103 | 11 (5.1%) | 6 (5.4%) | 0.926 |
| Potassium supplement | 123 (29.9%) | 61 (38.4%) | 0.051 | 78 (36.3%) | 40 (35.7%) | 0.920 |
| Symptoms and signs of HF | ||||||
| Dyspnea at rest | 75 (18.2%) | 31 (19.5%) | 0.722 | 42 (19.5%) | 20 (17.9%) | 0.713 |
| Dyspnea on exertion | 313 (76.0%) | 110 (69.2%) | 0.097 | 166 (77.2%) | 82 (73.2%) | 0.423 |
| Activity limitation | 335 (81.3%) | 120 (75.5%) | 0.120 | 174 (80.9%) | 87 (77.7%) | 0.487 |
| Jugular venous distension | 35 (8.5%) | 22 (13.8%) | 0.056 | 23 (10.7%) | 14 (12.5%) | 0.625 |
| Third heart sound | 73 (17.7%) | 37 (23.3%) | 0.132 | 49 (22.8%) | 22 (19.6%) | 0.512 |
| Pulmonary râles | 63 (15.3%) | 20 (12.6%) | 0.410 | 33 (15.3%) | 14 (12.5%) | 0.486 |
| Lower extremity edema | 85 (20.6%) | 27 (17.0%) | 0.325 | 44 (20.5%) | 22 (19.6%) | 0.860 |
| NYHA functional class | ||||||
| I | 52 (12.6%) | 24 (15.1%) | 23 (10.7%) | 14 (12.5%) | ||
| II | 221 (53.6%) | 88 (55.3%) | 0.340 | 119 (55.3%) | 64 (57.1%) | 0.833 |
| III | 127 (30.8%) | 46 (28.9%) | 69 (32.1%) | 33 (29.5%) | ||
| IV | 12 (2.9%) | 1 (0.6%) | 4 (1.9%) | 1 (0.9%) | ||
| Heart rate (/minute), | 77.2 (±13.0) | 76.6 (±12.6) | 0.600 | 76.9 (±13.3) | 76.2 (±12.6) | 0.645 |
| Blood pressure (mm Hg) | ||||||
| Systolic | 128.0 (±21.9) | 127.6 (±22.4) | 0.817 | 128.9 (±22.1) | 128.1 (±21.6) | 0.742 |
| Diastolic | 74.7 (±12.2) | 75.9 (±12.6) | 0.276 | 76.3 (±12.2) | 75.7 (±11.7) | 0.674 |
| Pulmonary congestion | 44 (10.7%) | 15 (9.4%) | 0.661 | 21 (9.8%) | 13 (11.6%) | 0.605 |
| Cardiothoracic ratio >0.5 | 268 (65.0%) | 102 (64.2%) | 0.840 | 142 (66.0%) | 69 (61.6%) | 0.426 |
| Serum concentrations | ||||||
| Creatinine (mg/dL) | 1.27 (±0.38) | 1.27 (±0.32) | 0.965 | 1.30 (± 0.40) | 1.27 (± 0.30) | 0.536 |
| Potassium (mEq/L) | 4.33 (±0.41) | 4.24 (±0.46) | 0.020 | 4.28 (± 0.41) | 4.28 (± 0.46) | 0.959 |
| Estimated glomerular filtration rate (mL/min/1.73 square meter) | 63.2 (±20.6) | 62.9 (±16.3) | 0.863 | 63.2 (± 20.8) | 62.1 (± 16.2) | 0.618 |
| Ejection fraction (%) | 35.0 (±13.5) | 33.5 (±12.8) | 0.211 | 34.5 (±13.1) | 33.8 (±12.6) | 0.640 |
The primary outcomes of this analysis were all-cause mortality and all-cause hospitalization. However, we also studied mortality and hospitalization due to cardiovascular causes and worsening heart failure as secondary outcomes. Kaplan-Meier and matched Cox regression analysis were used to determine the effect of baseline education level on mortality and hospitalization. All data analyses were performed using SPSS for Windows version 14 (SPSS, Chicago, Illinois). All P values were 2-sided and P < 0.05 was regarded as statistically significant.
