Abstract
Collagenous colitis is an inflammatory mucosal disorder of the colon with distinctive histopathological features, including a thickened subepithelial collagen layer. The clinical course is usually benign, but serious complications, including death, may occur. In the present report, a 69-year-old woman with watery diarrhea and collagenous colitis developed bloody diarrhea that was refractory to treatment medications, including corticosteroids and azathioprine. Endoscopic and histopathological studies showed a focal neutrophilic inflammatory process that progressed to a diffuse and extensive form of colitis, eventually requiring total proctocolectomy. Careful histological review of the resected colon showed no evidence of persistent collagenous colitis. These findings suggest an important need for continued long-term follow-up of patients with collagenous colitis because superimposed and serious colonic complications may occur, including a severe and extensive pancolitis refractory to medications and necessitating total proctocolectomy.
Keywords: Collagenous colitis; Etiology, pathogenesis; medical and surgical treatment of inflammatory bowel disease; Ulcerative colitis
Abstract
La colite collagénique est un trouble inflammatoire de la muqueuse du côlon aux caractéristiques histopathologiques particulières, y compris un épaississement de la couche de collagène sous-épithélial. D’ordinaire, l’évolution clinique est bénigne, mais de graves complications, y compris la mort, peuvent survenir. Dans le présent rapport, une femme de 69 ans atteinte de diarrhée aqueuse et de colite collagénique a développé une diarrhée sanglante réfractaire aux médicaments, y compris les corticoïdes et l’azathriopine. Les études endoscopiques et histopathologiques ont révélé un processus inflammatoire neutrophile focal qui a évolué vers une forme de colite diffuse et étendue, laquelle a fini par exiger une proctocolectomie totale. Une analyse histologique attentive du côlon réséqué n’a révélé aucune trace de colite collagénique persistante. Ces observations soulignent l’importance d’assurer un suivi prolongé continu des patients atteints de colite collagénique en raison du risque concomitant de complications coliques graves, y compris une pancolite grave et étendue réfractaire aux médicaments et exigeant une proctocolectomie totale.
Collagenous colitis is an inflammatory mucosal disorder of the colon with distinctive histopathological features, including a thickened subepithelial collagen layer (1). Collagenous colitis is most often seen in middle-aged and elderly women, usually with watery and nonbloody diarrhea. In some individuals, the disease may also involve the stomach and the small intestine (2,3). Finally, there is an intimate relationship between collagenous colitis and celiac disease (4,5).
Most often, the clinical course appears to be benign (6,7). However, serious colonic complications, including death, have been reported (8), although they are rare. Other complications include spontaneous peritonitis with free perforation of the colonic wall (9), submucosal dissection (10) and colonic ‘fracturing’, apparently during endoscopic instrumentation (11). Colon carcinoma may also complicate the clinical course of collagenous colitis (12,13), while lymphoma and carcinoid tumours have also been noted in some case studies (14–16). Recently, a paraneoplastic form of collagenous inflammatory disease involving the small intestine and the colon completely resolved following resection of an invasive colon carcinoma (17). The present report documents yet another serious colonic complication of collagenous colitis, namely, the development of severe and extensive ulcerative colitis.
