Abstract
Hostility is a multifaceted construct encompassing affective, behavioral, and cognitive aspects. There is preliminary evidence linking hostility to poorer outcomes in smoking cessation treatment; however, it is unclear which components of hostility are most important in cessation. In this study, we examined multiple aspects of trait hostility in 92 heavy social drinkers who were seeking smoking cessation treatment. Consistent with our hypothesis, we found that the cognitive component of hostility was most relevant to smoking cessation outcome. Specifically, those who expressed bitterness about their life and tended to believe that they had poor luck and had gotten a raw deal out of life had poor smoking cessation outcomes. Cognitive measures of hostility also predicted greater nicotine withdrawal symptoms one week after quitting smoking. Other components of hostility including anger and both physical and verbal aggression did not significantly predict smoking outcome or nicotine withdrawal. Further examination of how a hostile world view contributes to smoking cessation failure is warranted as this facet of hostility may prove a valuable target for smoking cessation interventions.
Keywords: smoking, smoking cessation, hostility, aggression, personality
The personality trait of hostility has been conceptualized both as a primarily cognitive construct involving cynical attitudes and a general mistrust of others, and as a multidimensional construct involving hostile attitudes, expressions of anger, and aggressive behavior (Miller, Smith, Turner, Guijarro, & Hallet, 1996). Hostility is correlated with the broader personality dimension of neuroticism as well as with trait depression and anxiety, but it remains conceptually and empirically distinct from these dimensions of negative emotionality tending to correlate more highly with more interpersonally-relevant traits such as agreeableness (Barefoot, Dodge, Peterson, Dahlstrom, & Williams, 1989; Lubin & Van Whitlock, 2002) and trait anger (Han, Weed, Calhoun, & Butcher, 1995; Smith & Frohm, 1985). Cross-sectional studies have consistently found that smokers have higher levels of hostility than non-smokers (cf., Bunde & Suls, 2006). In longitudinal studies, greater hostility has been associated with a lower odds of quitting smoking in a sample of college students followed for 20 years(Lipkus, Barefoot, Williams, & Siegler, 1994), in a community sample of 18–30 year-olds followed for 5 years (Iribarren et al., 2000), and in patients followed for 6 years after coronary angiography (Brummett et al., 2002). Recently, Kahler and colleagues (Kahler, Strong, Niaura, & Brown, 2004) found that higher trait hostility was associated with poor smoking cessation treatment outcome in a group of smokers with a history of past major depressive disorder. Taken together, these finding suggests that hostility may warrant further consideration as a potential target for interventions that address risk factors for poor smoking cessation outcome.
There are a number of reasons that high hostility may interfere with efforts to quit smoking. First, cynicism may lead people to discount health-promoting messages regarding a range of health behaviors (Barefoot et al., 1991). However, among smokers in cessation treatment, hostility is not significantly correlated with motivation for quitting smoking due to health concerns (Kahler et al., 2004). Hostility is related to an external locus of control (Vandervoort, Pamela, & Hamilton, 1997) and among smokers in cessation treatment, to stronger extrinsic social reasons for quitting smoking (Kahler et al., 2004). However, greater extrinsic social reasons for quitting do not appear to mediate the effect of hostility on smoking outcomes (Kahler et al., 2004).
Hostility may impact smoking cessation through social factors. Greater reactivity to lab-based social stressors is associated with greater cigarette craving and relapse (Niaura, Shadel, Britt, & Abrams, 2003). High hostiles are particularly reactive to social stressors (Llabre, Spitzer, Siegel, Saab, & Schneiderman, 2004; Miller et al., 1998; Suarez, Harlan, Peoples, & Williams, 1993; Suarez, Kuhn, Schanberg, Williams, & Zimmermann, 1998) and report a greater frequency of negative social interactions (Brondolo et al., 2003). Therefore high hostiles may be particularly vulnerable to the effects of social stress on smoking relapse. In addition, cynicism and mistrust could undermine the therapeutic relationship between high hostile individuals and their smoking cessation counselors, which in turn could have a damaging effect on engagement in treatment (Boardman, Catley, Grobe, Little, Ahluwalia, 2006).
Finally, hostility may contribute to difficulty quitting smoking through its association with negative affect. Research supports the prominent role of negative affect in smoking withdrawal and its relation to relapse (Kenford et al., 2002; Piasecki, Kenford, Smith, Fiore, & Baker, 1997). Smoking relapses often occur in situations involving negative moods such as anxiety, anger, and depression (Brandon, Tiffany, Obremski, & Baker, 1990; Marlatt & Gordon, 1980; Shiffman, 1982), and affective distress after quitting (Covey, Glassman, & Stetner, 1990; Ginsberg, Hall, Reus, & Muñoz, 1995; Kahler et al., 2002; West, Hajek, & Belcher, 1989) predicts poor outcome. Trait hostility is positively related to frequency of reports of anger and other negative emotions (Shapiro, Jamner, & Goldstein, 1997). Furthermore, nicotine appears to reduce reports of anger among high hostile but not low hostile individuals (Jamner, Shapiro, & Jarvik, 1999), which could make smoking a particularly powerful negative reinforcer for high hostile smokers. Therefore, high hostile smokers may be particularly vulnerable to negative moods and subsequent relapse when quitting smoking.
