Abstract
Background: The rates of epidural steroid injections have increased dramatically over time, with conflicting evidence regarding the efficacy of epidural steroid injections for the treatment of various low-back pain disorders. Given the uncertainty about their role, we sought to evaluate the geographic variation in the use of epidural steroid injections for low back pain within the United States. We also sought to determine whether greater rates of epidural steroid injections are associated with lower rates of lumbar surgery.
Methods: We used the 2001 Medicare Physician Part-B claims to examine the geographic variation in the use of epidural steroid injections. Current Procedural Technology codes were used to identify the number of procedures performed as well as the percentage of injections that were fluoroscopically guided. Procedure rates were analyzed with use of several geographic indicators, including state, United States Census Bureau regions (Northeast, South, Midwest, and West), and health referral regions as defined by the Dartmouth Atlas of Health Care.
Results: In 2001, there was a 7.7-fold difference between the state with the lowest rate (Hawaii at 5.2 per 1000) and the state with the highest rate (Alabama at 39.9 per 1000). The variation among health referral regions, which are smaller in size, was even greater, with an 18.4-fold difference from 5.6 per 1000 in Honolulu, Hawaii, to 103.6 per 1000 in Palm Springs, California. Higher statewide rates of epidural steroid injections were associated with significantly higher rates of lumbar surgery (p = 0.001). In areas with high injection rates, a significantly higher percentage of patients who sought care for low back pain received injections (p < 0.001). In addition, in areas with high injection rates, a significantly higher percentage of patients who presented with low back pain received both injections and lumbar surgery within the same year (p < 0.001).
Conclusions: There is substantial geographic variation in the rates of epidural steroid injections within the United States. Southern states tend to have the highest procedure rates, whereas northeastern states have the lowest. Injection rates are positively correlated with lumbar surgery rates; therefore, epidural steroid injections do not appear to be substituting for lumbar surgeries or reducing overall rates of lumbar surgery.
Geographic variation in the use of many medical services is well established, particularly among procedures with uncertainty in their clinical effectiveness1-4. The use of the diverse treatments for low back pain is highly variable. For example, lumbar surgery rates have been reported to vary substantially nationally and internationally5. Epidural steroid injection for low back pain is another treatment with uncertain effectiveness and without well-established guidelines for its use6. The success rate of epidural steroid injection has been reported to range from 18% to 90%, depending on methodology, outcome measures, and technique7-14. Randomized trials have had conflicting conclusions15,16. Nonetheless, this procedure has developed widespread acceptance and rapid increases in use6.
Given the variable success of surgery for lumbar spine disorders, less invasive and more cost-effective treatments are commonly sought to treat low back pain and sciatica17. Epidural steroid injections are often used as a less invasive alternative to lumbar surgery in patients with radiculopathy and other low-back pain disorders18. Epidural steroid injections can provide temporary pain relief to a subset of patients, and they are used for a variety of reasons. They may be used in an effort to avoid surgery by providing pain relief during the natural recovery from injury or to extend the period of time before a patient undergoes surgery. Understanding patterns of the use of epidural steroid injections across geographic regions can provide insight into variations in clinical decision-making. In this study, we sought to examine the patterns of the use of epidural steroid injections across geographic regions and to explore the relationship between the use of epidural steroid injections and lumbar surgery in actual clinical practice. We hypothesized that there would be substantial variation in the use of epidural steroid injections among both large (that is, region and statewide) and small (that is, health referral regions) geographic regions. We also hypothesized that regions with high epidural steroid injection rates would have lower lumbar surgery rates and that epidural steroid injection use in a geographic region would be positively correlated with the physician supply.
