Abstract
Objective
To compare immediate with delayed prescribing of antibiotics for acute otitis media.
Design
Open randomised controlled trial.
Setting
General practices in south west England.
Participants
315 children aged between 6 months and 10 years presenting with acute otitis media.
Interventions
Two treatment strategies, supported by standardised advice sheets—immediate antibiotics or delayed antibiotics (antibiotic prescription to be collected at parents' discretion after 72 hours if child still not improving).
Main outcome measures
Symptom resolution, absence from school or nursery, paracetamol consumption.
Results
On average, symptoms resolved after 3 days. Children prescribed antibiotics immediately had shorter illness (−1.1 days (95% confidence interval −0.54 to −1.48)), fewer nights disturbed (−0.72 (−0.30 to −1.13)), and slightly less paracetamol consumption (−0.52 spoons/day (−0.26 to −0.79)). There was no difference in school absence or pain or distress scores since benefits of antibiotics occurred mainly after the first 24 hours—when distress was less severe. Parents of 36/150 of the children given delayed prescriptions used antibiotics, and 77% were very satisfied. Fewer children in the delayed group had diarrhoea (14/150 (9%) v 25/135 (19%), χ2=5.2, P=0.02). Fewer parents in the delayed group believed in the effectiveness of antibiotics and in the need to see the doctor with future episodes.
Conclusion
Immediate antibiotic prescription provided symptomatic benefit mainly after first 24 hours, when symptoms were already resolving. For children who are not very unwell systemically, a wait and see approach seems feasible and acceptable to parents and should substantially reduce the use of antibiotics for acute otitis media.
Introduction
Otitis media (or, more descriptively, acute red ear) is one of the commonest acute respiratory conditions managed in primary care, yet treatment is controversial.1–3 Most children attending their doctor will be prescribed antibiotics, but evidence from systematic review suggests that these provide only marginal benefit.4 There is, however, considerable debate as to the precise nature and magnitude of benefit from antibiotics. The largest trial from primary care gave conflicting results5: use of antibiotics led to one day less of crying and one day less away from school, suggesting they have important benefits, but there was little difference in analgesic (paracetamol) consumption, which suggests that the perceived pain and distress may be little affected by antibiotics.
If the duration of illness is reduced when antibiotics are prescribed the symptomatic benefit and distress in both treated and untreated children requires further clarification. The benefit of prescribing antibiotics must also be balanced against the increased likelihood of side effects such as diarrhoea.4 Furthermore, the effect of prescribing antibiotics on belief in and expectation for antibiotics must be quantified: the cycle of prescribing and expectation is likely to encourage attendance in future episodes, increase pressure on doctors to prescribe, increase antibiotic use,6–9 and increase the danger of antibiotic resistance.3,10
If antibiotics are not to be prescribed initially then what alternatives exist? Evidence from a cohort of 7000 children from Holland suggests that waiting for 72 hours with symptomatic treatment only is safe,11 but a blanket approach of no treatment may have dangers: the only child to develop mastoiditis was not given antibiotics after 72 hours despite remaining unwell.11 Although there are case series describing the acceptability of delayed prescribing,12 it has not been subject to a randomised controlled trial. The implications of this approach are unclear for both doctors and patients, including what effect this might have on patients' beliefs and expectation for antibiotics.
We therefore conducted an open randomised trial comparing standard management (immediate antibiotics) with a 72 hour wait and see policy. To assess efficacy, placebo controlled trials provide the best evidence. However, to assess the practical implications of prescribing strategies such as a wait and see approach (for example, collection and use of prescriptions, satisfaction, belief in antibiotics), open trials are also important. The main disadvantage of an open trial is the possibility of a placebo effect favouring antibiotics. This can be minimised, however, by using a structured management approach: the doctor is used to support the proposed strategy, thus acting like a “placebo” in all groups.
Methods
Setting
We contacted 93 general practices in three health authorities in south west England close to the administrative centre. Forty two doctors expressed interest and recruited patients for the study: 26/42 (62%) were from training practices, 25 (60%) managed their own budgets (fundholders), and 14 (33%) were in mixed urban and rural (as opposed to urban) practice settings.