3. Results
The mean (±SD) age of the 327 matched patients was 64 (±12) years, (median 65; range 28–92), 22% were women, and 12% were non-whites. There were significant pre-match imbalances in several prognostically important covariates including age and sex that were balanced after matching (Table 1 and Figure 1). Absolute standardized differences for most baseline covariates were <10% in the post-matching cohort, suggesting substantial reduction of bias [14, 19, 20].
Figure 1.
Absolute standardized differences for covariates between patients with high school education and higher education, before and after propensity score matching
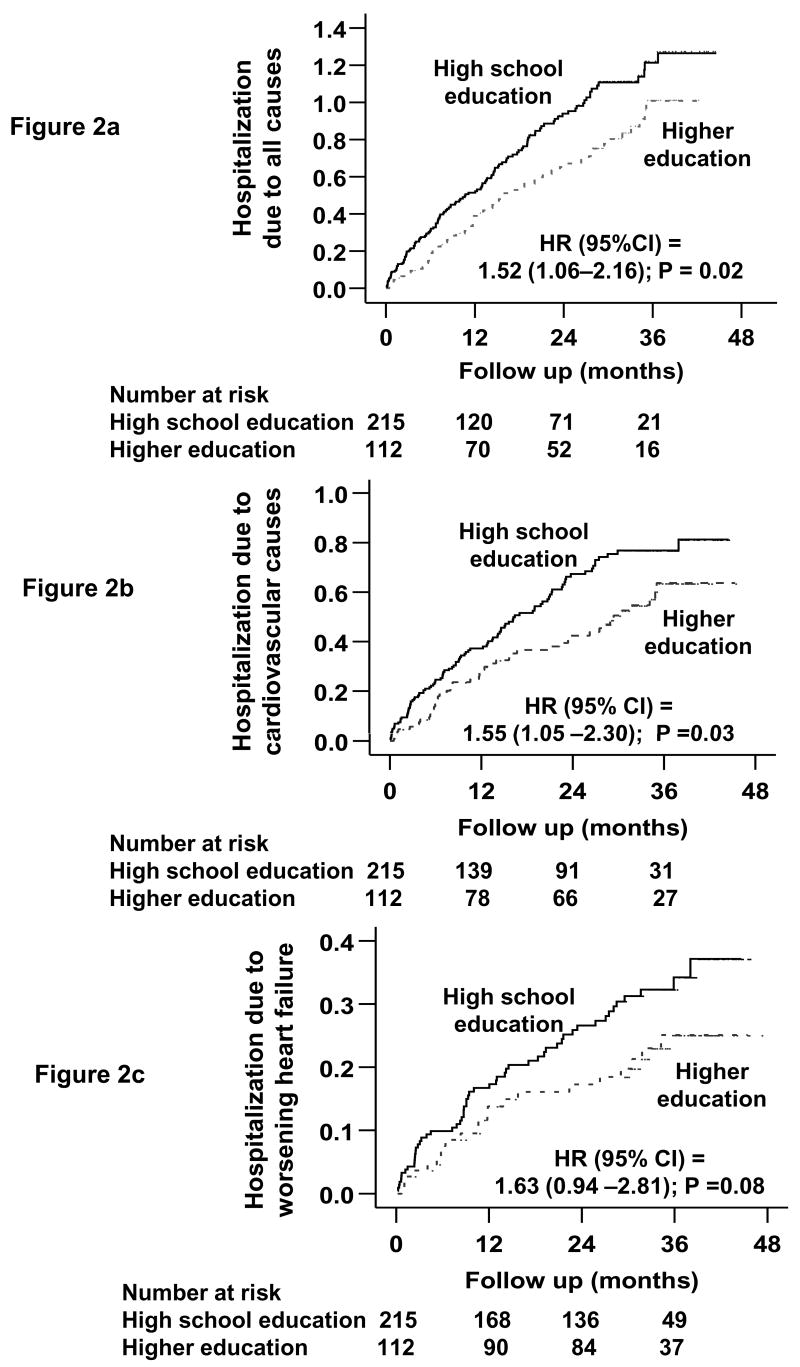
During an average 30 months of follow up (range, 0.3 to 45.4 months), hospitalizations due to all causes, cardiovascular causes and worsening HF occurred respectively in 202 (62%), 155 (47%) and 78 (24%) patients. Kaplan-Meier plots for hospitalizations are displayed in Figures 2 a–c. All-cause hospitalizations occurred in 56% (63/112) of patients in the higher education group (rate, 3233/10000 person-years) during a total of 195 person-years of follow-up and 65% (139/215) of patients in the high school education group (rate, 4558/10000 person-years) during a total of 305 years of follow-up (hazard ratio =1.52; 95% confidence interval =1.06–2.16; p =0.022; Table 2).
