Abstract
A 43-year-old man with a history of metastatic carcinoid disease is presented. The patient had symptoms of chronic intermittent abdominal pain two years after undergoing a wireless capsule endoscopy procedure. Radiological examinations revealed a retained capsule endoscope, and the patient underwent exploratory laparotomy with capsule retrieval. To the authors’ knowledge, this is the first case presentation of chronic, partial small bowel obstruction caused by unrecognized retention of a capsule endoscope.
Keywords: Abdominal pain, Capsule endoscopy, Carcinoid tumour, Small-bowel
Abstract
Les auteurs présentent le cas d’un homme de 43 ans atteint d’un cancer métastatique. Le patient éprouvait des symptômes de douleur abdominale intermittente chronique deux ans après avoir subi une endoscopie au moyen d’une capsule vidéo-endoscopique sans fil. Les examens radiologiques ont révélé la présence de la capsule et une laparotomie exploratoire à permis de l’extraire. À la connaissance des auteurs, il s’agit du premier cas d’obstruction partielle chronique du grêle causée par la rétention d’une capsule endoscopique.
Wireless capsule endoscopy is a new and sensitive diagnostic modality for examining the small bowel. It has been used for a variety of clinical indications, primarily the diagnosis of inflammatory bowel disease and localization of occult gastrointestinal (GI) bleeding (1–6). It is also an important tool for detecting small bowel tumours, including carcinoid tumours of the GI tract (7–10).
Although it is usually a safe procedure, capsule retention due to an unsuspected, obstructive small bowel lesion is a known complication (1,6,11,12). We report a case of a 43-year-old man with a history of metastatic carcinoid disease who had undergone capsule endoscopy two years earlier to rule out a primary small bowel tumour. Over the ensuing years, he complained of intermittent postprandial abdominal pain and weight loss. Although interval radiological examinations were obtained, a diagnosis of capsule retention was not made. To our knowledge, this is the only reported case of prolonged, unrecognized capsule retention causing chronic, partial small bowel obstruction.
CASE PRESENTATION
A 43-year-old man with a history of metastatic carcinoid disease was referred to the H Lee Moffitt Cancer Center and Research Institute (USA) for evaluation of intractable abdominal pain.
He had an eight-year history of intermittent diarrhea and abdominal pain, and a five-year history of facial flushing. In April 2003, a contrast-enhanced abdominal computed tomography (CT) scan revealed innumerable heterogeneous enhancing masses in the liver. There was also thickening and dilation in a distal segment of the small bowel. A CT-guided needle biopsy of a liver lesion demonstrated a metastatic carcinoid tumour. Subsequently, an upper GI series with small bowel follow-through showed no evidence of an abnormal mass or filling defect. Therefore, capsule endoscopy was performed. The capsule was noted to enter the small intestine after approximately 1 h and approximately 5 h 14 min later, a large amount of debris was noted within the lumen of the intestine, suggesting possible passage into the colon. The study terminated at 7 h 19 min and failed to demonstrate any evidence of tumour inflammation or narrowing within the intestines. In retrospect, the patient did not remember ever passing the capsule.
Treatment for the metastatic carcinoid tumour was initiated with the drug octreotide acetate (Sandostatin LAR, Novartis Pharmaceuticals Canada Inc), and later with gefitinib. During the ensuing two years, the patient complained of increasing frequency and intensity of his abdominal pain. He described the pain as spasmodic, and rated it as six of 10 on average, three of 10 at best and 10 of 10 at worst, particularly after meals. Because eating often aggravated the pain, he limited his food intake, resulting in a weight loss of approximately 18 kg over two years. Frequently, the pain was only relieved by emesis. CT scans were performed at regular intervals to evaluate the progression of metastatic carcinoid disease. Several radiologists noted a small, metallic object in the lower right quadrant of the abdomen, but this finding was dismissed on one CT scan report as a possible bullet fragment. The patient’s GI symptoms were attributed to his metastatic carcinoid tumour.
At the time of presentation to the H Lee Moffitt Cancer Center and Research Institute, physical examination revealed a healthy-appearing man who was conscious to people, places and time. His pulse rate was a regular 62 beats/min, his respiratory rate was 12 breaths/min and his right arm blood pressure was 104/68 mmHg. Chest auscultation was clear with no adventitial sounds. The abdomen was soft and nontender, with palpable hepatomegaly to the level of the umbilicus. Bowel sounds were loud and high pitched. Palpation of the liver precipitated intense facial flushing.