CASE PRESENTATION
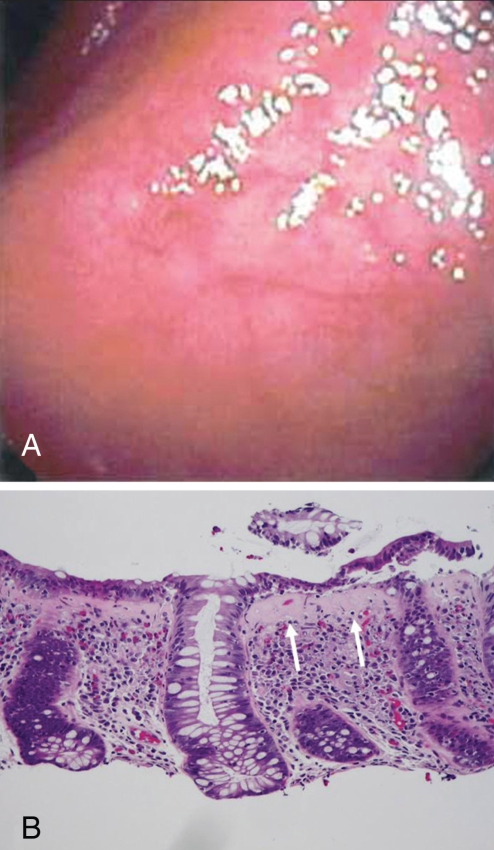
A 69-year-old woman was first evaluated in June 2003 because of five weeks of watery diarrhea, occuring three to four times daily. Fecal cultures and parasite studies were negative. Results of the hemogram were normal, showing hemoglobin levels of 134 g/L, white blood cell counts of 9600/mm3 and platelet counts of 252,000/mm3. The sedimentation rate (3 mm/h), flexible sigmoidoscopy and rectal biopsy were normal. Because the diarrhea became more severe (up to 10 times daily), endoscopic studies were performed. Examination of the upper gastrointestinal tract was normal, and the gastric and duodenal mucosal biopsies were normal. Colonoscopic evaluation showed slightly erythematous, but nonfriable, mucosa (Figure 1A), while biopsies showed collagenous colitis (Figure 1B).
Figure 1).
A Initial colonoscopy performed in June 2003 showing virtually normal colonic mucosa with a faint vascular pattern. B Colonic biopsy showing collagenous colitis with markedly thickened subepithelial collagen layer (arrows), increased number of intraepithelial lymphocytes and characteristic separation of epithelial layer from underlying stroma (right side of photograph). Hematoxylin and eosin stain, original magnification × 200
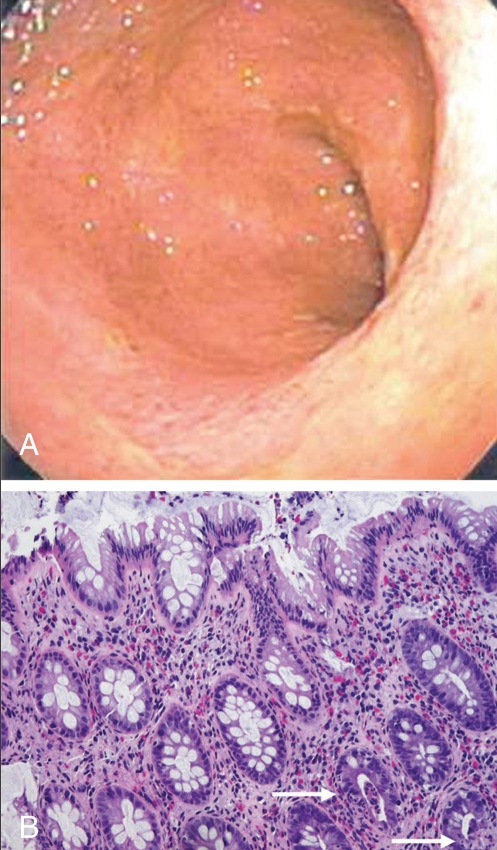
The diarrhea resolved over the next month but recurred in April 2004. This led to treatment with 5-aminosalicylate (5-ASA) (Asacol, Procter & Gamble Pharmaceuticals Canada Inc) 800 mg twice a day followed by the addition of budesonide controlled ileal release (Entocort 2, AstraZeneca Canada Inc) 3 mg twice a day. Because her diarrhea subsided, the budesonide was discontinued by August 2004. In December 2004, the diarrhea recurred. Additional fecal cultures were negative. Colonoscopy showed mucosal hyperemia throughout the entire colon (Figure 2A). The mucosa was not friable, and no ulceration or exudate was present. Biopsies showed focal neutrophilic infiltration within several crypts, along with increased chonic inflammatory cells in the lamina propria (Figure 2B). However, the subepithelial collagen layer was no longer increased in thickness and there was no intra-epithelial lymphocytosis. Another course of 5-ASA was administered along with budesonide controlled ileal release, and the diarrhea resolved again.