Materials and Methods
We used the 2001 standard 5% national sample of the U.S. Centers for Medicare and Medicaid Services (CMS) Physician Part-B outpatient billing claims. This dataset is a sample of patients enrolled in the fee-for-service Medicare program based on the selection of records with specific numbers in positions 8 and 9 of the health insurance claim number and is generated by CMS. This CMS 5% sample dataset is therefore unbiased and unpredictable in terms of any patient characteristics, but it does allow for tracking patients over time and across datasets. CMS makes this 5% sample available to researchers, as the 100% dataset is so large that it is not feasible to use for research purposes. Only patients who were sixty-five years old or older were included in this analysis, for consistency with prior studies on degenerative low-back pain treatments in the Medicare population5,19. We also included only persons with continuous enrollment during the study year in order to have a stable population to study. Injection rates were calculated with use of the total number of injections performed on eligible enrollees with continuous enrollment during the study year in the numerator and the total number of eligible enrollees with continuous enrollment during the study period in the denominator. Injection rates as reported represent the number of injections performed per 1000 Medicare enrollees. As persons in this sample may have received more than one injection during the study year, we also reported the number of persons receiving injections per 1000 Medicare enrollees. This analysis was completed in order to determine if the areas with a high rate of injections had a high rate because injections were performed on a higher number of people or if the rate was high because more injections were performed per person.
The 2001 Current Procedural Terminology (CPT) procedure codes for lumbar epidural steroid injections (62311 and 64483) were used to select cases for inclusion in this study20. Cases of patients who had lumbar surgery were identified with use of a previously described algorithm21. Patients with low back pain were defined as patients with any claim in the Medicare dataset with an International Classification of Diseases, Ninth Revision (ICD-9)22 diagnosis code for a low-back pain disorder based on a previously described algorithm6 and therefore represent those patients with low back pain who sought medical care for low back pain. Postal (ZIP) codes were used to determine the geographic location where the procedure was performed. Procedure rate variations were analyzed by state, U.S. Census Bureau definitions of regions (Northeast, South, Midwest, and West), and the Dartmouth Atlas of Health Care's previously defined health referral regions23. There are 306 health referral regions throughout the United States created to represent smaller health markets. Each represents a region that provides tertiary care services and typically represents a city and the surrounding areas. Physician supply was determined by counting individual provider codes on the injection claims. The number of different providers identified in each region was totaled to calculate the number of “injection providers” per 1000 Medicare beneficiaries within geographic regions. Providers and provider specialties were identified with use of the provider code and the specialty code on each claim. Human subjects approval was obtained through the University of Washington prior to the start of this study. Most of the data analyses were descriptive. Rates of injections were correlated with surgical rates, physician supply, and other variables with use of Pearson correlations. When variables were not distributed normally and variances were large, nonparametric correlation tests were used (Spearman rank coefficient). A p value of <0.05 was considered significant.
Results
Epidural Steroid Injection Rates
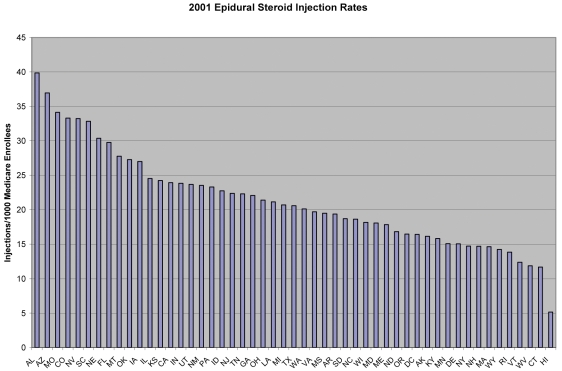
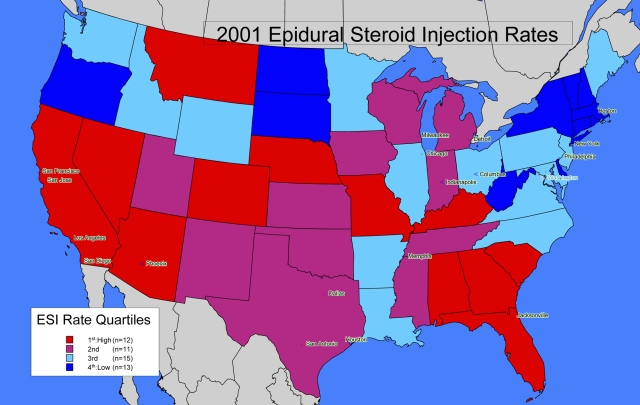
In 2001, there was a 7.7-fold difference between the state with the lowest rate (Hawaii at 5.2 per 1000) and the state with the highest rate (Alabama at 39.9 per 1000) (Fig. 1-A). Eight states had injection rates of >25% above the national average of 26.5 per 1000. The statewide variations are graphically demonstrated in the map of the contiguous United States, with each quartile of rates depicted by a different color (Fig. 1-B). Both Hawaii, with the lowest injection rate, and Alaska, with the thirteenth lowest, are in the lowest quartile (dark blue) but are not represented in this map of the contiguous United States.
