Abstract
OBJECTIVES
To evaluate the proportion of EMS requests in a rural community made by unique, non-institutionalized, older adults, or individuals making their first request of EMS services during the study period, and the impact on research parameters.
METHODS
This study was a retrospective chart review of patients age 65 and older cared for by the Geneseo Fire Department Ambulance between February 2004 – May 2005 (period 1), and July 2006 – October 2007 (period 2). The Geneseo Fire Department Ambulance response territory is a rural community in Upstate New York. We obtained demographic information including age, race, gender, call location, and the frequency of EMS use from the medical record, as well as clinical information including level of prehospital care, chief complaint, and disposition. Descriptive statistics were used for the analysis, along with 95% confidence intervals.
RESULTS
Over two 16-month periods, approximately 70% of the EMS calls by community dwelling (non-institutionalized) older adults were from unique individuals. The monthly proportion ranged from between 75–100% during the first four months to between 43–80% for the remaining 12 months for both groups.
CONCLUSION
In rural, prehospital studies that enroll older adults and last more than four months, approximately 70% of EMS requests are made by unique older adults, or individuals making their first request of EMS services. Investigators must consider these results when estimating the enrollment period for prehospital studies.
Keywords: Emergency medical services, Prehospital care, Research methods, Geriatrics
Introduction
Identifying and enrolling sufficient numbers of subjects in clinical research studies is an ongoing challenge faced by investigators. Difficulties accruing subjects result in extended enrollment periods or underpowered studies with a high likelihood of Type II errors, which in turn may result in resource and ethical issues. 1 Enrollment periods that extend beyond initial projections are increasingly common and require additional resources, from both personnel and non-personnel, to sustain recruitment activities.2,3,4 Underpowered studies, resulting from an insufficient number of subjects to perform the proper statistical analyses are not only a potential waste of financial resources and investigator effort, but more importantly raise ethical concerns of exposing subjects to research risks unnecessarily, without benefits to the individual or community.2, 5, 6, 7
Investigators are well known to over-estimate their potential to recruit sufficient numbers of subjects, a phenomenon described as Lasagna’s Law.8 Evidence to inform recruitment estimates is lacking in many areas. Investigators seeking to study prehospital care often must estimate the proportion of emergency medical services (EMS) requests that arise from unique subjects, or individuals making their first request of EMS services during a study period. For many studies, subjects cannot be repeatedly enrolled in the study protocol; therefore, using unadjusted EMS case volumes would significantly over-estimate the number of eligible subjects.9, 10 The over-estimation problem may be further exacerbated when recruitment is limited to older adults (age≥65) because of their relatively high rates of EMS use, which may increase the probability of repeat use.11 The only published study that sought to quantify this phenomenon in an urban community showed that only 78% of EMS calls by older adults were from unique individuals.9 No other studies were identified that could be useful in guiding investigators developing estimates for prehospital studies recruiting older adults in rural settings. The objective of this study was to quantify the proportion of EMS requests in a rural community made by unique, community-dwelling, older adults.
Methods
Study Design
This study was a retrospective review of prehospital medical records from a rural New York community. The medical records from two separate 16-month periods, February 2004 to May 2005 (Period One) and July 2006 and October 2007 (Period Two), were reviewed. We delayed starting the second period to eliminate the impact of a significant increased demand for mutual aid throughout the County, resulting from the skilled nursing home moving to a neighboring EMS district. . The University of Rochester’s Research Subjects Review Board approved the study.
Study Setting
Livingston County is a rural county in Upstate New York with 64,328 residents in 2000. The Geneseo Fire Department (GFD), located in Livingston County, primarily provides service to Geneseo and Groveland, New York. Together the communities of Geneseo and Groveland had 1,011 residents aged 65 and older in 2000. Of the older adult population, 409 (40%) were male and 602 (60%) were female. 712 (70%) had at least a high school diploma, and 985 (97%) were white.12 There was one nursing home in Geneseo, NY, during the first 16-month period. By Period Two the nursing home had moved out of the service territory. One adult living community (neither assisted living nor independent living under New York regulations) existed during both periods.