Although there are numerous potential explanations for hostility’s association with low rates of smoking cessation, a number of questions need to be addressed before the mechanisms linking hostility to poor smoking cessation treatment outcome can be more fully understood. In particular, the Kahler et al. (2004) treatment study requires replication as well as extension to address limitations in methodology and sample and to define more precisely the aspects of hostility that are most relevant to smoking outcomes. As with all of the longitudinal studies cited above that examined hostility and smoking cessation, Kahler et al. (2004) relied on the Cook-Medley Hostility Scale (Cook & Medley, 1954) to assess trait hostility. Although the Cook-Medley appears to predominantly be a measure of cynical hostility (Smith & Frohm, 1985), the 50 items on the Cook-Medley scale are heterogeneous reflecting the multidimensional nature of the hostility construct (Contrada & Jussim, 1992; Costa, Zonderman, McCrae, & Williams, 1986; Greenglass & Julkunen, 1991; Han et al., 1995; Steinberg & Jorgensen, 1996). This heterogeneity of Cook-Medley items makes it difficult to establish which aspects of hostility may be more or less related to certain poor health outcomes (Strong, Kahler, Greene, & Schinka, 2005). Use of a measure that focuses more narrowly on expectations of a hostile and oppositional interpersonal world, such as the recently developed 17-item version of the Cook-Medley scale (CM-17; Strong et al., 2005), could help clarify whether it is hostile interpersonal attitudes per se that predict poor outcomes.
A second way to refine further which aspects of hostility relate to smoking outcome is to use a well-specified multidimensional measure of related constructs such as the brief Buss and Perry Aggression Questionnaire (AQ; Bryant & Smith, 2001), which assesses physical aggression, verbal aggression, anger, and hostility. The hostility subscale on the brief AQ appears to tap a different aspect of the hostility construct compared to the CM-17. Specifically, AQ hostility items focus on a general cynicism about life, with item content relating to having bad luck, getting a raw deal out of life, and not getting the same breaks that others get. Administering the brief AQ and the CM-17 scale to the same sample of smokers can allow for comparison of the effects of two related, yet distinct and relatively homogeneous, measures of hostility on smoking outcomes. Also, the other subscales on the AQ allow for a strong test of discriminant validity, enabling examination of whether it is the cognitive components of hostility that most strongly predict smoking outcome or whether related behavioral and affective constructs such as anger or aggression are equally relevant. Although frequent experiences of anger may increase risk for smoking relapse as noted above, it is not clear theoretically that aggressive behaviors would directly impact smoking cessation.
In addition to discriminating between facets of cognitive hostility and between hostility and other facets of aggression, it is also important to examine whether hostility has unique effects on smoking outcomes that are independent from the effects of other measures of negative affect. Kahler et al. (2004) found that hostility predicted smoking outcome beyond the effects of current depressive symptoms, a finding that requires replication. However, that study did not contain a measure of trait negative emotionality or neuroticism. Determining whether hostility’s effects on smoking outcome extend beyond the effects of general negative emotionality can help guide the development of future smoking cessation interventions by indicating whether a specific intervention focused on facets of hostility may be indicated for certain smokers rather than a more general mood management treatment.
The present investigation was conducted to replicate and extend the primary finding of the Kahler et al. (2004) study regarding the role of hostility in predicting poor smoking cessation treatment outcome. First, the sample in the present study was not selected for having a history of major depressive disorder (MDD). Second, in contrast to the Kahler et al. (2004) study, in which no pharmacotherapy was provided, all participants received transdermal nicotine patch making the treatment in the present study more consistent with current best practices. Third, by using two distinct and relatively unidimensional measures of trait hostility, we sought to better understand the relationship between hostility and smoking cessation outcome. Furthermore, by incorporating measures of anger, aggression and negative emotionality we sought to test further the discriminant predictive validity of trait hostility in a smoking cessation study.
We also sought to replicate and extend the findings of Kahler et al. (2004) by examining hostility’s association with relevant demographic and clinical characteristics and by examining its relation to nicotine withdrawal after quitting. Kahler et al. (2004) found that although hostility was not related to greater negative mood upon quitting smoking, there was a trend which suggested that negative mood tended to reduce more slowly after quit date in those with greater hostility. Therefore, we hypothesized that greater hostility would be associated with reporting more nicotine withdrawal at one and two weeks after quit date but not at quit date itself.
Method
Participants
Participants were 92 smokers seeking cessation treatment in a clinical trial comparing standard smoking cessation treatment (ST) to smoking cessation treatment that incorporates a brief alcohol intervention (ST-BI) (see Kahler et al., in press, for a more detailed description). Participants were recruited through postings on community bulletin boards and newspaper and radio advertisements, which asked for social drinkers who wanted to quit smoking. Potential participants were screened by telephone before completing an intake interview, at which they signed a statement of informed consent approved by the Brown University Institutional Review Board.