Fig. 1-A.
Variations in the use of epidural steroid injections in the United States in 2001.
Fig. 1-B.
Map showing the statewide variations in the use of epidural steroid injections (ESI) in 2001.
Among census regions, the Northeast had the lowest injection rates and the South had the highest rates overall, and these rates were different from each other (p = 0.003). The injection rates in the South, Midwest, and West were not significantly different from one another.
The variation among health referral regions, which are smaller in size, was even greater, with an 18.4-fold difference from 5.6 per 1000 in Honolulu, Hawaii, to 103.6 per 1000 in Palm Springs, California (Table I). Of note, one health referral region recorded no injections and four health referral regions had fewer than ten recorded procedures during the study period, and these health referral region data are not presented individually to maintain confidentiality. Seventy-one of the 306 health referral regions had injection rates of >25% above the national average of 26.5 per 1000.
TABLE I.
Percentages of Medicare Enrollees Receiving Epidural Steroid Injections, Lumbar Surgery, or Both, in 2001
| Percentage of Patients with Back Pain Receiving Various Treatments in 2001*
|
||||
|---|---|---|---|---|
| Health Referral Region† | Epidural Steroid Injections per 1000 Enrollees | Epidural Steroid Injections | Lumbar Surgery | Epidural Steroid Injection and Surgery |
| Top 20 health referral regions | ||||
| Palm Springs, CA | 103.6 | 16.5 | 2.9 | 1.4 |
| Pueblo, CO | 79.2 | 11.8 | 0.0 | 0.0 |
| Mobile, AL | 68.8 | 14.9 | 2.6 | 0.6 |
| Charleston, SC | 61.8 | 10.9 | 1.6 | 0.5 |
| Abilene, TX | 59.1 | 9.8 | 0.8 | 0.2 |
| Fort Lauderdale, FL | 57.5 | 9.3 | 1.7 | 0.5 |
| Dubuque, IA | 55.4 | 12.4 | 2.8 | 1.5 |
| Kansas City, MO | 55.2 | 7.0 | 1.2 | 0.3 |
| Houma, LA | 52.2 | 7.5 | 0.5 | 0.3 |
| Fort Myers, FL | 52.0 | 9.2 | 3.0 | 0.5 |
| San Angelo, TX | 51.3 | 10.6 | 3.1 | 1.1 |
| Pensacola, FL | 50.4 | 8.9 | 3.8 | 0.5 |
| Columbia, MO | 49.9 | 8.9 | 1.3 | 0.4 |
| Waterloo, IA | 49.0 | 6.2 | 3.1 | 1.0 |
| Hattiesburg, MS | 48.3 | 8.3 | 1.1 | 0.5 |
| Greeley, CO | 47.4 | 7.6 | 2.2 | 0.4 |
| Tuscaloosa, AL | 47.0 | 10.8 | 0.4 | 0.0 |
| Hinsdale, IL | 46.6 | 10.0 | 2.4 | 0.9 |
| Hickory, NC | 45.4 | 6.5 | 2.1 | 0.3 |
| Newport News, VA | 44.5 | 10.7 | 4.1 | 1.1 |
| Lowest 20 health referral regions | ||||
| Dearborn, MI | 11.76 | 1.9 | 1.7 | 0.07 |
| Paducah, KY | 11.75 | 1.8 | 0.7 | 0.08 |
| Lebanon, NH | 11.61 | 3.4 | 0.8 | 0.21 |
| Temple, TX | 11.51 | 3.7 | 1.2 | 0.00 |
| Rochester, MN | 11.38 | 2.7 | 2.2 | 0.09 |
| Pontiac, MI | 11.35 | 2.3 | 1.8 | 0.32 |
| Kettering, OH | 11.17 | 1.8 | 0.8 | 0.12 |
| Duluth, MN | 10.97 | 2.0 | 2.4 | 0.21 |
| Waco, TX | 10.5 | 2.1 | 2.8 | 0.00 |
| Rochester, NY | 9.95 | 1.7 | 0.6 | 0.10 |
| Bronx, NY | 9.06 | 1.0 | 0.2 | 0.00 |
| Longview, TX | 8.97 | 1.2 | 0.8 | 0.18 |
| Salem, OR | 8.53 | 3.2 | 5.1 | 0.33 |