Figure 2).
A Colonoscopy performed in April 2004 showing diffusely inflamed colonic mucosa with loss of vascular pattern. B Colonic biopsy showing focal infiltrate of neutrophils within a few crypts (arrows). There is no evidence of subepithelial collagen layer thickening or intraepithelial lymphocytosis. The crypt architecture is well-maintained. Hematoxylin and eosin stain, original magnification × 200
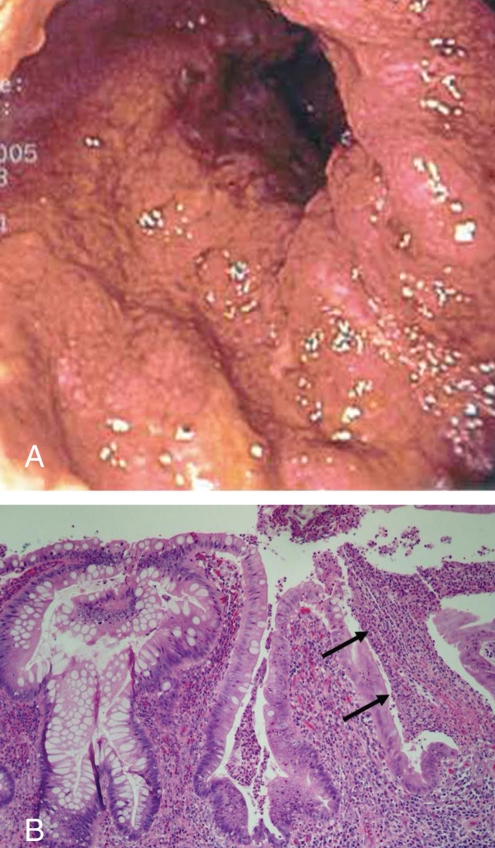
In March 2005, bloody diarrhea was noted for the first time. Lower abdominal pain, increased stool frequency up to 10 times daily and weight loss of 10 kg were noted. Fecal cultures, parasite studies and toxin assays were negative. Colonoscopy now showed extensive and diffuse inflammatory disease with mucosal friability and exudate, typical of extensive mucosal involvement with ulcerative colitis (Figure 3A). Biopsies showed changes of severe ulcerative colitis but no evidence of persistent collagenous colitis (Figure 3B).
Figure 3).
A Colonoscopy performed in November 2005 showing diffusely inflamed, swollen and friable colonic mucosa. B Colonic biopsy showing features of ulcerative colitis with mixed inflammatory cell infiltrate within the lamina propria, marked distortion of crypt architecture and crypt abscess formation (arrows). No thickened subepithelial collagen layer was present and there was no intraepithelial lymphocytosis. Hematoxylin and eosin stain, original magnification ×200
Over the next eight months, her symptoms became more severe despite treatment with 5-ASA, and the addition of oral prednisone (40 mg daily) and azathioprine (100 mg daily). By November 2005, bloody diarrhea became intractable with frequent episodes of incontinence. She became anemic with hemoglobin levels dropping to 90 g/L, and developed hypoalbuminemia, with serum albumin levels dropping to 29 g/L. She had a laparoscopic hand-assisted proctocolectomy with abdominoperineal resection and creation of an end-ileostomy. A review of histology from the resected colon showed extensive ulcerative colitis involving the entire colon without dysplasia. There was no histological evidence of collagenous colitis.