Figure 2.
Kaplan-Meier plots for hospitalization due to (a) all-causes, (b) cardiovascular causes, and (c) worsening heart failure
Table 2.
Association of high school education (versus higher education) with cause-specific mortalities and hospitalizations in a propensity matched cohort of heart failure patients
| Higher education(>12 years) (N=112)
|
High school Education (≤12 years) (N=215)
|
||||
|---|---|---|---|---|---|
| Rate, per 10000 person-years (events/total follow-up in years) | Absolute rate difference* (per 10000 person-years of follow-up) | Hazard ratio(95% confidence interval) | P value | ||
| Mortality | |||||
| All-cause | 746 (22/295) | 1,204 (64/531) | + 458 | 1.52 (0.89–2.58) | 0.124 |
| Cardiovascular | 644 (19/295) | 1,054 (56/531) | + 410 | 1.60 (0.90–2.84) | 0.110 |
| Worsening heart failure | 271 (8/295) | 452 (24/531) | + 180 | 1.58 (0.66–3.78) | 0.308 |
| Hospitalization** | |||||
| All-cause | 3,233 (63/195) | 4,558 (139/305) | + 1,325 | 1.52 (1.06–2.16) | 0.022 |
| Cardiovascular*** | 2,067 (47/227) | 3,009 (108/359) | + 942 | 1.55 (1.05–2.30) | 0.029 |
| Worsening heart failure | 826 (22/266) | 1,223 (56/458) | + 397 | 1.63 (0.94–2.81) | 0.082 |
| Number of total hospitalizations | 190 | 428 | + 238 | ||
Absolute differences in rates of events per 10000 person-year of follow up were calculated by subtracting the event rates in the higher education group from the event rates in the high school education group (before values were rounded)
Data shown include the first hospitalization of each patient due to each cause.
Cardiovascular hospitalization included first hospitalization due to worsening heart failure, ventricular arrhythmia, cardiac arrest, supraventricular arrhythmias, suspected digoxin toxicity, myocardial infarction, unstable angina, stroke, coronary revascularization, or cardiac transplantation.
Hospitalizations due to cardiovascular causes occurred in 42% (rate, 2067/10000 person-years) of higher education and 50% (rate, 3009/10000 person-years) of high school patients (hazard ratio =1.55; 95% confidence interval =1.05–2.30; p=0.029; Table 2). Hospitalizations due to worsening HF occurred in 20% (rate, 826/10000 person-years) of higher education and 26% (rate, 1223/10000 person-years) of high school education patients (hazard ratio =1.63; 95% confidence interval =0.94–2.81; p=0.082; Table 2).
During an average 30 months of follow-up, 86 (26%) patients died from all causes, 75 (23%) due to cardiovascular causes, and 32 (10%) due to progressive HF. All-cause mortality occurred in 20% (22/112) of patients in the higher education group (rate, 746/10000 person-years) during a total of 295 person-years of follow-up and 30% (64/215) of patients in the high school education group (rate, 1204/10000 person-years) during a total of 531 years of follow-up (hazard ratio =1.52; 95% confidence interval =0.89–2.58; p =0.124; Table 2). Associations of education with cardiovascular and HF mortalities and hospitalizations are displayed in Table 2.