| St. Joseph, MI | 8.46 | 1.9 | 0.5 | 0.00 |
| Huntington, WV | 8.37 | 1.7 | 0.8 | 0.10 |
| Lexington, KY | 7.26 | 1.0 | 1.0 | 0.12 |
| Charleston, WV | 7.04 | 1.6 | 0.5 | 0.09 |
| Sayre, PA | 6.96 | 0.8 | 0.8 | 0.00 |
| Honolulu, HI | 5.64 | 2.2 | 0.6 | 0.00 |
Data show the percentage of enrollees with low back pain receiving one or more epidural steroid injections in 2001, the total percentage of enrollees with low back pain receiving one or more lumbar operations in 2001, as well as the percentage of enrollees with low back pain who received one or more epidural steroid injections followed by a subsequent lumbar surgery within a year of the first injection.
The highest and lowest health referral regions are given in terms of overall epidural steroid injection rates.
The analysis was also performed with use of the number of persons receiving injections per 1000 Medicare enrollees rather than the number of actual injections performed per 1000 enrollees (that is, accounting for the fact that a person could and often did receive multiple injections during the study year). We found a high degree of correlation between the “person” rates (that is, the number of persons receiving injections per 1000 enrollees) and the “injection” rates (that is, the total number of injections performed per 1000 enrollees) (r = 0.91, p < 0.001). Thus, in areas with high injection rates, more persons received injections (with population size differences controlled for by calculating rates). Along with this, we found a correlation between injection rates (and “person” rates) and the average number of injections being performed per patient (r = 0.392, p < 0.001). Therefore, it appears that areas with high injection rates have high rates because more injections are performed per patient and more patients are receiving injections.
Lumbar Surgery Rates
Statewide lumbar surgery rates also varied widely, with an 11.5-fold difference between the state with the highest rate (Nebraska, with 6.9 per 1000 Medicare enrollees) and the state with the lowest rate (Vermont, with 0.6 per 1000 Medicare enrollees). Among health referral regions, lumbar surgery rates (0.6 to 11.6 per 1000 enrollees) also varied to a similar degree as that of injection rates. Statewide rates of epidural steroid injections were positively correlated with lumbar surgery rates (Pearson correlation coefficient, r = 0.299; p = 0.001). There was a weaker positive correlation between surgery rates and epidural steroid injection rates at the health referral region level (Pearson correlation coefficient, r = 0.21; p < 0.001). To account for the fact that persons can and do receive more than one injection or operation, we also calculated the number of persons receiving surgery per 1000 enrollees and the number of persons receiving injections per 1000 enrollees. Using the rates at the person level, we found no difference in correlations compared with those between the rates calculated at the procedure level.