Participants were included if they: (a) were at least 18 years old; (b) had regularly smoked cigarettes for at least one year; (c) were currently smoking at least 10 cigarettes per day; (d) were not using any other tobacco products or nicotine replacement; and (e) drank heavily according to NIAAA guidelines but were not dependent on alcohol (National Institute on Alcohol Abuse and Alcoholism, 1995): for men, >14 drinks per week or ≥5 drinks per occasion at least once per month over the past 12 months; for women, >7 drinks per week or ≥4 drinks per occasion at least once per month). Participants were excluded if they: (a) met full DSM-IV criteria for alcohol dependence in the past 12 months; (b) met criteria for other current psychoactive substance abuse or dependence (excluding nicotine dependence and alcohol abuse) in the past 12 months; (c) had a current affective disorder; (d) were psychotic or suicidal; (e) had an unstable medical condition that would suggest caution in the use of the nicotine patch (e.g., unstable angina, arrhythmia, recent congestive heart failure); (f) were currently pregnant or lactating or intended to become pregnant. Overall, 56.8% of participants calling into the study met preliminary eligibility criteria, of whom 61.3% completion their baseline interview. Of those completing the baseline interview, 68.0% were confirmed as eligible and enrolled in the trial. At baseline, 3.5% were ruled out for current major depression and 5.5% for current alcohol dependence.
The sample used in these analyses included only those who completed all measures examined. Because some measures were not added to the study until its latter phases, the sample represents only the final 92 out of 236 participants recruited in the trial. The sample used in these analyses was 42.4% female and 57.6% male. The mean age of the sample was 40.9 (SD = 12.7) years, and the median education was 13.0 (SD = 2.3) years. Almost all participants (85.8%) identified themselves as White, and 38.0% were married. At baseline, participants smoked an average of 22.0 (SD = 10.9) cigarettes per day and had been smoking for an average of 22.1 years (SD = 11.4). The sample mean on the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991) was 5.0 (SD =2.0).
Procedure
Forty-seven of the participants in this subsample were randomized to the ST condition, and 45 were randomized to the ST-BI condition. Treatment consisted of four individual counseling sessions over three weeks with the quit date occurring at session 2, one week after session 1. Sessions ranged in length from 70 minutes for session 1, 40 minutes for session 2, and 20 minutes each for sessions 3 and 4. Standard treatment was based on recent clinical practice guidelines (Fiore, Bailey, Cohen, & et al., 2000) and focused on problem solving regarding high-risk situations for smoking relapse, providing support within the treatment, and encouraging participants to seek support for quitting smoking outside of treatment (Kahler, Zvolensky, Goldstein, & Brown, 2003). All participants received treatment with transdermal nicotine patch with the initial dose starting at 21 mg for four weeks, followed by two weeks of 14 mg patch, and then two weeks of 7 mg patch.
The ST and ST-BI conditions were matched on amount of therapist contact time. In the ST condition, 40 minutes of session 1 and 20 minutes of session 2 were dedicated to teaching progressive muscle relaxation. In ST-BI, this same amount of time was dedicated to an in-depth discussion of the participant’s alcohol use, which included open-ended discussion of current drinking and smoking patterns, feedback on drinking levels and the risk of smoking relapse associated with drinking, and goal setting regarding changing drinking during smoking cessation. A brief, 5-minute, check-in regarding use of relaxation skills in ST or achievement of drinking goals in ST-BI was included in sessions 3 and 4. Because this study focuses on only a subset of participants in a larger clinical trial, we do not report treatment effects in this paper. Instead, we covary for treatment assignment. We did run analyses testing interactions between treatment condition and personality scores; these showed no significant interactions between any personality variable and treatment condition in predicting smoking cessation outcome.
Participants completed brief assessments of smoking status, nicotine withdrawal symptoms, and alcohol use at each treatment session (i.e., through 2 weeks after quit date). In addition, follow-ups were conducted at 8, 16, and 26 weeks after quit date. Prior to all assessments, participants provided a breath sample to confirm that they were alcohol-negative. Research assistants were not informed of treatment condition assignment.
Measures
Prior to treatment, participants provided demographic and other clinically relevant information. Depressive symptoms during the past week were measured using the Center for Epidemiologic Studies –Depression scale (CES-D; Radloff, 1977), a well-validated, 20-item self-report scale that has been widely used as a measure of depression in nonclinical samples (Cronbach’s α = .90 in the present sample). Lifetime history of MDD was assessed using the Structured Clinical Interview for DSM-IV (Spitzer, Williams, Gibbon, & First, 1990). Severity of nicotine dependence was assessed using the FTND (Heatherton et al., 1991), a well-validated 6-item measure (α = .62). The 8-item Commitment to Quitting Smoking Scale (CQSS; Kahler et al., 2007) was used assess an individuals’ commitment to quit smoking (α = .91). The CQSS has good psychometric properties and predictive validity (Kahler et al., 2007).
Personality Measures
Trait hostility was measured with the 17-item abbreviated version of the MMPI – based Cook-Medley hostility scale (Strong et al., 2005). This scale was developed using a Rasch model analysis of the 50 Cook-Medley items to extract a unidimensional subset of items that represents the primary latent construct assessed by the full scale. The content of the CM-17 items reflects a distrust and devaluation of others, expectations of deceit, and interpersonal guardedness (e.g., “Most people make friends because friends are likely to be useful to them,” α = .82). Items are assessed with a true-false scale, and the total score is the sum of “true” responses.