DISCUSSION
The present report documents the clinical, endoscopic and histopathological evolution of collagenous colitis followed by severe ulcerative pancolitis refractory to different drug treatments, including corticosteroids, and an immunosuppressive medication, eventually resulting in a proctocolectomy. Earlier literature-reported cases, summarized in Table 1, have suggested the progression of collagenous colitis into extensive ulcerative colitis (18–21). However, in contrast to our patient, these earlier reports all described only symptomatic improvements to medications, including 5-ASA and steroids, and in some, the use of azathioprine. Unfortunately, the durations of follow-up in most of these earlier cases were brief, often only limited to reduced symptoms during, or for a short period after, hospitalization. In only one reported case (17) with post-treatment biopsies, no active inflammatory disease or evidence for collagenous colitis could be documented. In all of the other cases (18–21), further follow-up endoscopic and histopathological studies were not performed. In the present report, careful pathological evaluation of the entire resected colon revealed an extensive and diffuse mucosal inflammatory process typical of ulcerative pancolitis with no residual thickening of the subepithelial collagen layer, characteristic of collagenous colitis.
TABLE 1.
Reported cases of collagenous colitis evolving into ulcerative colitis in women
| Age, years (Reference) | NSAIDS | Collagenous colitis duration* | Pancolitis† | Treatment | Outcome |
|---|---|---|---|---|---|
| 67 (18) | Yes | 12 weeks | Yes | 5-ASA, Ster, Aza | Diarrhea resolved‡ |
| 66 (19) | No | 13 months | Yes | 5-ASA, Ster | Remission§ |
| 64 (19) | Yes | 12 months | Yes | 5-ASA, Ster | Remission§ |
| 54 (20) | No | 12 months | Yes | 5-ASA, Ster | Remission§ |
| 51 (21) | No | >10 years | Yes | 5-ASA, Ster, Aza | Improved¶ |
| 69 (present case) | No | 20 months | Yes | 5-ASA, Ster, Aza | Colectomy |
Collagenous colitis duration (biopsy-defined) before diagnosis of ulcerative colitis;
Extent of ulcerative colitis defined by colonoscopy and biopsies;
Repeat biopsies showed no active inflammation or evidence of collagenous colitis;
Symptomatic remission, no repeat colonoscopic biopsies;
After small-bowel biopsies showed changes consistent with untreated celiac disease, further improvement occurred with a gluten-free diet. No repeat small intestinal or colonoscopic biopsies. 5-ASA 5-aminosalicylate; Aza Azathioprine; NSAIDs Nonsteroidal anti-inflammatory drugs; Ster Steroids
While associations between collagenous colitis and other inflammatory bowel disorders (eg, Crohn’s disease) have been reported in the same patient (22,23) or family (24), this could occur due to chance alone. Moreover, differences in genetic and other factors suggest that collagenous colitis has a separate etiology and/or pathogenesis, distinct from chronic idiopathic inflammatory bowel disease (25–28). However, the abrupt and complete transition of this distinctive pathological process, collagenous colitis into extensive ulcerative colitis, as occurred in the present patient, provides especially strong evidence that the two may be more directly linked. Although concomitant treatment with nonsteroidal anti-inflammatory drugs in patients with collagenous colitis may have been a factor in the exacerbation of occult ulcerative colitis in some earlier cases (18,19), this was not seen in others (19–21), including the present case. Studies are still needed to elucidate possible similarities and differences in the pathogenetic features of collagenous colitis and ulcerative colitis.
Although collagenous colitis is generally regarded as a disorder having a relatively ‘benign’ clinical course, a number of serious colonic complications have been recorded. These include spontaneous development of peritonitis associated with free perforation of the colon (9), submucosal dissection (10) and colonic ‘fracturing’, particularly during endoscopic instrumentation (11). Malignant colonic disease may also occur during the clinical course of collagenous colitis, although the risk of colon cancer may not be increased (12,13). The present report further emphasizes that collagenous colitis may herald another colonic complication with potentially serious clinical consequences. Together, the reports reviewed showed that most cases of extensive ulcerative colitis progressing from collagenous colitis occur within one to two years of initial diagnosis of collagenous colitis. However, progression to extensive colitis even decades later (21) further suggests that the risk of this complication persists despite the passage of time. These findings underscore the need for continued clinical follow-up and investigation of any change in symptoms in patients with collagenous colitis.