GFD is a volunteer EMS agency staffed by emergency medical technicians (EMTs) trained at the basic life support level. Requests for assistance are processed by a county-operated emergency communications center that dispatches EMS assistance for the EMS agency based upon the call location. GFD does not provide interfacility transport services, only 911 originated emergency responses. A mutual aid system is also used. GFD responds outside its primary service areas if another area’s EMS resources are unavailable. Similarly, other agencies respond into Geneseo or Groveland if no GFD ambulances are available. Advanced life support care is provided on GFD ambulances by a county-wide, flycar based agency. GFD creates a medical record for every patient to which they are dispatched, regardless of the patient outcome or level of prehospital care provided.
The prehospital medical record for the study period was paper-based. Most responses were narrative, such as the name, address, and chief complaint, but some were checkboxes from a list, such as location of call. Some of the data, although written by the EMS provider, derived from the 911 dispatch center.
Protocol
A single reviewer (PS) using a standard data abstraction form abstracted all EMS medical records from the GFD for both Period One and Two. Data abstracted included date of call; setting of call (nursing home, private residence, street/highway, medical facility, and other); patient full name, permanent address, age, gender, and race; primary EMS chief complaint; patient disposition (hospital, refused transport); and level of care provided. Data unavailable for any of these variables were identified as missing and categorized as such. Two investigators (MNS, PS) coded chief complaints into 10 different categories found in Table 1. The two investigators jointly resolved any discrepancies in the categorization through discussion.
Table 1.
Demographic and EMS Call Characteristics by Time Period
| Period One | Period One (Adjusted*) | Period Two | |
|---|---|---|---|
| Total Calls | 577 | 394 | 386 |
| #(%) | #(%) | #(%) | |
| Unique EMS Patients | 409 (71) | 290 (74) | 274 (71) |
| Age, years (average, standard deviation) | 80.8 (7.8) | 80.3 (7.7%) | 81.98 (7.4) |
| Gender, Female | 325 (56) | 215 (55) | 210 (54) |
| Race | |||
| White | 402 (70) | 271 (69) | 315 (82) |
| African American | 4 (0.7) | 0 | 3 (0.8) |
| Other | 1 (0.2) | 1 (0.2) | 2 (0.5) |
| Not Reported/Unknown | 170 (29%) | 122 (31) | 66 (17) |
| Type of Location | |||
| Residence | 316 (55) | 316 (80) | 315 (82) |
| Skilled Nursing Facility | 183 (32) | 0 (0) | 0 (0) |
| Street/Highway | 23 (4.0) | 23 (5.8) | 16 (4.2) |
| Medical Facility | 32 (5.5) | 32 (8.2) | 31 (8.0) |
| Other | 23 (4.0) | 23 (5.8) | 24 (6.2) |
| Level of Care | |||
| ALS Care | 373 (65) | 237 (60) | 215 (56) |
| BLS Care | 204 (35) | 157 (40) | 170 (44) |
| Disposition | |||
| Hospital | 564 (98) | 381 (97) | 357 (92) |
| Refusal | 13 (2.2) | 13 (3.3) | 29 (7.5) |
| Chief Complaint | |||
| Traumatic Injury | 96 (17) | 79 (20) | 77 (20) |
| Respiratory | 98 (17) | 51 (14) | 54 (14) |
| Cardiac Related | 88 (15) | 57 (15) | 41 (11) |
| Gastrointestinal Complaint | 19 (3.3) | 8 (2.0) | 27 (7.0) |
| General Illness | 60 (10) | 42 (11) | 39 (10) |
| Pain (non-traumatic) | 70 (12) | 55 (14) | 27 (7.0) |
| Mental status changes | 22 (3.8) | 12 (3.0) | 27 (7.0) |
| Stroke | 14 (2.4) | 9 (2.3) | 8 (2.1) |
| Syncope | 32 (5.6) | 25 (6.4) | 27 (7.0) |
| Other | 78 (14) | 56 (14) | 59 (15) |
Adjusted: Nursing Home Patients Excluded
Using the abstracted data, all patients were individually identified by comparing the first and last names, age, gender, and permanent address. The study team viewed these criteria as sufficiently unique to correctly identify patients and allow for comparisons to identify duplicate patients.13 All data were entered into a Microsoft Excel (Microsoft Corp., Redmond, WA) spreadsheet.
The first EMS call for each patient during each period was considered the “unique EMS call” to identify the earliest point that a patient could have been identified as a study subject. All subsequent calls during that period were considered repeat EMS calls.