Trait hostility also was assessed using the abbreviated Aggression Questionnaire (AQ; Buss & Perry, 1992). The original version of the AQ consisted of 29 items; however, Bryant and Smith (2001) proposed a refined measurement model with an improved fit which consisted of 3 items per scale and has good psychometric properties (Bryant & Smith, 2001); Tremblay & Ewart, 2005). The refined version of the AQ consists of four subscales: Physical Aggression (e.g., “Given enough provocation, I may hit another person,” α = .78), Verbal Aggression (“My friends say that I am somewhat argumentative,” α = .76), Anger (“I have trouble controlling my temper,” α = .70), and Hostility (“At times I feel I have gotten a raw deal out of life,” α = .73). All items are rated on a 0 = extremely uncharacteristic of me to 5 = extremely characteristic of me Likert-type scale, and total scores are the mean of the items.
We used the 18-item Stress Reaction subscale (α = .90) of the Multidimensional Personality Questionnaire (MPQ; Tellegen, 1982) as a measure of a general tendency to be easily upset, nervous, sensitive, and prone to worry and guilt. The MPQ that has been well-validated in longitudinal and genetic research (Krueger, 2000; Roberts, Caspi, & Moffitt, 2001). All items are rated on a 0 = definitely false to 3 = definitely true scale. Total scores are the mean of the items.
Smoking Outcome Measures
Nicotine withdrawal
The 7-item Minnesota Nicotine Withdrawal Scale (MNWS; (J. Hughes & Hatsukami, 1998; J. R. Hughes & Hatsukami, 1986) was used to measure nicotine withdrawal at session 1 (α = .80), quit date (session 2; α = .85), 1 week after quit date (session 3; α = .84), and 2 weeks after quit date (session 4; α = .77). Response options range from 0 = none to 4 = severe Total scores are the sum of the 7 items.
Smoking status
Outcome analyses were based on 7-day point prevalence abstinence (i.e., reported abstinence of at least 7 days prior to the assessment day) as assessed at 2 (end of psychosocial treatment), 8 (end of treatment with the nicotine patch), 16, and 26 weeks after each participant’s quit date. Self-reported abstinence was verified by alveolar carbon monoxide (CO) using a Bedfont Scientific Smokelyzer® breath CO monitor. At 16- and 26-week follow-ups, a saliva sample for cotinine level determination by enzyme immunoassay was collected from those reporting abstinence. Abstinence was confirmed by a combination of CO ≤ 10 ppm and cotinine ≤ 15 ng/ml (SRNT Subcommittee on Biochemical Verification, 2002). Significant other report was used to verify smoking status for those who did not provide self-report data or did not provide biochemical verification of abstinence (a total of 3 assessments). Complete smoking data verified either biochemically or by significant other report was obtained from 93.5%, 94.5%, 91.3%, and 94.5% of participants at the 2-, 8-, 16-, and 26-week follow-ups, respectively. Only individuals who had smoking abstinence confirmed at a given follow-up were considered abstinent; those with missing data were considered non-abstinent.
Data Analysis Plan
As a first step, to determine the overlap of hostility with other key personality variables in the data set, we examined the correlations among the personality variables. We also examined the correlations between the personality variables and demographics (gender, age, race, years of education, and marital status), depression-related characteristics (MDD history and current depressive symptom severity), and level of level of nicotine dependence. We then examined the correlation between each of the personality characteristics and nicotine withdrawal symptoms on quit date, 1 week after quit date and 2 weeks after quit date, partialing out the effects of relevant demographic characteristics (i.e., those that correlated with hostility and could represent a confound), level of nicotine dependence and treatment condition. Finally, we examined differences in the personality variables between abstainers and non-abstainers at 2, 8, 16, and 26 weeks and then ran generalized estimating equations predicting 7-day point prevalence smoking abstinence across these follow-ups controlling for treatment assignment both with and without adjusting for relevant demographic factors, depressive symptoms, and level of nicotine dependence. All analyses used a two-tailed alpha of .05.
Results
Preliminary Analyses of Associations between Personality Variables and Clinical Characteristics
Correlations among each of the personality scales are presented in Table 1. Table 1 also shows each measure’s mean and standard deviation. There was a moderate degree of intercorrelation among the measures of hostility and aggression (i.e., the AQ subscales and the CM-17 scale; rs .37 – .64). In contrast, correlations between the MPQ-Stress Reaction subscale and the other personality variables were generally lower (rs .10 – .46).
Table 1.
Correlations Among Personality Variables
| Variable | M | SD | 1. | 2. | 3. | 4. | 5. | 6. |
|---|---|---|---|---|---|---|---|---|
| 1. Cook-Medley Hostility scale | 4.95 | 3.90 | - | |||||
| 2. AQ-Hostility subscalea | 1.18 | 1.04 | .44† | - | ||||
| 3. AQ-Anger subscalea | 1.09 | 0.99 | .41† | .60† | - | |||
| 4. AQ-Physical Aggression subscalea | 0.89 | 1.10 | .55† | .37*** | .47† | - | ||
| 5. AQ-Verbal Aggression subscalea | 1.12 | 1.00 | .52† | .50† | .64† | .51† | - | |
| 6. MPQ-Stress Reaction subscaleb | 1.21 | 0.51 | .31** | .46† | .34** | .10 | .26* | - |
Note. N = 92. AQ= Aggression Questionnaire; MPQ = Multidimensional Personality Questionnaire.