REFERENCES
- 1.Freeman HJ. Collagenous mucosal inflammatory diseases of the gastrointestinal tract. Gastroenterology. 2005;129:338–50. doi: 10.1053/j.gastro.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 2.Pulimood AB, Ramakrishna BS, Mathan MM. Collagenous gastritis and collagenous colitis: A report with sequential histological and ultrastructural findings. Gut. 1999;44:881–5. doi: 10.1136/gut.44.6.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castellano VM, Munoz MT, Colina F, Nevado M, Casis B, Solis-Herruzo JA. Collagenous gastrobulbitis and collagenous colitis. Case report and review of the literature. Scand J Gastroenterol. 1999;34:632–8. doi: 10.1080/003655299750026128. [DOI] [PubMed] [Google Scholar]
- 4.Hamilton I, Sanders S, Hopwood D, Bouchier IA. Collagenous colitis associated with small intestinal villous atrophy. Gut. 1986;27:1394–8. doi: 10.1136/gut.27.11.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freeman HJ. Collagenous colitis as the presenting feature of biopsy-defined celiac disease. J Clin Gastroenterol. 2004;38:664–8. doi: 10.1097/01.mcg.0000135363.12794.2b. [DOI] [PubMed] [Google Scholar]
- 6.Bonderup OK, Folkersen BH, Gjersoe P, Teglbjaerg PS. Collagenous colitis: A long-term follow-up study. Eur J Gastroenterol Hepatol. 1999;11:493–5. [PubMed] [Google Scholar]
- 7.Goff JS, Barnett JL, Pelke T, Appelman HD. Collagenous colitis: Histopathology and clinical course. Am J Gastroenterol. 1997;92:57–60. [PubMed] [Google Scholar]
- 8.Widgren S, MacGee W. Collagenous colitis with protracted course and fatal evolution. Report of a case. Pathol Res Pract. 1990;186:303–6. doi: 10.1016/S0344-0338(11)80551-0. [DOI] [PubMed] [Google Scholar]
- 9.Freeman HJ, James D, Mahoney CJ. Spontaneous peritonitis from perforation of the colon in collagenous colitis. Can J Gastroenterol. 2001;15:265–7. doi: 10.1155/2001/194837. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell JD, Teague R, Bolton R, Lowes J. Submucosal “dissection” in collagenous colitis. Gut. 2004;53:470. [PMC free article] [PubMed] [Google Scholar]
- 11.Sherman A, Ackert JJ, Rajapaksa R, West AB, Oweity T. Fractured colon: An endoscopically distinctive lesion associated with colonic perforation following colonoscopy in patients with collagenous colitis. J Clin Gastroenterol. 2004;38:341–5. doi: 10.1097/00004836-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Gardiner GW, Goldberg R, Currie D, Murray D. Colonic carcinoma associated with an abnormal collagen table. Collagenous colitis. Cancer. 1984;54:2973–7. doi: 10.1002/1097-0142(19841215)54:12<2973::aid-cncr2820541227>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 13.Chan JL, Tersmette AC, Offerhaus GJ, Gruber SB, Bayless TM, Giardiello FM. Cancer risk in collagenous colitis. Inflamm Bowel Dis. 1999;5:40–3. doi: 10.1097/00054725-199902000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Edwards DB.Collagenous colitis and histiocytic lymphoma Ann Intern Med 1989111260–1.(Lett) [DOI] [PubMed] [Google Scholar]
- 15.Freeman HJ.Lymphoproliferative disorders in collagenous colitis Inflamm Bowel Dis 200511781–2.(Lett) [DOI] [PubMed] [Google Scholar]