Data Analysis
We used Stata 8.0 (Stata Corp., College Station, TX) to analyze the data. The population of community-dwelling older adults using EMS services was characterized for each time period. Period One data were also adjusted to exclude nursing home patients (called Period One, Adjusted), thus simulating the absence of the nursing home from the EMS district. Characteristics evaluated included: age, race, gender, call location, level of prehospital care (advanced vs. basic life support), chief complaint, disposition (hospital vs. refused transport), and whether the EMS use was unique (the first time that patient accessed EMS care during the time period) or a repeat use. Standard descriptive statistics were used for the analysis.
To assess potential community-dwelling subject availability for enrollment in a study, we calculated the overall proportion of EMS calls that were unique, and then stratified the patients chronologically by service month. Additionally, we calculated three month moving averages of the first-call proportion to smooth month to month variability by using the Stata 8.0 “egen, ma” command. Our calculations were performed for both periods, and repeated for the first period after excluding nursing home patients (Period One, Adjusted). For all proportions, 95% confidence intervals were calculated using Stata 8.0 software.
Results
During Period One, the record review identified a total of 577 EMS calls for patients aged 65 and older. During Period Two, this age group only represented 386 records. The numeric difference between the two periods was thought to be due to the nursing home moving out of the EMS district. This was confirmed as after we excluded the nursing home calls from Period One, 394 calls remained (Period One, Adjusted). In all three scenarios (Period One, Period One Adjusted, and Period Two), unique patients comprised between 70% and 75% of all EMS calls.
Table 1 depicts the patient demographic and EMS call characteristics. All three scenarios, Period One, Period One Adjusted, and Period Two shared a number of characteristics. The patients tended to be older, with an average age exceeding 80; to be female; to be white; and to require advanced life support care. A difference in the location of the call and chief complaints was seen, as would be expected given that the skilled nursing facility was only open during Period One.
The overall proportion of unique, community-dwelling older adult patients who accessed EMS during the study periods was not statistically different (Period 1 Adjusted: 74%, 95% CI 70–79%, Period Two: 71%, 95% CI 64–74% (Table 2)). No statistically significant differences were found when comparing the proportion of unique older adult patients, as stratified by age and gender.
Table 2.
Proportion of Unique Older Adults Accessing EMS Across Patient Characteristics
| Proportion of Unique EMS Patients During Period One Adjusted* | Proportion of Unique EMS Patients During Period Two | |
|---|---|---|
| % unique patients 95% CI(Number of unique patients/Number of total patients) | % unique patients 95% CI(Number of unique patients/Number of total patients) | |
| All EMS Patients | 74%
70–79% (290/394) |