Means and SDs based on average response per item (possible range: 0–5).
Means and SDs based on average response per item (possible range: 0–3).
p < .05;
p < .01;
p < .001;
p < .0001
There were modest, but significant, correlations indicating that female, white, and older participants reported lower levels of hostility on the CM-17, rs = −.33, −.21, and −.23, respectively. Female (r = −.28) and white participants (r = −.28) also scored significantly lower on the AQ-physical aggression subscale but did not score differently on the other AQ subscales. Older participants had significantly lower scores on the AQ-verbal aggression subscale (r = −.21) and the MPQ-Stress Reaction scale (r = −.27). Severity of depression as assessed by the CESD (square-root transformed to correct positive skewness) was most strongly correlated with the MPQ-Stress Reaction subscale (r = .61) and the AQ-Hostility subscale (r = .47) and demonstrated modest associations with the other personality measures (rs = .18 – .30). Presence versus absence of MDD history did not associate with any of the personality measures. Only the MPQ-Stress Reaction subscale correlated with significantly greater FTND scores (r = .25). Personality variables did not correlate significantly with commitment to quitting smoking.
Associations between Personality Variables and Nicotine Withdrawal
Because nicotine withdrawal was assessed at each treatment session rather than at follow-up interviews, which were financially compensated, this variable had more missing data than the smoking abstinence variable. Completion rates ranged from 84.5% at session 2, to 73.8% at session 3, to 78.3% at session 4. At both session 2 and session 4, those who did not complete the MNWS reported significant more hostility on the baseline AQ-H compared to those who completed the measure; they did not differ on other personality scales. Those with missing MNWS data at a given session did not differ significantly from those with completed MNWS assessments on any other personality scale. Mean (SD) MNWS scores 1 week prior to quit date (session 1), on quit date (session 2), 1 week following quit date (session 3), and 2 weeks following quit date (session 4) were 4.84 (4.42), 4.83 (5.02), 5.73 (5.17), and 4.66 (4.31), respectively. Partial correlations between personality variables and MNWS scores were calculated adjusting for MNWS scores 1 week before quit date, FTND, treatment condition, and demographic characteristics that were found to significantly associate with personality variables (i.e., gender, age, race). Results showed that participants with higher scores on the CM-17 hostility scale [r(67) = .44, p < .001)] and the AQ-hostility [r(67) = .39), p < .01)] subscale reported significantly more severe withdrawal 1 week after quit date. The other personality variables did not significantly predict withdrawal at that assessment. In addition, none of the personality variables significantly predicted MNWS scores on either quit date or the 2-week post-quit date assessment.
It should be noted that some participants could have relapsed to smoking during the first two weeks following quit date, which could have affected MNWS scores assessed during that period and potential associations between withdrawal and personality. To account for this possibility, we recalculated the partial correlations between personality and MNWS scores above after adjusting for abstinence status 2 weeks following quit date. Results were generally unchanged with the minor exception that the association between AQ-Anger and MNWS assessed 1 week after quit date went from marginally significant (r = .24, p = .06) to statistically significant (r = .26, p = .046), after controlling for abstinence.
Associations between Personality Variables and Cessation Outcomes
Overall point-prevalence smoking abstinence rates at 2 weeks, 8 weeks (i.e.,post-treatment), 16, and 26 weeks following quit date were 50.0%, 32.6%, 18.5%, and 17.8%, respectively; the rate of continuous abstinence (i.e., reporting no smoking with confirmed abstinence at 2, 8, 16, and 26 weeks) was 12.0%. To show the association between abstinence at each follow-up and baseline personality scales, we present in Figure 1 the mean personality scale scores for those who were vs. those who were not abstinent at each follow-up. To allow for comparisons across personality measure, we standardized (z-scored) each personality scale. We then ran ANOVAs comparing baseline personality score between those who were and those who were abstinent at each follow-up. Results showed that those who were abstinent had lower precessation AQ-Hostility subscale scores than those who were not abstinent, with stronger effects for the later assessments: week 2, p = .12, Cohen’s d = .33; week 8, p = .047, d = .46; week 16, p = .01, d = .75; week 26, p = .01, d = .86. AQ-Anger scores did not differ by abstinence status on weeks 2 or 8, ps > .41. However, precessation AQ-Anger scores were marginally lower among abstinent participants at the week 16 follow up, p = .06, d = .51, and significantly lower among those who were abstinent at week 26, p = .02, d = .73. MPQ-Stress Reaction scores were marginally lower among abstinent participants at week 2, p = .07, d = .38, but did not differ by abstinence status at week 8, p = .21. MPQ-Stress Reaction scores were significantly lower among abstinent participants at week 16, p = .004, d = .77, and at week 26, p = .03, d = .64. There were no differences on CM-17, AQ-Verbal Aggression, and AQ-Physical Aggression scores between abstinent and non-abstinent participants at each follow up, Fs ≤ 1.93, ps ≥ .16. Those who were continuously abstinent had significantly lower AQ-Hostility scores than those who were not (p = .001, d = .75), but did not differ on any other scale, ps>.10.