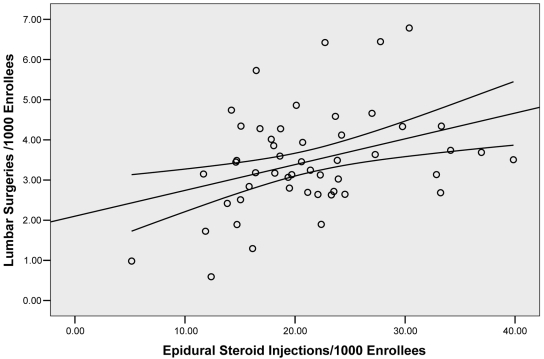
We also found a moderate correlation between injection rates and the percentage of persons who had one injection or more as well as surgery in the year 2001 (Pearson correlation coefficient, r = 0.41; p < 0.001) (Table I), as well as a correlation between injection rates and rates of lumbar surgeries within one year following an epidural steroid injection (r = 0.58, p < 0.001) (Fig. 2). Therefore, in areas with a high injection rate, persons were more likely to undergo both epidural steroid injections as well as a subsequent lumbar surgery.
Fig. 2.
This graph depicts the relationship between state-level epidural steroid injection (ESI) rates and lumbar surgery rates. The lumbar surgery rates include only the persons who underwent surgery within one year of receiving an epidural steroid injection. This graphically depicts the moderate correlation (r = 0.59, p < 0.001) between epidural steroid injection rates and subsequent surgery rates. The circles indicate states, the middle line indicates the fit line for state data, and the two outer lines indicate the 95% confidence interval.
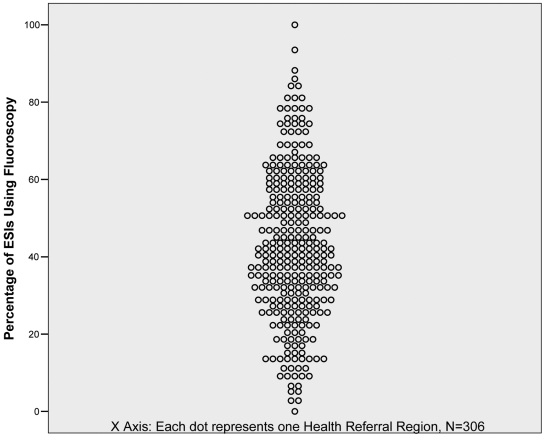
Fluoroscopy Use
Only 7% of the injections performed in Vermont were fluoroscopically guided compared with 87% of the injections in Wyoming. Nationally, 42% of the injections were performed with use of fluoroscopy. The use of fluoroscopy varied even more widely among health referral regions, ranging from 0% to 100% (Fig. 3). Fluoroscopy use was not correlated with injection rates at either the statewide level (Spearman rank coefficient, ρ = 0.056; p = 0.70) or the regional level (Spearman rank coefficient, ρ = −0.01; p = 0.86).
Fig. 3.
Variation in fluoroscopy use by health referral region. ESI = epidural steroid injections.
Physician Supply
Physician supply was determined by counting the number of distinct providers who performed the injections (“injection providers”) in each health referral region during the year 2001. The density of injection providers was determined by calculating the number of injection providers per 1000 Medicare enrollees at the state and health referral region level. Health referral regions with high rates of steroid injections were associated with higher densities of physicians performing the procedures (r = 0.79, p < 0.001). The physician supply was further examined in two distinct health referral regions, one with a very high injection rate and another with a very low injection rate. In the health referral region with a high injection rate, there were twenty-five physicians performing injections per 1000 enrollees. However, only a small percentage of physicians (3.4%, or two physicians) accounted for 43% of all injections performed, and one of those two physicians accounted for 30% of all injections performed in this area. In contrast, in a health referral region with a low injection rate, there were fewer injection providers (3.8 per 1000 enrollees) and two physicians accounted for 39% of all injections performed in the area.
We also examined the number of injections provided per patient by individual providers to try to better understand the variation in practice patterns. There was an enormous range in the number of injections performed per patient by individual providers during the study year (range, one to forty injections per patient per year; median, 1.3 injections; mean [and standard deviation], 1.6 ± 0.9 injections). Only a very small percentage of physicians performed a large number of injections per patient per year, with only 0.06%, or twenty-four physicians, who performed ten or more injections per patient per year. Over 75% of physicians performed two or fewer injections per Medicare patient per year.