71%
64–74% (274/386) |
| Patients 65–80 years old | 81%
75–86% (161/198) |
74%
66–81% (105/141) |
| Patients >80 years old | 68%
61–75% (134/196) |
69%
63–75% (169/245) |
| Female Patients | 77%
71–82% (165/215) |
74%
68–80% (156/210) |
| Male Patients | 73%
65–79% (130/179) |
67%
60–74% (118/176) |
Adjusted: Nursing Home Patients Excluded
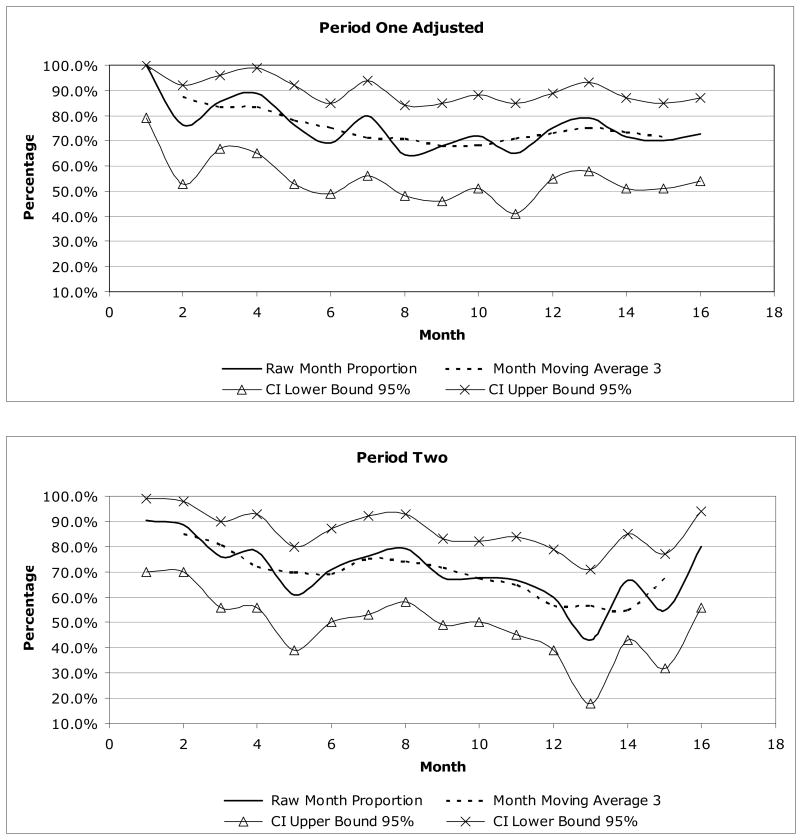
The monthly proportion of unique individuals who were patients for Period One Adjusted and Period Two ranged from highs of 100% and 90% during the first few months to lows of 64% and 43%, which were not reached until month 8 and 13 respectively (Table 3). The proportion of unique individuals who were EMS older adult patients was higher for the first few months as all patients accessing EMS would be considered unique until they had a subsequent EMS service call. The monthly proportion of unique community-dwelling patients during Period One Adjusted never exceeded 80% after month 4 and this proportion was never exceeded after month 3 for Period 2. Following these declines, the monthly proportion of unique patients ranged between 64 and 79% for Period One Adjusted, and between 43 and 80% for Period Two. After compensating for the initial higher rates by eliminating the results from the first four months, the proportion of unique patients in Period One Adjusted stabilized at a monthly average rate of 72%. For Period Two the proportion stabilized at a monthly average rate of 67%.
Table 3.
Proportion of Unique Older Adult EMS Patients Over Time
| Period One, Adjusted* | Period Two | |||
|---|---|---|---|---|
| Month | Proportion Unique Proportion/percent/95% CI | 3 Month Average | Proportion Unique Proportion/percent/95% CI | 3 Month Average |
| 1 | 16/16 (100.0%) 79–100% | N/A | 19/21 (90.5%) 70–99% | N/A |
| 2 | 16/21 (76.2%) 53–92% | 87.3% | 23/26 (88.5%) 70–98% | 84.9% |
| 3 | 24/28 (85.7%) 67–96% | 83.4% | 22/29 (75.9%) 56–93% | 80.8% |
| 4 | 16/18 (88.9%) 65–99% | 83.6% | 18/23 (78.3%) 39–80% | 72.0% |
| 5 | 16/21 (76.2%) 53–92% | 78.0% | 14/23 (60.9%) 50–87% | 70.0% |
| 6 | 20/29 (69.0%) 49–85% | 75.1% | 17/24 (70.8%) 58–93% | 69.3% |
| 7 | 16/20 (80.0%) 56–94% | 71.1% | 16/21 (76.2%) 53–92% | 75.4% |
| 8 | 18/28 (64.3%) 48–84% | 70.8% | 19/24 (79.2%) 58–93% | 74.3% |
| 9 | 17/25 (68.0%) 46–85% | 68.1% | 23/34 (67.7%) 49–83% | 71.5% |
| 10 | 18/25 (72.0%) 51–88% | 68.3% | 25/37 (67.3%) 50–82% | 67.3% |
| 11 | 13/20 (65.0%) 41–85% | 70.7% | 16/24 (64.7%) 45–84% | 64.7% |
| 12 | 21/28 (75.0%) 55–89% | 73.1% | 15/25 (60.0%) 39–79% | 56.5% |
| 13 | 19/24 (79.2%) 58–93% | 75.2% | 6/14 (42.9%) 18–71% | 56.5% |
| 14 | 20/28 (71.4%) 51–87% | 73.5% | 14/21 (66.8%) 43–77% | 54.8% |
| 15 | 21/30 (70.0%) 51–85% | 71.4% | 11/20 (55.0%) 32–77% | 67.2% |
| 16 | 24/33 (72.7%) 54–87% | N/A | 16/20 (80.0%) 56–94% | N/A |
Adjusted: Nursing Home Patients Excluded
We adjusted for month to month variability through calculating three month moving averages, as depicted in Figure 1 and Table 3. The data demonstrate that after month 4, Period One Adjusted variation narrowed to between 68 and 78%. For Period Two the variation after month four narrowed to 55 to 75%, similar to Period One Adjusted.