Figure 1.
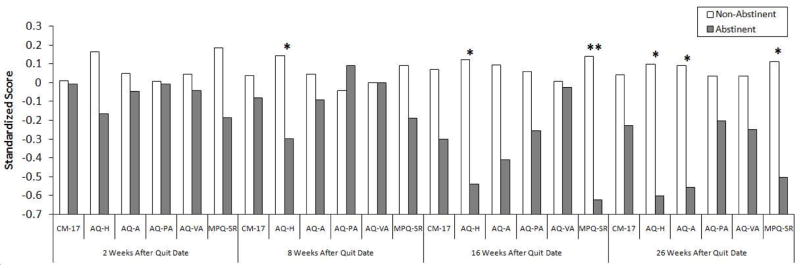
Standardized means of personality variables by abstinence status. Mean precessation scores for each personality scale are presented comparing those who are abstinent from smoking at each follow-up to those who are not abstinent at that follow-up. Standardized z scores are reported to ease interpretative comparisons across measures. CM-17 = 17-item Cook-Medley Hostility scale; AQ= Aggression Questionnaire; MPQ-SR = Multidimensional Personality Questionnaire-Stress Reaction subscale; H = Hostility subscale; A = Anger subscale; PA = Physical Aggression Subscale; VA = Verbal Aggression Subscale
Abstinent vs. Non-abstinent comparisons: *p < .05, **p < .01
GEE analyses of standardized personality variables predicting abstinence are reported in Table 2. Results showed that higher AQ-Hostility subscale scores were associated with significantly lower odds of abstinence, odds ratio (OR) = .63. That is, with each increase in one standard deviation in AQ-Hostility score, participants had 37% lower odds of being abstinent. The effects of AQ-Hostility on abstinence remained essentially unchanged and significant (OR = .63) when adjusting for demographics that were shown to associate with personality (i.e., gender, race, age), depressive symptoms (CES-D), and FTND scores (see Table 2). Higher scores on the MPQ-Stress Reaction subscale also predicted reduced odds of abstinence when unadjusted; OR = .64. However, when demographics, CES-D, and FTND were included in the model, the effect of the MPQ-Stress Reaction subscale on abstinence was nonsignificant; OR = .70, p = .18. Other personality measures failed to significantly predict abstinence in GEE analyses (see Table 2).
Table 2.
Generalized Estimation Equation Analyses of Standardized Personality Variables predicting 7-day Point Prevalence Smoking Abstinence at 2, 8, 16, and 26 weeks after quit date
| Unadjusted Effecta |
Adjusted Effectb |
|||
|---|---|---|---|---|
| Personality Variable | OR (95% CI) | p | OR (95% CI) | p |
| Cook-Medley Hostility, 17 items | .91 (.64–1.29) | .59 | .95 (.66–1.37) | .80 |
| AQ-Hostility subscale | .63 (.44–.91) | .01 | .63 (.41–.98) | .04 |
| AQ-Anger subscale | .81 (.57–1.14) | .22 | .88 (.62–1.24) | .46 |
| AQ-Physical Aggression subscale | .97 (.71–1.34) | .87 | 1.00 (.73–1.34) | .99 |
| AQ-Verbal Aggression subscale | .96 (.70–1.32) | .82 | 1.04 (.76–1.41) | .80 |
| MPQ-Stress Reaction subscale | .64 (.44–.93) | .02 | .70 (.42–1.17) | .18 |
Note. N = 92. ORs < 1 indicate that higher scores on the personality measure predict reduced odds of abstinence. OR = odds ratio of standardized scores (z-scores). AQ = Aggression Questionnaire; MPQ = Multidimensional Personality Questionnaire; CI = Confidence Interval FTND = Fagerström Test for Nicotine Dependence; CES-D = Center for Epidemiologic Studies - Depression Scale.
Model included only a personality variable and treatment condition as predictors.
Model included a personality variable, treatment condition, age, gender, race, CES-D, and FTND as predictors.
To test the extent to which AQ-Hostility predicted smoking abstinence beyond MPQ-Stress Reaction (the only other personality scale that significantly associated with outcome), both AQ-Hostility and MPQ-Stress Reaction were added to the adjusted GEE model controlling for demographics, CES-D, and FTND. The effect of AQ-Hostility was reduced to a slight degree with the inclusion of MPQ-Stress Reaction and was just over the threshold for significance; OR = .66, p = .08. The effect of MPQ-Stress Reaction was nonsignificant; OR = .77, p = .36.
Supplemental Analyses
Previous research demonstrating that hostility predicts smoking outcomes were demonstrated in a sample of smokers who were positive for past MDD (Kahler et al., 2004). This leaves unclear whether hostility’s effects on cessation occur only among smokers with a MDD history or whether effects generalize across smokers with and without an MDD history. To address this question, we conducted two supplemental GEE analyses. In the first set of models, we examined if hostility scores predicted outcome when adjusting for treatment condition, demographics (age, race, and gender), FTND, and MDD history (at least one past depressive episode versus no past episodes). We conducted separate GEE models for the AQ-Hostility scale and the CM-17. In this model using the AQ-Hostility scale, the effects of AQ-Hostility was significant, OR (95% CI) = .64 (.42–.98), p = .04, whereas MDD history had no effect, OR (95% CI) = 1.16 (.53–2.57), p = .71. In the model using the CM-17, both the CM-17 and MDD history were nonsignificant (ps > .47). We conducted a second set of GEE models that was identical to the first, except that it also included the interaction between MDD history and hostility as an additional predictor of abstinence. For both hostility variables, the interaction term was nonsignificant (ps >.60), indicating that the effect of hostility on cessation did not differ significantly between smokers with and without a history of MDD.