Comparison of Epidural Steroid Injection Rates and Low-Back Pain Rates
To determine whether high injection rates in certain geographic regions simply reflected the variable prevalence of low back pain, we standardized injection rates to eliminate the potential effects of these differences between health referral regions. We did this by calculating injections per 1000 patients with low back pain in each health referral region. We found that health referral regions with a high injection rate tended to have high rates whether the entire Medicare population was considered or just the subset of patients who sought care for low back pain (Spearman rank coefficient, ρ = 0.97; p < 0.001). We also found that, in health referral regions with a high injection rate, a substantially higher percentage of patients who sought care for low back pain received at least one epidural steroid injection during the study year (Pearson correlation coefficient, r = 0.84; p < 0.001). For example, in Palm Springs, California, the injection rate was the highest in the nation at 103.6 per 1000 Medicare enrollees and nearly 17% of all patients who sought care for low back pain received one injection or more. In contrast, in one of the areas with the lowest injection rates (Honolulu, Hawaii), <3% of the patients who sought care for low back pain received one injection or more. In addition, in high injection-rate areas, a higher percentage of patients who presented with low back pain also underwent lumbar surgery (Pearson correlation coefficient, r = 0.16; p = 0.006) and a higher percentage had one injection or more as well as surgery in the year 2001 (Pearson correlation coefficient, r = 0.41; p < 0.001) (Table I).
Discussion
Previous studies have documented substantial geographic variation in several medical procedures, including lumbar surgery for low back pain3. We found that there was large geographic variation in the rates of epidural steroid injections within the United States. The extent of this variation is similar to the variation in the rates of lumbar surgery. We found that injection rates were highest in the southern states, whereas lumbar surgery rates were highest in the Midwest. Northeastern states had the lowest rates of both injections and lumbar surgeries. High injection rates were not simply a result of a higher prevalence of back pain in certain geographic regions. Areas with high injection rates tended to have higher rates whether the entire Medicare population was considered or just the patients who sought care for low back pain.
Contrary to our original hypothesis, there was a modest positive correlation between lumbar surgery and the use of epidural steroid injections among Medicare patients with low back pain, such that states and health referral regions with higher injection rates also had higher lumbar surgery rates. In addition, in the areas with high injection rates, a larger percentage of patients with low back pain received at least one epidural steroid injection as well as a subsequent lumbar surgery within the same year. Thus, it does not appear that the epidural steroid injections were substituting for lumbar surgeries or reducing overall rates of lumbar surgery.
The use of fluoroscopy throughout the country at the statewide level as well as at the regional level was also extremely variable, ranging from 0% to 100%. Fluoroscopy use did not correlate with injection rates at either the statewide level or the regional level.
As we hypothesized, areas with high injection rates were associated with higher densities of injection providers, or physicians performing the injections. In both the health referral regions with high injection rates and those with low injection rates, a small percentage of physicians accounted for a substantial portion of the injections performed. This suggests that some of the regional variations may be due to physician supply as well as local practice conventions, training styles, or other factors.
There are several limitations to our study. This study examines Medicare patients over the age of sixty-five years with degenerative spinal disorders. The use of steroid injections in this group may be different from that in a younger group with different causes of low back pain. Since billings for patients in the Medicare health maintenance organization are not captured in our dataset, our findings also cannot be generalized to this group. Another limitation is that some of the variation may be related to coding errors, diagnostic ambiguity, or local conventions24,25. However, as the billing claims are used for reimbursement and are subject to regular audits, providers are obligated to report procedures accurately and are subject to substantial penalties if procedure codes are not reported properly25. Studies that have examined the accuracy of Medicare claims data for other diagnoses and procedures have generally found that the claims data have a good deal of accuracy in capturing procedures and diagnosis codes, with positive predictive values ranging from 62% to 95%26-30. However, on the basis of these previous studies of other diagnoses, such as renal disease, cancer, and arthritis, the claims data may be less accurate for determining disease prevalence31,32. These studies have demonstrated that there are frequent omissions in the claims data in terms of diagnoses, but that the diagnoses captured in the Medicare claims data are relatively accurate. In the current study, we primarily focused on procedure rates and thus it is unlikely that potential diagnostic inaccuracies affected the analysis of geographic variations in the use of injections. 