4. Discussion
We observed that compared with ≥12 years of education, <12 years of patient or spousal education was associated with significant increase in hospitalizations due to all causes and cardiovascular causes, with a trend toward increase in HF hospitalizations, among ambulatory chronic HF patients. However, <12 years of education was not statistically associated with significant increase in mortality, likely due to small sample size of our study. These findings are important as HF patients and their spouses’ education levels can be used to identify HF patients at increased risk for hospitalizations.
As education levels correlate positively with socioeconomic status [21, 22], patients with higher education may have better understanding and knowledge of their disease process and treatment thereof. They also have easier access to high quality health care [23]. Patients with lower education levels are less likely to have a regular primary care physician [24, 25], to see or consult a cardiologist [26, 27], or be adherent to therapeutic recommendations [28, 29]. In addition, lower education level has been shown to be associated with poor quality of life [30], anxiety [30], physical and emotional distress [31], and inability to actively participate in self-care recommendations [32–34]. Non-compliance with medications and diet contributes to worsening HF symptoms, in many cases leading to HF hospitalizations [35]. Even though association of education level and hospitalization due to worsening HF did not reach statistical significance, likely due to small number of events, the association was in the same direction as for total and cardiovascular hospitalizations, and was of borderline significance. This consistency of associations of lower education with hospitalizations due to both cardiovascular and non-cardiovascular causes adds to the internal validity of our findings. Lack of significant association between education level and mortality was likely due to small number of events. For example, among patients in the lower education group, compared with 139 events of all-cause hospitalization, there were only 64 events of all-cause mortality. However, the large increase in absolute rates in all-cause mortality (458 extra deaths in patients with <12 years of education per 10000 person-years of follow-up) and the large magnitude (52%, similar to that of all-cause hospitalization; Table 2) of relative increase in all-cause mortality suggest that our study was underpowered to detect a significant association between education and mortality.
Data from non-HF patient populations suggest that lower education levels may be associated with increased mortality [10, 11, 36]. Among HF patients, lower socioeconomic status has been shown to be associated with increased HF hospitalization in hospitalized acute HF patients [27]. Education has also been shown to be associated with incident HF in men [37]. However, to the best of our knowledge, this is the first study of an association of education level and long-term outcomes in a cohort of propensity matched patients with chronic HF [27, 35, 37].
Despite improvements in therapy, rates of hospitalization and readmission in HF patients remain high [38]. It is estimated that approximately half of all HF readmissions may be preventable [32, 35]. Lack of adherence to and insufficient knowledge about diet, medication and HF symptoms may contribute to HF hospitalizations and readmissions [32, 33]. Our findings suggest that HF patients with lower level patient or spousal education are at increased risk of hospitalization and that these patents might benefit from targeted intervention to improve their knowledge about their disease [1–4].
These results of our study should be interpreted in light of its limitations. We did not have data on patients’ income, occupation, and insurance status. We used both patients’ and their spouses’ education levels; however, we had no data if spouses were living with the patients or were involved in care giving. Though propensity score matching can account for imbalances in all measured covariates, it may or may not balance unmeasured covariates. However, for any unmeasured confounder to explain away our finding it must be strongly related to both education level and outcomes, and be not strongly related to any of the many baseline covariates used in our analysis [12, 14]. Patients in our study were relatively younger, predominantly white men with normal sinus rhythm, thus limiting generalizability. Further, since the conduct of the DIG trial, the treatment of HF has changed significantly, and has become more complex and poly-pharmaceutical, potentially making it more difficult for patients with lower education to comprehend and adhere to. Thus, it is likely that associations observed in our analysis will be more pronounced in contemporary HF patients. Therefore, the results of this study needs to be replicated in contemporary HF patients.
In conclusion, educational status of HF patients and their spouses may be used to risk stratify HF patients at increased risk of hospitalizations, and probably of mortality, and targeted for appropriate interventions. Future prospective studies are needed to assess the potential prognostic role of education level in contemporary HF patients, and interventions need to be developed and tested to improve outcomes in those with lower levels of education.
Acknowledgments
“The Digitalis Investigation Group (DIG) study was conducted and supported from the NHLBI in collaboration with the DIG Investigators. This Manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the DIG Study or the NHLBI.”