Discussion
Results of this study provide further evidence of the value of trait hostility in predicting smoking cessation treatment outcome and suggest the facets of hostility that appears particularly relevant to smoking outcomes. Consistent with Kahler et al (2004), we found that greater trait hostility was associated with significantly lower odds of smoking abstinence and predicted greater withdrawal symptoms one week after quitting smoking. However, the current study extended that of Kahler et al. (2004) in a number of important ways that are detailed below.
The Kahler et al. (2004) study measured hostility using only the total score from the 50-item Cook-Medley Hostility Scale. Given the heterogeneous item content of that scale, the specific facets of hostility that most strongly related to smoking outcome could not be identified. The present study included measures of the behavioral (verbal and physical aggression) and affective (anger) components of hostility. None of these measures significantly predicted nicotine withdrawal or smoking outcome in multivariate models. We also included two relatively unidimensional measures of the cognitive components of hostility, the 17-item Cook-Medley scale (CM-17) and the hostility subscale from the Aggression Questionnaire (AQ-H). The CM-17 focuses on expectations of a hostile and oppositional interpersonal world, while the AQ-H focuses on bitter and cynical cognitive content regarding one’s life in general. The CM-17 and AQ-H were moderately highly correlated (r = .44) and also correlated moderately highly with anger and both physical and verbal aggression. It was these two measures of hostile cognitive content, particularly the AQ-H, that appeared most relevant to smoking cessation.
Both measures of cognitive hostility were not associated with nicotine withdrawal symptoms on quit date but were positively associated with greater withdrawal at 1 week post quit date, as we had hypothesized. However, the hypothesized effect of hostility on withdrawal symptoms at 2 weeks was not found. This likely reflects the fact that withdrawal symptoms at week 2 were similar to baseline in the sample as whole, suggesting that even among those high in hostility, withdrawal effects were largely resolved within two weeks after quitting. The relatively low levels of withdrawal symptoms reported in the sample may reflect the fact that all participants received the nicotine patch. Also, individuals with missing withdrawal data at quit date and 2 weeks after quit date had higher AQ-H score than those completing these assessments; thus the effect of hostility may have been attenuated by selective missingness of withdrawal data.
Overall, results were consistent with the Kahler et al. (2004) study and suggest that individuals high in hostility may be prone to more prolonged nicotine withdrawal symptoms upon quitting smoking, an effect which is not due to differences in nicotine dependence severity, nor is eliminated by nicotine patch treatment. Individuals high in hostility have been shown to have greater emotional and physiological reactivity to certain interpersonal stressors, an effect that seems to be distinct from effects of neuroticism and depression. For example, when harassed during problem-solving tasks, high hostile participants show enhanced blood pressure, heart rate, norepinephrine, testosterone, and cortisol response relative to harassed low hostile participants and nonharassed high hostile participants (Llabre et al., 2004; Miller et al., 1998; Suarez et al., 1993; Suarez et al., 1998). Also, when recalling a self-chosen anger memory, high hostile participants show a larger and longer-lasting blood pressure response compared to low hostile participants (Fredrickson et al., 2000). The stress of quitting smoking and the effects of nicotine withdrawal may represent another stressor that high hostile individuals recover from more slowly, although the mechanisms that account for such an effect are unclear, nor is it clear why cognitive aspects of hostility but not stress reaction are related to nicotine withdrawal symptoms.
Although both measures of cognitive hostility related to withdrawal at week 1, only the AQ-H significantly predicted smoking abstinence over 6 months. The association between high AQ-H scores and poor smoking outcomes persisted even when controlling for demographic characteristics, depressive symptoms, and levels of nicotine dependence. We speculate that the cognitive content reflected in the AQ-H may be especially relevant to quitting smoking or possibly to behavior change as a whole. It may prove difficult for individuals to sustain changes in health-promoting behaviors if they view themselves as being the victims of bad luck. Individuals with this worldview might be prone to seeing their behavioral choices and their health as being outside of their personal control and doomed to failure, and therefore they may make less efforts to cope with challenges to remaining abstinent. However, such conjectures can not be directly tested with the data available in the present study.
In addition to examining a number of hostility-related constructs, the current study extended that of Kahler et al. (2004) in three other ways. First, we included a measure of trait negative emotionality to demonstrate the discriminant validity of the hostility and smoking cessation relationship. Although AQ-H and the measure of proneness to negative emotions (MPQ-Stress Reaction) were moderately highly correlated, 75% of their variance was unshared, allowing these constructs to show differential associations with smoking outcomes. Although Stress Reaction showed an association with smoking cessation outcome, the association was not significant in the GEE models that controlled for relevant demographic characteristics, depressive symptoms, and nicotine dependence. When both AQ-H and Stress Reaction were included in a GEE model predicting smoking outcome, the effect of AQ-H was just over the threshold for significance, whereas the Stress Reaction scale was clearly nonsignificant. These results suggest that although cognitive hostility and negative emotionality do overlap to some degree in their prediction of smoking cessation, hostility appears to be a more robust predictor. Furthermore, Stress Reaction did not predict withdrawal symptom severity, whereas both cognitive measures of hostility did, again highlighting the potentially unique role of hostility.