Acknowledgments
Note: The authors thank William Kreuter, programmer, for his contribution to the data acquisition and analysis.
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the Intramural Research Program of the National Institutes of Health, Clinical Research Center, Rehabilitation Medicine Scientist Training (RMSTP) K12 Program (National Institutes of Health grant 2K12HD001097-11) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (National Institutes of Health grant P60 AR 48093), National Institutes of Health. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. A commercial entity (Synthes) paid or directed in any one year, or agreed to pay or direct, benefits in excess of $10,000 to a research fund, foundation, division, center, clinical practice, or other charitable or nonprofit organization with which one or more of the authors, or a member of his or her immediate family, is affiliated or associated.
Investigation performed at the University of Washington, Seattle, Washington
References
- 1.Irwin ZN, Hilibrand A, Gustavel M, McLain R, Shaffer W, Myers M, Glaser J, Hart RA. Variation in surgical decision making for degenerative spinal disorders. Part I: lumbar spine. Spine. 2005;30:2208-13. [DOI] [PubMed] [Google Scholar]
- 2.Irwin ZN, Hilibrand A, Gustavel M, McLain R, Shaffer W, Myers M, Glaser J, Hart RA. Variation in surgical decision making for degenerative spinal disorders. Part II: cervical spine. Spine. 2005;30:2214-9. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein JN, Bronner KK, Morgan TS, Wennberg JE. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood). 2004;Suppl Web Exclusive:VAR81-9. [DOI] [PubMed]
- 4.Sung JC, Curtis LH, Schulman KA, Albala DM. Geographic variations in the use of medical and surgical therapies for benign prostatic hyperplasia. J Urol. 2006;175:1023-7. [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139-46. [DOI] [PubMed] [Google Scholar]
- 6.Friedly J, Chan L, Deyo R. Increases in lumbosacral injections in the Medicare population: 1994 to 2001. Spine. 2007;32:1754-60. [DOI] [PubMed] [Google Scholar]
- 7.Koes BW, Scholten RJ, Mens JM, Bouter LM. Efficacy of epidural steroid injections for low-back pain and sciatica: a systematic review of randomized clinical trials. Pain. 1995;63:279-88. [DOI] [PubMed] [Google Scholar]
- 8.Leonardi M, Pfirrmann CW, Boos N. Injection studies in spinal disorders. Clin Orthop Relat Res. 2006;443:168-82. [DOI] [PubMed] [Google Scholar]
- 9.Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil. 1998;79:1362-6. [DOI] [PubMed] [Google Scholar]
- 10.Manchikanti L, Singh V, Kloth D, Slipman CW, Jasper JF, Trescot AM, Varley KG, Atluri SL, Giron C, Curran MJ, Rivera J, Baha AG, Bakhit CE, Reuter MW. Interventional techniques in the management of chronic pain: part 2.0. Pain Physician. 2001;4:24-96. [PubMed] [Google Scholar]
- 11.Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, Kloth DS, Trescot AM, Hansen HC, Falasca TD, Racz GB, Deer TR, Burton AW, Helm S, Lou L, Bakhit CE, Dunbar EE, Atluri SL, Calodney AK, Hassenbusch SJ, Feler CA. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2003;6:3-81. [PubMed] [Google Scholar]
- 12.Papagelopoulos PJ, Petrou HG, Triantafyllidis PG, Vlamis JA, Psomas-Pasalis M, Korres DS, Stamos KG. Treatment of lumbosacral radicular pain with epidural steroid injections. Orthopedics. 2001;24:145-9. [DOI] [PubMed] [Google Scholar]
- 13.Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, Goette K. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000;82:1589-93. [DOI] [PubMed] [Google Scholar]
- 14.Weinstein SM, Herring SA, Derby R. Contemporary concepts in spine care. Epidural steroid injections. Spine. 1995;20:1842-6. [DOI] [PubMed] [Google Scholar]
- 15.Valat JP, Giraudeau B, Rozenberg S, Goupille P, Bourgeois P, Micheau-Beaugendre V, Soubrier M, Richard S, Thomas E. Epidural corticosteroid injections for sciatica: a randomised, double blind, controlled clinical trial. Ann Rheum Dis. 2003;62:639-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weinstein SM, Herring SA; NASS. Lumbar epidural steroid injections. Spine J. 2003;3(3 Suppl):37S-44S. [DOI] [PubMed] [Google Scholar]
- 17.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363-70. [DOI] [PubMed] [Google Scholar]
- 18.Nelson DA, Landau WM. Intraspinal steroids: history, efficacy, accidentality, and controversy with review of United States Food and Drug Administration reports. J Neurol Neurosurg Psychiatry. 2001;70:433-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ciol MA, Deyo RA, Kreuter W, Bigos SJ. Characteristics in Medicare beneficiaries associated with reoperation after lumbar spine surgery. Spine. 1994;19:1329-34. [DOI] [PubMed] [Google Scholar]
- 20.American Medical Association. Current procedural terminology. Chicago: American Medical Association; 2001.