Sample and diagnostic criteria
The precise diagnostic criteria for acute otitis media differ according to national perspectives and specialty.1,5,13–16 Diagnosis of otitis media is uncontroversial when florid clinical signs are present (dull drum with severe inflammation, bulging drum, or perforation with discharge), but some authorities have advocated pneumatic otoscopy, particularly for early presentations without florid clinical signs.13,14 Although the reliability of pneumatic otoscopy is established for chronic otitis media with effusion,15 a systematic review of its diagnostic accuracy found no evidence of its validity for acute otitis media compared with microbiological or virological evidence of infection, nor its reliability in primary care.15 Furthermore, pneumatic otoscopy is not used routinely in Europe in diagnosing acute otitis media in primary care, where the vast majority of cases are managed.1,5
Since our study was intended to be a pragmatic effectiveness trial—that is, to inform clinical decision making in everyday practice—our inclusion criteria had to mimic the conditions of practice in Britain, where diagnosis is made on an acute history and appearances of the tympanic membrane.1,5 We used similar clinical criteria to those of an earlier trial to facilitate comparison of results.5 Children were eligible for inclusion if they were aged 6 months to 10 years and attended their doctor with acute otalgia and otoscopic evidence of acute inflammation of the ear drum (dullness or cloudiness with erythema, bulging, or perforation). To standardise agreement about physical signs according to recommendations for research in acute otitis media,16 we sent a sheet of clinical photographs showing examples of each physical sign (degrees of erythema, bulging drum, etc) to each participating doctor. For comparability of results, we used the same photographs as were used in an earlier trial in primary care.5 When children were too young for otalgia to be specifically documented from their history (under 3 years old) then otoscopic evidence alone was a sufficient entry criterion. To assess the influence of our pragmatic inclusion criteria (that is, the possible diagnostic imprecision, particularly when florid clinical signs were absent), we assessed treatment interaction according to whether florid clinical signs were present (see below).
Exclusion criteria were otoscopic appearances consistent with crying or a fever alone (pink drum alone); appearances and history more suggestive of otitis media with effusion and chronic suppurative otitis media; serious chronic disease (such as cystic fibrosis, valvular heart disease); use of antibiotics for ear infections within the previous two weeks; previous complications (septic complications, hearing impairment); and if the child was too unwell to be left to wait and see (for example, high fever, floppy, drowsy, not responding to antipyretics).
Sample size
We calculated samples size (for 80% power and 95% confidence) using means and standard deviations for the main outcomes from a previous trial (mean consumption of analgesics in the week after seeing the doctor, number of days crying, and number of days off school)5 and to detect a 15% difference in the number of children better by 72 hours after seeing their doctor. The limiting factor in the sample size calculation was the number better 72 hours after seeing the doctor, which required 233 children, or 291 children in total, allowing for up to 20% loss to follow up.
Intervention
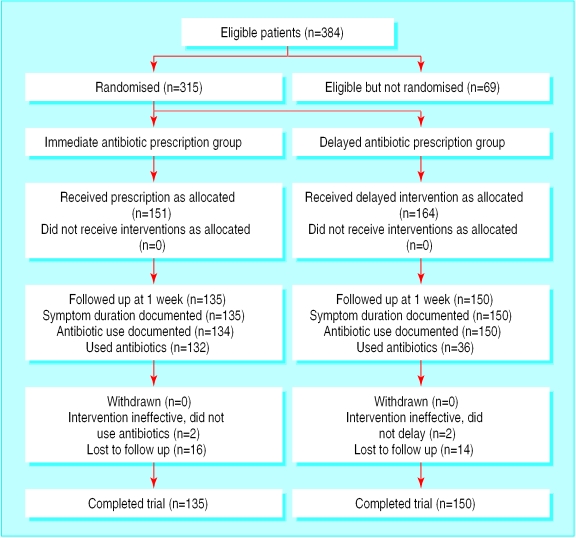
After parents had given written consent, patients were randomised to a group when their doctor opened a sealed numbered opaque envelope containing an advice sheet for one of two treatments (see fig 1).
Figure 1.
Flow of participants through trial
Immediate treatment with antibiotics—Patients were prescribed amoxicillin syrup, 125 mg in 5 ml, three times daily, 100 ml in total, according to British National Formulary guidelines for the age range of children included this study, and for exact comparability with a previous trial.5 The few patients allergic to penicillin were prescribed erythromycin 125 mg in 5 ml four times daily for 1 week (since this was a trial of common prescribing strategies and not of a particular antibiotic).
Delayed treatment with antibiotics—Similar antibiotics were prescribed, but parents were asked to wait for 72 hours after seeing the doctor before considering using the prescription. Parents were instructed that if their child still had substantial otalgia or fever after the 72 hours or was not starting to get better then they should come and collect the prescription for antibiotics, which was left at the practice's reception. Although parents could come earlier, they were encouraged to try to wait the 72 hours. Parents were also advised to use the prescription if their child had a discharge for 10 days or more.