Funding/Support: Dr. Ahmed is supported by the National Institutes of Health through grants from the National Institute on Aging (1-K23-AG19211-04) and the National Heart, Lung, and Blood Institute (1-R01-HL085561-01 and P50-HL077100).
Reference List
- 1.Jaarsma T, Halfens R, Huijer Abu-Saad H, et al. Effects of education and support on self-care and resource utilization in patients with heart failure. Eur Heart J. 1999;20:673–82. doi: 10.1053/euhj.1998.1341. [DOI] [PubMed] [Google Scholar]
- 2.Linne AB, Liedholm H, Israelsson B. Effects of systematic education on heart failure patients’ knowledge after 6 months. A randomised, controlled trial. Eur J Heart Fail. 1999;1:219–27. doi: 10.1016/s1388-9842(99)00041-0. [DOI] [PubMed] [Google Scholar]
- 3.Krumholz HM, Amatruda J, Smith GL, et al. Randomized trial of an education and support intervention to prevent readmission of patients with heart failure. J Am Coll Cardiol. 2002;39:83–9. doi: 10.1016/s0735-1097(01)01699-0. [DOI] [PubMed] [Google Scholar]
- 4.Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111:179–85. doi: 10.1161/01.CIR.0000151811.53450.B8. [DOI] [PubMed] [Google Scholar]
- 5.Stromberg A. The crucial role of patient education in heart failure. Eur J Heart Fail. 2005;7:363–9. doi: 10.1016/j.ejheart.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Mackenbach JP, Looman CW, van der Meer JB. Differences in the misreporting of chronic conditions, by level of education: the effect on inequalities in prevalence rates. Am J Public Health. 1996;86:706–11. doi: 10.2105/ajph.86.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simons CJ, Ritchie SK, Mullett MD, Liechty EA. Parental recall of infant medical complications and its relationship to delivery method and education level. J Dev Behav Pediatr. 1986;7:355–60. [PubMed] [Google Scholar]
- 8.Jacobsen BK, Thelle DS. Risk factors for coronary heart disease and level of education. The Tromso Heart Study. Am J Epidemiol. 1988;127:923–32. doi: 10.1093/oxfordjournals.aje.a114895. [DOI] [PubMed] [Google Scholar]
- 9.Drozdzowska B, Pluskiewicz W, Skiba M. Knowledge about osteoporosis in a cohort of Polish females: the influence of age, level of education and personal experiences. Osteoporos Int. 2004;15:645–8. doi: 10.1007/s00198-003-1581-2. [DOI] [PubMed] [Google Scholar]
- 10.Pincus T, Keysor J, Sokka T, Krishnan E, Callahan LF. Patient questionnaires and formal education level as prospective predictors of mortality over 10 years in 97% of 1416 patients with rheumatoid arthritis from 15 United States private practices. J Rheumatol. 2004;31:229–34. [PubMed] [Google Scholar]
- 11.Lee JR, Paultre F, Mosca L. The association between educational level and risk of cardiovascular disease fatality among women with cardiovascular disease. Womens Health Issues. 2005;15:80–8. doi: 10.1016/j.whi.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 12.The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–33. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 13.Collins JF, Howell CL, Horney RA. Determination of vital status at the end of the DIG trial. Control Clin Trials. 2003;24:726–30. doi: 10.1016/j.cct.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Ahmed A, Husain A, Love TE, et al. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–9. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed A, Ali M, Lefante CM, Mullick MS, Kinney FC. Geriatric heart failure, depression, and nursing home admission: an observational study using propensity score analysis. Am J Geriatr Psychiatry. 2006;14:867–75. doi: 10.1097/01.JGP.0000209639.30899.72. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed A, Perry GJ, Fleg JL, Love TE, Goff DC, Jr, Kitzman DW. Outcomes in ambulatory chronic systolic and diastolic heart failure: a propensity score analysis. Am Heart J. 2006;152:956–66. doi: 10.1016/j.ahj.2006.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenbaum P, Rubin D. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–24. [Google Scholar]