Due to the history of persistent, spasmodic abdominal pain, plain films of the abdomen were obtained to exclude bowel obstruction. The films revealed a radiopaque foreign body in the pelvic area (Figure 1). It was thought to be a set of batteries retained during the capsule endoscopy procedure performed two years earlier. Small bowel enteroclysis was performed for further anatomical evaluation. It revealed focal bowel dilation proximal to the radiopaque foreign body.
Figure 1).
Plain abdominal x-ray demonstrating a radiopaque foreign body in the pelvic area
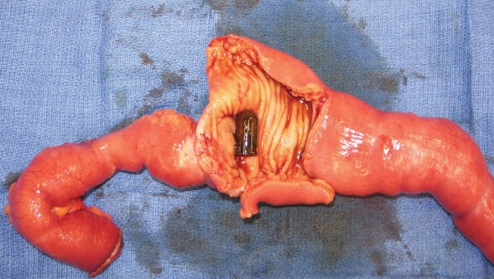
Next, the patient underwent exploratory laparotomy for small bowel resection and removal of the foreign body, with the aim of relieving his symptoms of intermittent, partial small bowel obstruction. A cylindrical, plastic capsule measuring 2 cm in length and 1.1 cm in diameter was located within the proximal ileum (Figure 2). Peristalsis caused it to impact intermittently against a near-obstructive lesion in a ‘ball-valve’ fashion. Inside the capsule were two batteries measuring 0.5 cm in length and 0.9 cm in diameter.
Figure 2).
Surgical specimen of terminal ilium containing a wireless capsule endoscope adjacent to the obstructive tumour
Approximately 50 cm of proximal ileum was resected. The ileal specimen contained numerous exophytic lesions, the largest measuring 1.5 cm and invading through the bowel wall into the serosa. Pathology was consistent with a well-differentiated carcinoid tumour. Nine months after surgery, the patient no longer complained of abdominal pain, weight loss or postprandial emesis.
DISCUSSION
The Pillcam SB capsule endoscope (Given Imaging Ltd, Israel) is an important diagnostic modality for evaluating small bowel mucosa. It is a plastic, nonbiodegradable capsule, measuring 11 mm × 26 mm, and housing a digital video camera, a light source, a transmitter, an antenna and batteries. Two images per second are taken and transmitted to a data recorder worn around the patient’s waist (11).
Although capsule endoscopy is usually safe, retention of the capsule due to an unsuspected, obstructive lesion is a known complication (6,11,13). A capsule retention rate of 1% to 5% has been reported in several clinical series (1,2,4,6). Pennazio et al (4) reported capsule retention in five of 100 patients, all who had negative barium small bowel follow-through. Four patients required surgical removal, and one had the capsule retrieved endoscopically. Cheifetz et al (12) reported retention of video capsule endoscopes in six of 102 patients who underwent the procedure for evaluation of Crohn’s disease. Capsule impaction can be caused by tumours, strictures or other structures such as Zenker’s diverticula (14). One case presentation described a capsule fragmentation in the small bowel (15). The two-year duration of capsule retention reported in this case is the longest recorded in literature. It is notable that the nonbiodegradable plastic capsule shell survived the corrosive digestive environment for such a prolonged period.
To rule out an occult obstructing lesion, many patients undergo a small bowel contrast study before capsule endoscopy. Evidence of lumenal narrowing is generally considered a contraindication to capsule endoscopy (11). However, small bowel contrast studies are not entirely sensitive for excluding potential stenosis (13). Enteroclysis yields greater anatomical detail than small bowel follow-through studies and may therefore be a preferable screening exam for excluding an occult obstructive lesion.
Retained capsules do not always result in obstructive symptoms and may not necessitate surgical retrieval. Kornbluth et al (16) reported on a patient who retained a capsule for 21 months without having any symptoms (16).
A recent innovation designed to reduce the risk of capsule retention is the new Patency Capsule (Given Imaging Ltd, Israel) (13,15). This capsule is the same size as the standard Pillcam capsule, but is designed to dissolve in the GI tract after two to three days if it is retained. The capsule contains barium and can therefore be detected radiographically (13). Increased use of this screening capsule may help to prevent capsule retention and enhance the safety of wireless capsule endoscopy.
Clinicians who order and/or perform capsule endoscopy should be aware of the potential for capsule retention and perform appropriate follow-up. Plain abdominal films should be considered in patients who cannot recall excreting the capsule after two weeks or who manifest symptoms of bowel obstruction (15). Because of the increasing frequency of video capsule endoscopy, radiologists interpreting plain abdominal films or CT scans need to be cognizant of the radiographical appearance of retained capsule endoscopes and alert clinicians when retention is suspected.