Each advice sheet listed several issues that the doctor had to deal with in the consultation, with suggested wordings. Doctors were not required to use the wording verbatim, but they were asked to tick boxes by each statement to signify that they had dealt with that issue and then return the sheet to the administrative centre. The standardised advice in the sheets was designed to maximise the support and placebo effect for each strategy and to ensure some consistency in the advice given to each group no matter what the personal prescribing preference of the doctor. Those prescribed immediate antibiotics were advised that antibiotics could help symptoms settle and may prevent complications, and the importance of taking the full course was stressed. Those asked to delay using antibiotics were advised that antibiotics do not work very well and have disadvantages (side effects and resistance). For both groups, doctors emphasised the importance of paracetamol in full doses for relief of pain and fever. If parents reported that they were already using full doses of paracetamol they were advised to use ibuprofen as well if the child was over 1 year old. In both groups parents were asked to return to see their doctor after three months if they were concerned about their child's hearing.
Outcome measures
Doctor documentation sheet
—Doctors were asked to provide information on days of illness, physical signs, and antibiotic prescription.
Daily diary and questionnaire—Participants were asked to complete a daily diary of presence of symptoms (earache, unwell, sleep disturbance), perceived severity of pain (from 1 (no pain) to 10 (extreme pain)), number of episodes of distress, number of spoonfuls of liquid paracetamol used, and temperature (using the tempadot thermometer17) until children were asymptomatic and had finished their medication—similar to our previous use of diaries.6 Within three days of starting, participants were contacted by a research assistant to check that there were no problems with filling in the diary. Parents were also asked to use a six point Likert scale (extremely, very, moderately, slightly, not very, not at all) to answer written questions at the start of treatment about their worries and their satisfaction and at the end of treatment about antibiotic use and its perceived efficacy, their intention to consult their doctor in future, and time taken off work and school.6 In the minority of cases when we had not received a diary within two weeks of participants entering the study we telephoned them: most gave diary information over the telephone (n=66), but some (n=30) could not be contacted.
As in our previous study,6 we used diary information as the main outcome measure rather than assessment by an observer to minimise the intrusive nature of assessment in a pragmatic study where we wanted to assess perceptions in as realistic an environment as possible and because patients or their parents are best able to judge how unwell they are, how much pain they are in, and whether they are back to normal. We included perceived severity of pain and episodes of distress and disturbed sleep in the diary after piloting with 20 parents, who emphasised the importance of such outcomes to them.
Validity of outcomes
Likert scales and symptom duration
—We have shown the reliability and validity of the simple Likert scales used in an earlier study and the validity of information obtained for the minority who required a telephone reminder.6
Paracetamol use—We provided 14 consecutive subjects with preweighed bottles of paracetamol, which we collected at the end of the study and weighed again. We estimated the validity of reported paracetamol use by comparing diary responses with weighed paracetamol use. There was good agreement between estimated and actual use (rank correlation r=0.74), although in absolute terms parents slightly overestimated the amount they used (mean difference of estimated from actual=0.3 spoons (SD 0.8) per day). Mean daily paracetamol consumption also showed evidence of construct validity since it correlated with mean pain scores (r=0.54, P<0.01).
Numerical analogue scores, and reported distress— In 17 consecutive children with otitis media there was good agreement between parents' rating by numerical analogue score and children's own independent rating using four facial pictures illustrating level of pain (r=0.74).18 The validity of the numerical pain score is shown by good correlation of the mean score with both mean paracetamol consumption (r=0.54) and mean number of episodes of distress (r=0.62).19
Statistical analysis
We entered data on an intention to treat basis (based on patients' randomised group) and analysed it with SPSS.
Summarising group differences—Most of the outcomes had small ranges and low average values. Thus, although the data were skewed, the median and interquartile range provided a poor summary of the differences in group averages and distributions. Instead, we used the mean and mean differences for group summary statistics. This had the advantage (compared with the median or geometric mean) of allowing a direct comparison with the previous major trial in primary care5 and providing meaningful estimation at a group level of the benefit of antibiotics (for example, treating 10 children with antibiotics immediately will save 11 days of symptoms and result in five spoons less of paracetamol used).