- 16.Nussinson E, Samara M, Vigder L, Shafer I, Tzur N. Concurrent collagenous colitis and multiple ileal carcinoids. Dig Dis Sci. 1988;33:1040–4. doi: 10.1007/BF01536004. [DOI] [PubMed] [Google Scholar]
- 17.Freeman HJ, Berean KW. Resolution of paraneoplastic collagenous enterocolitis after resection of colon cancer. Can J Gastroenterol. 2006;20:357–60. doi: 10.1155/2006/893928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giardiello FM, Jackson FW, Lazenby AJ. Metachronous occurrence of collagenous colitis and ulcerative colitis. Gut. 1991;32:447–9. doi: 10.1136/gut.32.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pokorny CS, Kneale KL, Henderson CJ. Progression of collagenous colitis to ulcerative colitis. J Clin Gastroenterol. 2001;32:435–8. doi: 10.1097/00004836-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Aqel B, Bishop M, Krishna M, Cangemi J. Collagenous colitis evolving into ulcerative colitis: A case report and review of the literature. Dig Dis Sci. 2003;48:2323–7. doi: 10.1023/b:ddas.0000007870.18891.10. [DOI] [PubMed] [Google Scholar]
- 21.Smith P, Bishop P, Whorwell PJ. Collagenous colitis, ulcerative colitis, celiac disease and hyperparathyroidism in one patient: Implications for management of collagenous colitis. Eur J Gastroenterol Hepatol. 2005;17:1239–42. doi: 10.1097/00042737-200511000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Jessurun J, Yardley JH, Giardiello FM, Hamilton SR, Bayless TM. Chronic colitis with thickening of the subepithelial collagen layer (collagenous colitis): Histopathologic findings in 15 patients. Hum Pathol. 1987;18:839–48. doi: 10.1016/s0046-8177(87)80059-x. [DOI] [PubMed] [Google Scholar]
- 23.Bohr J, Tysk C, Eriksson S, Abrahamsson H, Jarnerot G. Collagenous colitis: A retrospective study of clinical presentation and treatment in 163 patients. Gut. 1996;39:846–51. doi: 10.1136/gut.39.6.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chutkan R, Sternthal M, Janowitz HD. A family with collagenous colitis, ulcerative colitis, and Crohn’s disease. Am J Gastroenterol. 2000;95:3640–1. doi: 10.1111/j.1572-0241.2000.03388.x. [DOI] [PubMed] [Google Scholar]
- 25.Giardiello FM, Lazenby AJ, Yardley JH, et al. Increased HLA A1 and diminished HLA A3 in lymphocytic colitis compared to controls and patients with collagenous colitis. Dig Dis Sci. 1992;37:496–9. doi: 10.1007/BF01307569. [DOI] [PubMed] [Google Scholar]
- 26.Kucharzik T, Walsh SV, Chen J, Parkos CA, Nusrat A. Neutrophil transmigration in inflammatory bowel disease is associated with differential expression of epithelial intercellular junction proteins. Am J Pathol. 2001;159:2001–9. doi: 10.1016/S0002-9440(10)63051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perner A, Nordgaard I, Matzen P, Rask-Madsen J. Colonic production of nitric oxide gas in ulcerative colitis, collagenous colitis and uninflamed bowel. Scand J Gastroenterol. 2002;37:183–8. doi: 10.1080/003655202753416858. [DOI] [PubMed] [Google Scholar]
- 28.Andresen L, Jorgensen VL, Perner A, Hansen A, Eugen-Olsen J, Rask-Madsen J. Activation of nuclear factor kappaB in colonic mucosa from patients with collagenous and ulcerative colitis. Gut. 2005;54:503–9. doi: 10.1136/gut.2003.034165. [DOI] [PMC free article] [PubMed] [Google Scholar]