Figure 1.
Proportion of Unique EMS Patients: 3 Month Rolling Averages
Discussion
In this study, we have observed that without adjustments, researchers could overestimate the potential recruitment capabilities for rural, prehospital studies that enroll older adults and last more than three months by approximately 30%. This further complicates recruitment estimation. Many other challenges related to recruitment and consent face investigators undertaking prehospital studies that will further reduce enrollment. Subject-dependent difficulties such as subjects’ beliefs regarding research during in an emergency setting and limitations from acute disease process exist. Additionally, this type of research occurs in an uncontrolled environment with time constraints related to required immediate medical needs. Furthermore, the research requires coordinating a large number of stakeholders to support the studies, including training and coordinating the large numbers of emergency medical technicians and paramedics participating in the studies.14, 15, 16, 17, 18, 19
Our findings indicate that over two 16-month periods, approximately 70% of the EMS calls by community-dwelling older adults were from individuals who were unique persons. Our results were slightly lower than the 78% reported in a urban study.9 This difference may be due to methodological differences as Weiss et al based their calculations on patients transported to a single institution while this study was community-based. Alternatively, the differences may result from the variation in setting, as theirs took place in an urban community while this study used EMS calls from a rural community.
Interestingly, the monthly proportion of unique patients dropped significantly after approximately the fourth month of the study and approached the average unique proportion only after six months. Thus researchers who conduct pilot studies to determine their proportion of unique patients may overestimate their potential recruitment if the pilot is limited to less than four months.
We did find that those over age 80 years had a slightly lower proportion of calls for unique patients, as compared to those aged 65 to 80 years old and men had a slightly lower proportion, as compared to women. Neither of these differences were statistically significant, which was not surprising because the study was not powered to evaluate these differences. Despite the lack of power they may have meaning, especially to those who plan studies requiring the enrollment of large numbers of subjects, and must be carefully considered by EMS researchers in their studies.
When designing prehospital clinical studies, an imperative ethical and procedural issue is ensuring that the study will enroll a sufficient number of subjects. Investigators can use these empirical data to better estimate the study enrollment period. Thus, investigators can decrease the likelihood of proposing or undertaking trials with too few subjects to detect clinically and statistically significant effects, thus avoiding studies that are wasteful, unethical, and/or potentially misleading.
Future studies should examine the characteristics of the older adult population in the community, and the impact of those characteristics on the proportion of EMS calls by unique older adults. For instance, the impact of factors such as the burden of comorbidities, the proportion of the population in assisted living facilities, and the difficulty of accessing emergency care on recidivism would help researchers estimate recruitment numbers. Furthermore, this information may result in actions to improve the recruitment rates.
Limitations
This study employed a retrospective chart review that relied on previously collected data that cannot be verified for accuracy nor corrected if there were missing data. Second, because other EMS agencies did provide mutual aid in Geneseo and Groveland when the GFD ambulance was caring for another patient, the total number of requests for assistance does not represent the full number of calls in Geneseo and Groveland. However, this would be experienced by any rural prehospital researcher and must be considered by the researcher. Third, EMS documentation is known to be unreliable. It is possible that systematic errors biased the data. However, the variables used for the primary analyses were unambiguous and are required for reporting to New York State, thus tend to be well documented. Fourth, censoring occurred when subjects moved out of the response district or died after the initial call for EMS. This could bias the results, although the direction of the bias is difficult to determine given lack of extended follow up. Fifth, the generalizability of our findings to other EMS areas is limited. However, despite these limitations this study does provide useful information for investigators as they develop prehospital studies.
Conclusion
In rural, prehospital studies that enroll community-dwelling older adults and last more than four months, approximately 70% of EMS requests are made by unique older adults, or individuals making their first request of EMS services. Investigators must consider these results when estimating the enrollment period for prehospital studies.
Acknowledgments
Dr. Shah is supported by the Paul B. Beeson Career Development Award (NIA 1K23AG028942).
We would like to thank Duncan Ververs, Jennifer Williams, and the EMS providers from Geneseo Fire Department Ambulance for their assistance.