Testing differences between groups—Since the t test is robust to assumptions about the normality of the underlying distribution for large numbers, we used it to compare means without assuming equality of variance. To check the assumption that statistical inference was robust to assumptions of normality, we also performed non-parametric tests (Mann-Whitney U test) for the main outcomes, which did not alter the inferences. We compared group percentages using the χ2 test.
Results
Recruitment rates and baseline characteristics
The 42 recruiting doctors identified 384 eligible children, of whom 69 were not recruited (fig 1): the commonest reasons were parental refusal or the doctor not having time. Table 1 shows the baseline characteristics of the 315 children recruited and randomised to the two groups: there were no significant group differences, suggesting no selection bias between groups.
Table 1.
Characteristics of children with acute otitis media on day of entry into study by treatment. Values are numbers (percentages) unless stated otherwise
| Characteristics | Antibiotic treatment allocated
|
Difference | |
|---|---|---|---|
| Immediate (n=151) | Delayed (n=164) | ||
| Mean (SE) prior duration of illness (days) | 1.48 (0.07) | 1.46 (0.10) | t=0.22, P=0.82 |
| Aged >3 years | 93 (62) | 93 (57) | χ2=0.68, P=0.41 |
| Perforated ear drum | 13 (9) | 11 (7) | χ2=0.41, P=0.42 |
| Bulging ear drum | 69 (46) | 77 (47) | χ2=0.01, P=1.00 |
| Red ear drum* | 115/147 (78) | 133/163 (82) | χ2=0.55, P=0.46 |
Erythema more than injection of malleus or rim.
Potential bias
Responder bias
Symptom duration was documented in 285 (90%) of the 315 children randomised: 135/151 (89%) of those allocated immediate antibiotics and 150/164 (91%) of those allocated delayed treatment. We received diaries for 219 (70%) of the children and obtained telephone information about duration of symptoms for a further 66 (21%). A comparison of the baseline information from the three types of responder (those who provided diaries, those who gave information by telephone, and those from whom no diary information could be collected) showed no evidence of significant bias between treatment groups (49%, 42%, and 53% respectively for immediate antibiotic group, χ2=1.2, P=0.54) or between patients by age (60%, 61%, and 57% for those aged ≥4 years, χ2=0.14, P=0.93) or severity of symptoms (8%, 5%, and 11% for those with a perforated drum, χ2=1.5, P=0.47; 46%, 50%, and 45% for those with a bulging drum, χ2=0.34, P=0.85).
Recruitment bias
We compared the characteristics of the 140 patients of high recruiting doctors (those who recruited >20 patients a year) with the 175 patients of low recruiting doctors (⩽20 patients a year). On average, high recruiting doctors recruited 36 patients a year (that is, most of the patients presenting to them with otitis media20). There was no evidence of bias in terms of patients' sex (52% and 47% respectively were boys, χ2=0.38, P=0.22) or presence of red ear drum (78% and 82% had erythema more than just peripheral injection and injection of the handle of the malleus, χ2=0.60, P=0.44) or bulging drum (46% and 47%, χ2=0.06, P=0.80).
Although high recruiters recruited more children aged ≤3 years (49% v 34%, χ2=6.86, P=0.01) and more with a perforated drum (12% v 5%, χ2=5.71, P=0.02), the differences are unlikely to affect the results significantly. The mean duration of illness in patients from high recruiting doctors was identical to that in patients from low recruiting doctors (both 3.1 days), and there was no evidence of a treatment interaction (that is, a significantly different treatment effect) in such patients for mean duration of illness (analysis of variance interaction term, F=2.15, P=0.14) or for those who were better within 72 hours (logistic regression interaction term, Wald test=0.58, P=0.63). Similarly there was no evidence of interaction between treatment and age (≤3 years v >3 years, interaction term t=1.4, P=0.17), degree of erythema of the drum (t=1.5, P=0.13), or bulging drum (t=0.14, P=0.89). When we considered only those patients recruited by high recruiting doctors, we found a similar pattern of results to those in the main analysis for all patients (see below): comparison of the two treatment groups showed that patients allocated immediate antibiotic had similar mean daily pain scores (difference 0.20, P=0.37) and mean daily episodes of distress (0.04, P=0.85) but consumed fewer spoons of paracetamol a day (−0.59, P=0.04), had fewer days of earache (−0.61, P=0.098), and had fewer disturbed nights (−0.78, P=0.012).