- 18.Rubin D. Using propensity score to help design observational studies: application to the tobacco litigation. Health Services Outcomes Res Methodol. 2001;2:169–88. [Google Scholar]
- 19.Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med. 2007;26:734–57. doi: 10.1002/sim.2580. [DOI] [PubMed] [Google Scholar]
- 20.Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–98. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–98. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 22.Kitagawa E, Hauser P. Differential mortality in the United States: a study in socioeconomic epidemiology. Cambridge, MA: Harvard University Press; 1973. [Google Scholar]
- 23.Feldman JJ, Makuc DM, Kleinman JC, Cornoni-Huntley J. National trends in educational differentials in mortality. Am J Epidemiol. 1989;129:919–33. doi: 10.1093/oxfordjournals.aje.a115225. [DOI] [PubMed] [Google Scholar]
- 24.Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med. 1991;114:325–31. doi: 10.7326/0003-4819-114-4-325. [DOI] [PubMed] [Google Scholar]
- 25.Rask KJ, Williams MV, Parker RM, McNagny SE. Obstacles predicting lack of a regular provider and delays in seeking care for patients at an urban public hospital. JAMA. 1994;271:1931–3. [PubMed] [Google Scholar]
- 26.Auerbach AD, Hamel MB, Califf RM, et al. Patient characteristics associated with care by a cardiologist among adults hospitalized with severe congestive heart failure. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Coll Cardiol. 2000;36:2119–25. doi: 10.1016/s0735-1097(00)01005-6. [DOI] [PubMed] [Google Scholar]
- 27.Rathore SS, Masoudi FA, Wang Y, et al. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006;152:371–8. doi: 10.1016/j.ahj.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chaturvedi N, Stephenson JM, Fuller JH. The relationship between socioeconomic status and diabetes control and complications in the EURODIAB IDDM Complications Study. Diabetes Care. 1996;19:423–30. doi: 10.2337/diacare.19.5.423. [DOI] [PubMed] [Google Scholar]
- 29.Hypertension Detection and Follow-up Program Cooperative Group. Educational level and 5-year all-cause mortality in the Hypertension Detection and Follow-up Program. Hypertension. 1987;9:641–6. [PubMed] [Google Scholar]
- 30.Riedinger MS, Dracup KA, Brecht ML. Predictors of quality of life in women with heart failure. SOLVD Investigators. Studies of Left Ventricular Dysfunction. J Heart Lung Transplant. 2000;19:598–608. doi: 10.1016/s1053-2498(00)00117-0. [DOI] [PubMed] [Google Scholar]
- 31.Ross CE, Van WM. Education and the subjective quality of life. J Health Soc Behav. 1997;38:275–97. [PubMed] [Google Scholar]
- 32.Vinson JM, Rich MW, Sperry JC, Shah AS, McNamara T. Early readmission of elderly patients with congestive heart failure. J Am Geriatr Soc. 1990;38:1290–5. doi: 10.1111/j.1532-5415.1990.tb03450.x. [DOI] [PubMed] [Google Scholar]
- 33.Chin MH, Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Health. 1997;87:643–8. doi: 10.2105/ajph.87.4.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeWalt DA, Malone RM, Bryant ME, et al. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Michalsen A, Konig G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998;80:437–41. doi: 10.1136/hrt.80.5.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Plavinski SL, Plavinskaya SI, Klimov AN. Social factors and increase in mortality in Russia in the 1990s: prospective cohort study. BMJ. 2003;326:1240–2. doi: 10.1136/bmj.326.7401.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ingelsson E, Lind L, Arnlov J, Sundstrom J. Socioeconomic factors as predictors of incident heart failure. J Card Fail. 2006;12:540–5. doi: 10.1016/j.cardfail.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 38.Grundy SM, Balady GJ, Criqui MH, et al. Guide to primary prevention of cardiovascular diseases. A statement for healthcare professionals from the Task Force on Risk Reduction. American Heart Association Science Advisory and Coordinating Committee. Circulation. 1997;95:2329–31. doi: 10.1161/01.cir.95.9.2329. [DOI] [PubMed] [Google Scholar]