References
- 1.Pocock SJ. Size of cancer clinical trials and stopping rules. Br J Cancer. 1978;38:757–766. doi: 10.1038/bjc.1978.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charlson M, Horwitz R. Applying results of randomized trials to clinical practice: Impact of losses before randomization. British Medical Journal. 1984;289:1281–1284. doi: 10.1136/bmj.289.6454.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foy R, Parry J, Duggan A, et al. How evidence based are recruitment strategies to randomized controlled trials in primary care? Experience from seven studies. Family Practice. 2003;20:83–92. doi: 10.1093/fampra/20.1.83. [DOI] [PubMed] [Google Scholar]
- 4.Lovato LC, Hill K, Hertert S, Hunninghake DB, Probstfield JL. Recruitment for Controlled Clinical Trials: Literature Summary and Annotated Bibliography. Controlled Clin Trials. 1997;18:328–357. doi: 10.1016/s0197-2456(96)00236-x. [DOI] [PubMed] [Google Scholar]
- 5.Friedman LM, Furberg CD, Demets DL. Fundamentals of Clinical Trials. 3. New York, NY: Springer Science+Business Media, Inc; 1998. pp. 140–155. [Google Scholar]
- 6.Hully Cummings. Designing Clinical Research. II. Philadelphia PA: Lippincott Williams and Wilkins; 2001. [Google Scholar]
- 7.Raeburn Pauk. Commentary: Not Enough Patients? Don’t Do the Study, SCIENCE & TECHNOLOGY. [Retrieved July 7, 2007];2002 October, 21; http://www.businessweek.com/magazine/content/02_42/b3804106.htm.
- 8.McDonald AM, Knight RC, Campbell MK, Entwistle VA, Grant VM, Cook JA, Elbourne DR, Francis D, Garcia J, Roberts I, Snowdon C. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials. 2006;7:9. doi: 10.1186/1745-6215-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss SJ, Ernst AA, Miller P, Russell S. Repeat EMS Transports Among Elderly Emergency Department Patients. Prehospital Emergency Care. 2002;6:6–10. doi: 10.1080/10903120290938698. [DOI] [PubMed] [Google Scholar]
- 10.Pendergast HM, Jurivich D, Boxley C, Thomas R. Repeat Visits Among Elders in an Urban Emergency Department. [Accessed June 8, 2008];The Internet Jounal of Geriatrics and Gerontology. 2005 2(1) Available at: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijgg/vol2n1/visits.xml.
- 11.Shah MN, Bazarian JJ, Lerner EB, Fairbanks RJ, Barker W, Auinger P, Friedman B. The epidemiology of emergency medical services use by older adults: an analysis of the National Hospital Ambulatory Medical Care Survey. Academic Emergency Medicine. 2007;14:441–447. doi: 10.1197/j.aem.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 12.American FactFinder [on-line]. U.S. Census Bureau. [Accessed September 3, 2005]; Available at www.factfinder.census.gov.
- 13.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Academic Emergency Medicine. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 14.Ory MG, Lipman PD, Karlen PL, et al. Recruitment of older participants in frailty/injury prevention studies. Prevention Science. 2002;3:1–22. doi: 10.1023/a:1014610325059. [DOI] [PubMed] [Google Scholar]
- 15.Adams J, Silverman M, Musa D, Peele P. Recruiting older adults for clinical trials. Controlled Clin Trials. 1997;18:14–26. doi: 10.1016/s0197-2456(96)00132-8. [DOI] [PubMed] [Google Scholar]
- 16.Cassidy EL, Baird E, Sheikh JI. Recruitment and retention of elderly patients in clinical trials. Am J Geriatr Psychiatry. 2001;9:136–140. [PubMed] [Google Scholar]
- 17.Tolmie EP, Mungall MMB, Louden G, et al. Understanding why older people participate in clinical trials: the experience of the Scottish PROSPER participants. Age and Ageing. 2004;33:374–378. doi: 10.1093/ageing/afh109. [DOI] [PubMed] [Google Scholar]
- 18.Stahl SM, Vasquez L. Approaches to improving recruitment and retention of minority elders participating in research. Journal of Aging and Health. 2004;16:9S–17S. doi: 10.1177/0898264304268146. [DOI] [PubMed] [Google Scholar]
- 19.Resnick B, Concha B, Burgess JG, et al. Recruitment of older women: Lessons learned from the Baltimore hip studies. Nursing Research. 2003;52:270–273. doi: 10.1097/00006199-200307000-00010. [DOI] [PubMed] [Google Scholar]