Group differences
Use and collection of antibiotic prescriptions
—We found good agreement between reported collection of antibiotic prescriptions and actual collection (κ=0.97, P<0.01) for the group allocated delayed antibiotic treatment. The patients allocated immediate antibiotic and those allocated delayed treatment were well differentiated in the number who took an antibiotic prescription from the consultation (151/151 v 2/164) and the number who reported using antibiotics at some stage during the illness (132/134 v 36/150). Of the 36 patients in the delayed treatment group who used antibiotics, 29 waited until two days after seeing their doctor before starting antibiotics, but only 11 waited until three days after seeing their doctor.
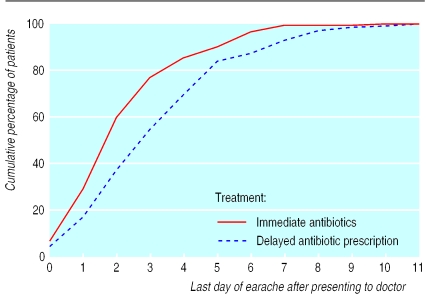
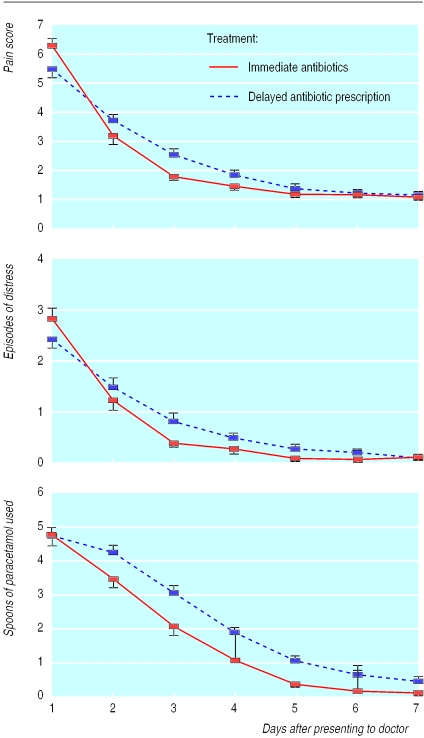
Symptoms and analgesia use—Figure 2 shows the difference in duration of symptoms in the two treatment groups, and tables 2 and 3 show the principal effects of treatment. There were significantly fewer days of discharge, less paracetamol consumption, fewer days when the child was reported as crying, and less night disturbance in the group allocated immediate antibiotics. Most of these differences, however, probably reflect modest symptomatic benefit since the clinical importance of the difference in paracetamol consumption is debatable, and there was no significant difference in mean pain scores, episodes of distress, or absence from school. This interpretation is supported by secondary evidence of the pattern of benefit for each day after seeing the doctor (fig 3): the reduction in paracetamol use occurred only after the first 24 hours after seeing the doctor, when children were less distressed and the illness was starting to settle.
Figure 2.
Duration of symptoms of acute otitis media in children after seeing doctor
Table 2.
Effect of immediate or delayed antibiotic treatment on course of childhood acute otitis media. Values are means (ranges) unless stated otherwise
| Measure of illness | Antibiotic treatment allocated
|
Difference (95% CI) | Student's t test | |
|---|---|---|---|---|
| Immediate (n=135) | Delayed (n=150) | |||
| Duration of symptoms (days): | ||||
| Earache | 2.56 (0-10) | 3.57 (0-11) | −1.10 (−0.54 to −1.48) | t=4.24, P<0.01 |
| Ear discharge | 0.56 (0-7) | 1.21 (0-14) | −0.66 (−0.19 to −1.13) | t=2.75, P<0.01 |
| Night disturbance | 1.64 (0-8) | 2.35 (0-11) | −0.72 (−0.30 to −1.13) | t=3.41, P<0.01 |
| Crying | 1.54 (0-7) | 2.23 (0-11) | −0.69 (−0.31 to −1.08) | t=3.56, P<0.01 |
| No of school days missed | 1.97 (0-8) | 2.15 (0-13) | −0.18 (−0.76 to 0.41) | t=0.59, P=0.56 |
| Daily No of episodes of distress | 0.70 (0-4) | 0.82 (0-7) | −0.12 (−0.34 to 0.11) | t=1.02, P=0.31 |
| Daily No of spoons of paracetamol consumed | 1.69 (0-6) | 2.28 (0-8) | −0.52 (−0.79 to −0.26) | t=3.42, P<0.01 |
| Daily pain score | 2.29 (1-5) | 2.45 (1-6) | −0.16 (−0.42 to 0.11) | t=1.18, P=0.24 |
Figure 3.