- 21.Cherkin DC, Deyo RA, Volinn E, Loeser JD. Use of the International Classification of Diseases (ICD-9-CM) to identify hospitalizations for mechanical low back problems in administrative databases. Spine. 1992;17:817-25. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. International statistical classification of diseases and related health problems (ICD). 11th revision. Geneva, Switzerland: World Health Organization; 2008.
- 23.Weinstein JN, Birkmeyer JD. Dartmouth atlas of musculoskeletal health care. Chicago: American Hospital Association Press; 2000. [PubMed]
- 24.Iezzoni LI, Moskowitz MA. The clinical impact of DRG-based physician reimbursement. Report prepared for the Health Care Financing Administration under Cooperative Agreement Number 18-C-98526/1-01. Boston: Health Care Research Unit, Boston University Medical Center; 1984.
- 25.Chan L, Houck P, Prela CM, MacLehose RF. Using medicare databases for outcomes research in rehabilitation medicine. Am J Phys Med Rehabil. 2001;80:474-80. [DOI] [PubMed] [Google Scholar]
- 26.Losina E, Barrett J, Baron JA, Katz JN. Accuracy of Medicare claims data for rheumatologic diagnoses in total hip replacement recipients. J Clin Epidemiol. 2003;56:515-9. [DOI] [PubMed] [Google Scholar]
- 27.Noyes K, Liu H, Holloway R, Dick AW. Accuracy of Medicare claims data in identifying Parkinsonism cases: comparison with the Medicare current beneficiary survey. Mov Disord. 2007;22:509-14. [DOI] [PubMed] [Google Scholar]
- 28.Katz JN, Barrett J, Liang MH, Bacon AM, Kaplan H, Kieval RI, Lindsey SM, Roberts WN, Sheff DM, Spencer RT, Weaver AL, Baron JA. Sensitivity and positive predictive value of Medicare Part B physician claims for rheumatologic diagnoses and procedures. Arthritis Rheum. 1997;40:1594-600. [DOI] [PubMed] [Google Scholar]
- 29.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148:99-104. [DOI] [PubMed] [Google Scholar]
- 30.Mouchawar J, Byers T, Warren M, Schluter WW. The sensitivity of Medicare billing claims data for monitoring mammography use by elderly women. Med Care Res Rev. 2004;61:116-27. [DOI] [PubMed] [Google Scholar]
- 31.Kern EF, Maney M, Miller DR, Tseng CL, Tiwari A, Rajan M, Aron D, Pogach L. Failure of ICD-9-CM codes to identify patients with comorbid chronic kidney disease in diabetes. Health Serv Res. 2006;41:564-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mitchell JB, Bubolz T, Paul JE, Pashos CL, Escarce JJ, Muhlbaier LH, Wiesman JM, Young WW, Epstein RS, Javitt JC. Using Medicare claims for outcomes research. Med Care. 1994;32(7 Suppl):JS38-51. [PubMed] [Google Scholar]