REFERENCES
- 1.Enns R, Go K, Chang H, Pluta K. Capsule endoscopy: A single-centre experience with the first 226 capsules. Can J Gastroenterol. 2004;18:555–8. doi: 10.1155/2004/319195. [DOI] [PubMed] [Google Scholar]
- 2.Fireman Z, Eliakim R, Adler S, Scapa E. Capsule endoscopy in real life: A four-centre experience of 160 consecutive patients in Israel. Eur J Gastroenterol Hepatol. 2004;16:927–31. doi: 10.1097/00042737-200409000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Hara AK, Leighton JA, Sharma VK, Fleischer DE. Small bowel: Preliminary comparison of capsule endoscopy with barium study and CT. Radiology. 2004;230:260–5. doi: 10.1148/radiol.2301021535. [DOI] [PubMed] [Google Scholar]
- 4.Pennazio M, Santucci R, Rondonotti E, et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: Report of 100 consecutive cases. Gastroenterology. 2004;126:643–53. doi: 10.1053/j.gastro.2003.11.057. [DOI] [PubMed] [Google Scholar]
- 5.Mata A, Llach J, Bordas JM, et al. [Role of capsule endoscopy in patients with obscure digestive bleeding] Gastroenterol Hepatol. 2003;26:619–23. doi: 10.1016/s0210-5705(03)70420-8. [DOI] [PubMed] [Google Scholar]
- 6.Eliakim R. Wireless capsule video endoscopy: Three years of experience. World J Gastroenterol. 2004;10:1238–9. doi: 10.3748/wjg.v10.i9.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coates SW, Jr, DeMarco DC. Metastatic carcinoid tumor discovered by capsule endoscopy and not detected by esophagogastroduo-denoscopy. Dig Dis Sci. 2004;49:639–41. doi: 10.1023/b:ddas.0000026311.62364.0b. [DOI] [PubMed] [Google Scholar]
- 8.de Mascarenhas-Saraiva MN, da Silva Araujo Lopes LM. Small-bowel tumors diagnosed by wireless capsule endoscopy: Report of five cases. Endoscopy. 2003;35:865–8. doi: 10.1055/s-2003-42625. [DOI] [PubMed] [Google Scholar]
- 9.Forner A, Mata A, Puig M, et al. Ileal carcinoid tumor as a cause of massive lower-GI bleeding: The role of capsule endoscopy. Gastrointest Endosc. 2004;60:483–5. doi: 10.1016/s0016-5107(04)01814-0. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Compean D, Gonzalez JA, Giasi Gonzalez E, Cuervo Perez LE, Saldana G, Maldonado Garza H. [Ileal carcinoid tumor manifesting as gastrointestinal hemorrhage and diagnosed with capsule endoscopy: Case report] Rev Gastroenterol Mex. 2005;70:164–8. [PubMed] [Google Scholar]
- 11.Chang PK, Holt EG, De Villiers WJ, Boulanger BR. A new complication from a new technology: What a general surgeon should know about wireless capsule endoscopy. Am Surg. 2005;71:455–8. [PubMed] [Google Scholar]
- 12.Cheifetz AS, Kornbluth AA, Legnani PE, et al. Incidence and outcome of the retained video capsule endoscope (CE) in Crohn’s disease (CD): Is it a “therapeutic complication”? Am J Gastroenterol 200499S262(Abst) [Google Scholar]
- 13.Melmed GY, Lo SK. Capsule endoscopy: Practical applications. Clin Gastroenterol Hepatol. 2005;3:411–22. doi: 10.1016/s1542-3565(05)00019-4. [DOI] [PubMed] [Google Scholar]
- 14.Geller AJ. Videocapsule impaction in a Zenker’s diverticulum. J Clin Gastroenterol. 2005;39:647–8. doi: 10.1097/01.mcg.0000171154.46907.f0. [DOI] [PubMed] [Google Scholar]
- 15.Fry LC, De Petris G, Swain JM, Fleischer DE. Impaction and fracture of a video capsule in the small bowel requiring laparotomy for removal of the capsule fragments. Endoscopy. 2005;37:674–6. doi: 10.1055/s-2005-870252. [DOI] [PubMed] [Google Scholar]
- 16.Kornbluth A, Legnani P, Lewis BS. Video capsule endoscopy in inflammatory bowel disease: Past, present, and future. Inflamm Bowel Dis. 2004;10:278–85. doi: 10.1097/00054725-200405000-00017. [DOI] [PubMed] [Google Scholar]