Mean (SE) daily pain score, distress, and use of analgesia in children with acute otitis media after seeing doctor
Discussion
The results of our study, the largest randomised controlled trial to date of antibiotic use for acute otitis media in primary care, suggest that immediate prescription has some benefits but that these are probably balanced by the disadvantages. Our aim was not to assess efficacy of antibiotics but the effectiveness of prescribing strategies. This is the first trial to assess the implications of immediate prescription of antibiotics compared with delayed prescribing.
Limitations of trial
Selection and diagnostic bias
—The general practitioners agreeing to participate in this trial came from a representative spread of practice types. Despite the fact that low recruiting doctors were apparently more reluctant to recruit young children (hence a slightly older trial population than expected) and those with a perforated ear drum, the impact on the results is not likely to be significant. Patients of low recruiting doctors showed no difference from those of high recruiting doctors in mean duration of illness and response to treatment. With diagnosing otitis media, there is always concern that children with milder symptoms may simply have a pink ear drum due to non-specific viral illness, fever, or crying. However, doctors in our study were instructed to exclude any such cases if they were in doubt. Furthermore, since there was no significant interaction between treatment effect and the presence of florid clinical signs, the precise diagnostic criteria are unlikely to alter our conclusions. Similarly, the inclusion of more older children than expected is a potential concern, but this is not likely to alter the generalisability of our results since we found no significant difference in treatment effect according to age, nor according to whether participating doctors were low or high recruiters. Although we cannot exclude a modest difference in treatment effect in younger children (since the study was not powered to specifically look at subgroups), our inference that there is little difference in symptomatic benefit for younger children is supported by the most recent (and largest) trial of antibiotics in children aged under 2 years.21
Non-response bias—There was no evidence of significant differences in the characteristics of those patients who did not provide information compared with those who did. Thus, non-response is not likely to significantly bias the results.
Placebo effect—An open trial design was essential to assess the effect of treatment on participants' beliefs and behaviour, but it has the disadvantage of allowing a placebo effect. Although we minimised this by asking doctors to use a structured advice sheet—which was shown to abolish the antibiotic placebo effect in a previous trial6—some placebo effect might have contributed to the apparent benefits from antibiotics. However, the effect if any is probably small: our conclusions about the benefit of antibiotics are the same as those from meta-analyses of blinded, placebo controlled trials, and the size of difference in paracetamol consumption that we found is the same as in the largest blinded trial to date.5
Benefits from prescribing antibiotics immediately
Prescribing antibiotics immediately gave about one day's benefit in symptom duration, duration of ear discharge, number of days crying (when the child cried at some stage), and night disturbance and resulted in less paracetamol being used. We used the antibiotic dose recommended by UK prescribing guidelines, and the same as in a previous trial.5 However, children aged over 6 (20% of our study population) can be given a larger dose; thus we may have slightly underestimated the potential benefits, and side effects, of antibiotics in some older children. The overall benefit we found is consistent with results from both the previous systematic review4 and with the largest previous trials in both younger21 and older children.5 In particular, the estimate of differences in paracetamol use are very similar.5
However, the benefit came mainly after the first 24 hours, when distress and symptoms were settling anyway. Thus there was no significant reduction in pain or distress, and the difference in paracetamol consumption is arguably clinically insignificant—less than a spoon of paracetamol a day. An earlier trial suggested that immediate antibiotics would reduce absence from school during the acute illness.5 However this may have been a misleading finding: when parents know that the illness is settling without antibiotics (as in the current study) they are not sufficiently concerned about the severity of illness to make any difference in school attendance. Perhaps one of the most important findings for parents from the current study, and consistent with the previous trial,5 is the reduced night disturbance with antibiotics. This suggests that if delayed prescribing is to be used instead of prescribing antibiotics immediately, particular attention should be paid to advising parents about giving full doses of analgesia before bed time.
What is already known on this topic
There is debate whether acute ear infections (otitis media) should be treated with antibiotics
A delayed prescribing strategy used in other countries has not been subject to a randomised trial
What this study adds
Immediate antibiotics provided benefits compared with delayed prescribing, but mainly after the first 24 hours, when symptoms were already improving
Immediate antibiotics increased diarrhoea by 10%
A wait and see approach is feasible, acceptable to parents, and should substantially reduce use of antibiotics
There may be a case for treating younger children more aggressively, in view of the possible greater risk of mastoiditis. A case series found that 60% of cases of mastoiditis were in children aged under 2 years and that boys were almost twice as likely to be affected as girls.22 However, three reports claim that the increased incidence of acute mastoiditis in modern populations is related to penicillin resistant organisms.23–25 Thus, the solution to the problem of increasing acute mastoiditis may be more selective use of antibiotics for acute infections, including acute otitis media, which is the commonest reason for children to be prescribed antibiotics in primary care.26
Disadvantages of antibiotics
Prescribing antibiotics immediately increased the number of children who had diarrhoea, which supports the findings from the systematic review.4 Immediate prescribing also increased parents' belief in the effectiveness of antibiotics and their intention to consult their doctor with the same problem in future, as we found in a previous trial for sore throat.6 By prescribing early for a self limiting illness, doctors fuel expectation and probably encourage the cycle of reattendance.7 This will maintain parental demand for antibiotics, which encourages the prescribing of antibiotics8,9 and the further development of antibiotic resistance.10
Satisfaction of parents
Doctors overestimate the pressure by patients to prescribe antibiotics.27 Doctors also prescribe to satisfy their patients even when they don't think the prescription is necessary because they believe that patients will not be satisfied unless an antibiotic is prescribed.28 This study clearly shows that this perception is false: although satisfaction was slightly increased when antibiotics were prescribed, most of the parents in the delayed treatment group were very satisfied with the “wait and see” approach.
Conclusion
Immediate prescription of antibiotics for acute otitis media reduced the duration of illness, but the benefit occurred mainly after the first 24 hours, when symptoms were already resolving. This must be balanced against both side effects and increasing parents' belief in the importance of antibiotics. A wait and see approach in the management of acute otitis media is feasible and was acceptable to most parents and resulted in a 76% reduction in the use of antibiotic prescriptions.
Table 3.
Effect of immediate or delayed antibiotic treatment for childhood acute otitis media on percentage not better (3 days after seeing the doctor), parents' belief in antibiotics and satisfaction with treatment, and side effects of antibiotic use. Values are numbers (percentages) unless stated otherwise
| Antibiotic treatment allocated
|
Difference | ||
|---|---|---|---|
| Immediate (n=135) | Delayed (n=150) | ||
| Patients not better | 19 (14) | 45 (30) | χ2=10.3, P<0.01 |
| Belief that antibiotics are very effective | 100/131 (76) | 64/140 (46) | χ2=19.3, P<0.01 |
| Very satisfied with treatment approach | 123 (91) | 115 (77) | χ2=10.8, P<0.01 |
| Very likely to consult doctor in future | 109/132 (83) | 92/147 (63) | χ2=13.8, P<0.01 |
| Side effects: | |||
| Rash | 6/133 (5) | 8/149 (5) | χ2=0.1, P=0.74 |
| Diarrhoea | 25 (19) | 14 (9) | χ2=5.2, P=0.02 |
Acknowledgments
We are grateful to the following doctors for their enthusiasm and help in recruiting patients: Doctors Newman, Taylor, Traynor, Tippett, Warner, Peace, Stephens, Glasspool, Stone, Webb, Snell, Devereux, Hoghton, Terry, Dickson, Nightingale, Richenbach, Bacon, Lupton, Padday, Cookson, Stanger, Glaysher, Bond, Baker, Barnsley, Jeffries, Willard, Carlisle, Hill, Collier, Cubitt, De Quincey, Over, White, Billington, Percival, Hollands, Glaysher, and Stranger.
Footnotes
Funding: NHS Research and Development (South West and South East Regions). PL is supported by the Medical Research Council.
Competing interests: None declared.
References
- 1.Bain J. Controversies in therapeutics: Childhood otalgia: justification for antibiotic use in general practice. BMJ. 1990;300:1006–1007. doi: 10.1136/bmj.300.6730.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Browning G. Controversies in therapeutics: childhood otalgia: acute otitis media. Antibiotics not necessary in most cases. BMJ. 1990;300:1005–1006. doi: 10.1136/bmj.300.6730.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Froom J, Culpepper L, Jacobs M. Antimicrobials for acute otitis media? A review from the international primary care network. BMJ. 1997;315:98–102. doi: 10.1136/bmj.315.7100.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Del Mar C, Glaziou P, Hayem M. Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis. BMJ. 1997;314:1526–1529. doi: 10.1136/bmj.314.7093.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke P, Bain J, Robinson D, Dunleavey J. Acute red ear in children: controlled trial of non-antibiotic treatment in general practice. BMJ. 1991;303:558–562. doi: 10.1136/bmj.303.6802.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Little PS, Williamson I, Warner G, Gould C, Gantley M, Kinmonth AL. An open randomised trial of prescribing strategies for sore throat. BMJ. 1997;314:722–727. doi: 10.1136/bmj.314.7082.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Little PS, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ. 1997;315:350–352. doi: 10.1136/bmj.315.7104.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Britten N, Ukoumunne O. The influence of patients' hopes of receiving a prescription on doctors' perceptions and the decision to prescribe: a questionnaire survey. BMJ. 1997;315:1506–1510. doi: 10.1136/bmj.315.7121.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MacFarlane J, Holmes W, MacFarlane R, Britten N. Influence of patients' expectations on antibiotics management of acute lower respiratory illness in general practice: questionnaire study. BMJ. 1997;315:1211–1214. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arason V, Kristinsson K, Sigurdsson J, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the rate of penicillin resistant pneumococci in children? Cross sectional prevalence study. BMJ. 1996;313:387–391. doi: 10.1136/bmj.313.7054.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Buchem FL, Peeters MF, Van 'T Hof MA. Acute otitis media a new treatment strategy. BMJ. 1985;290:1033–1037. doi: 10.1136/bmj.290.6474.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pitts J. Shared decision making in the informed treatment of acute otitis media. Practitioner. 1987;231:1232–1233. [PubMed] [Google Scholar]
- 13.Gates G, Northern J, Ferrer P. Diagnosis and screening. Ann Otolo Laryngol. 1989;98(suppl 139):39–41. [PubMed] [Google Scholar]
- 14.Schwartz R, Rodriguez W, Brook I, Grundfast K. The febrile response in otitis media. JAMA. 1981;245:2057–2058. [PubMed] [Google Scholar]
- 15.Preston K. Pneumatic otoscopy: a review of the literature. Issues Compr Pediatr Nurs. 1998;21:117–128. doi: 10.1080/014608698265537. [DOI] [PubMed] [Google Scholar]
- 16.Ruuskanen O, Heikkinen T. Otitis media: etiology and diagnosis. Pediatr Infect Dis J. 1994;13:s23–6. [PubMed] [Google Scholar]
- 17.Rogers M. A viable alternative to the glass/mercury thermometer. Paediatr Nurs 1992;4.
- 18.Brown T, Fisk G. Anaesthesia for children. Oxford: Blackwell Scientific; 1992. p. 129. [Google Scholar]
- 19.Wilkin D, Hallam L, Doggett AM. Measures of need and outcome for primary health care. Oxford: Oxford University Press; 1992. [Google Scholar]
- 20.Office of Population Censuses and Surveys. Morbidity statistics from general practice: fourth national study 1991. London: HMSO; 1994. [Google Scholar]
- 21.Damoiseaux R, Van Balen F, Hoes A, Verheij T, De Melker R. Primary care based randomised double blind trial of amoxicillin versus placebo for acute otitis media in children aged under 2 years. BMJ. 2000;320:350–354. doi: 10.1136/bmj.320.7231.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoppe J, Koster S, Bootz F, Niethammer D. Acute mastoiditis—relevant once again. Infection. 1994;22:178–182. doi: 10.1007/BF01716698. [DOI] [PubMed] [Google Scholar]
- 23.Kudo F, Sasamura Y. Acute mastoiditis in infants: penicillin-resistant Streptococcus pneumoniae and its therapy. Nippon Jibiinkoka Gakkai Kaiho. 1998;101:1075–1081. doi: 10.3950/jibiinkoka.101.9_1075. [DOI] [PubMed] [Google Scholar]
- 24.Collison P, Farver D. Acute coalescent mastoiditis caused by antibiotic resistant organisms. S D J Med. 1998;51:379–383. [PubMed] [Google Scholar]
- 25.Antonelli P, Dhanani N, Giannoni C, Kubilis P. Impact of resistant pneumococcus on the rates of acute mastoiditis. Otolaryngol Head Neck Surg. 1999;121:190–194. doi: 10.1016/S0194-5998(99)70170-1. [DOI] [PubMed] [Google Scholar]
- 26.Cates C. An evidence based approach to reducing antibiotic use in children with acute otitis media: controlled before and after study. BMJ. 1999;318:715–716. doi: 10.1136/bmj.318.7185.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cartwright A, Anderson R. General practice revisited: a second study of general practice. London: Tavistock; 1981. [Google Scholar]
- 28.Butler C, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners' and patients' perceptions of antibiotics for sore throat. BMJ. 1998;317:632–637. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]