This study also included those with and without a history of MDD. One limitation to the Kahler et al. (2004) study was that it included only those individuals with a past history of MDD, making it difficult to generalize beyond that sample. Our results suggest that hostility is relevant to smoking outcome regardless of MDD history.
Finally, all participants in this study were provided transdermal nicotine patch. Among both smokers and nonsmokers high in hostility, nicotine patch has been shown to reduce the frequency of reports of anger and other negative moods compared to placebo patch during a 24-hr monitoring period (Jamner et al., 1999), an effect that was not found among those low in hostility. Those results suggest that nicotine patch might mitigate some of the effects of hostility on smoking cessation outcome and nicotine withdrawal. In the present study, the association between hostility and smoking outcome was least robust at the earlier follow-ups when nicotine patch was being used. It is possible, therefore, that nicotine patch mitigated the effects of hostility on early outcomes; however, a placebo-controlled study would be needed to confirm this possibility. Also, the inclusion of the nicotine patch might explain why the CM-17 did not significantly predict smoking abstinence in this study, while its close relative, the 50-item Cook-Medley, predicted outcome in the Kahler et al. (2004) study in which no participants received patch. Nonetheless, the fact that the AQ-H was a robust predictor of smoking outcome in the present study indicates that high hostility may predict poor smoking outcome even when nicotine replacement is used.
Limitations
In considering the results of the study, several limitations should be considered. First, our sample was of modest size, was primarily White, and included relatively heavy social drinkers who were seeking cessation treatment. The relationship between hostility and smoking cessation may differ in the general population of smokers. This study’s findings in combination with the Kahler et al. (2004) results suggest that hostility may be relevant to smoking cessation treatment outcomes across a range of populations. Nonetheless, generalization of each of the study findings to smokers who do not drink heavily must be made with caution.
Conclusions
There is now converging evidence that greater trait hostility predicts poor smoking cessation outcome. The current study found that constructs related to hostility such as anger, physical aggression, verbal aggression, and stress reaction did not significantly predict smoking abstinence beyond the effects of demographics, current depressive symptoms, and level of nicotine dependence. These findings provide additional evidence for the discriminant predictive validity of the hostility construct. Although the AQ-H and CM-17 both predicted withdrawal symptom severity one week after quitting, only the AQ-H predicted poor smoking cessation outcome. These findings suggest that individuals who are highly cynical and bitter about their own life may be at elevated risk of continued smoking. The accumulated evidence across the present study, Kahler et al. (2004), and other investigations of smoking and hostility (Brummett et al., 2002; Iribarren et al., 2000; Lipkus et al., 1994) suggest that it may be valuable to begin to develop and test interventions that integrate methods to reduce hostility into standard smoking cessation treatment. For example, initial studies have indicated that group-based cognitive behavioral interventions can reduce hostility as assessed by the Cook-Medley scale (Gidron & Davidson, 1996; Gidron, Davidson, &Bata, 1999). The components of these interventions that address cynical cognitive content may be particularly relevant. In addition, more research is needed to elucidate the cognitive and behavioral mechanisms through which cognitive hostility impacts smoking cessation treatment outcome and to develop a working model that integrates the role of hostility in smoking cessation with other related factors known to impact cessation outcomes such as negative affect, nicotine withdrawal, and social support for quitting.
Acknowledgments
This study was supported by grant R01 DA15534 from the National Institute on Drug Abuse to Christopher Kahler. Dr. Monti’s effort was supported in part by a Department of Veterans Affairs Senior Career Research Scientist Award. The authors gratefully acknowledge Andrea Resendes, Jennifer Larence, Dan Belenky, Catherine Costantino, Cheryl Eaton, Timothy Souza, Kara Szczesny, and Heather LaChance for their assistance on this project, as well as treatment providers John McGeary, Jane Metrik, Patricia Relli-Moniz, Gail Schilke, and James MacKillop.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/adb/
References
- Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB., Jr The Cook-Medley hostility scale: item content and ability to predict survival. Psychosomatic Medicine. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Peterson BL, Dahlstrom WG, Siegler IC, Anderson NB, Williams RB., Jr Hostility patterns and health implications: correlates of Cook-Medley Hostility Scale scores in a national survey. Health Psychology. 1991;10:18–24. doi: 10.1037//0278-6133.10.1.18. [DOI] [PubMed] [Google Scholar]
- Boardman T, Catley D, Grobe JE. Using motivational interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance? Journal of Substance Abuse Treatment. 2006;31:329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Tiffany ST, Obremski KM, Baker TB. Postcessation cigarette use: The process of relapse. Addictive Behaviors. 1990;15:105–114. doi: 10.1016/0306-4603(90)90013-n. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Rieppi R, Erickson SA, Bagiella E, Shapiro PA, McKinley P, et al. Hostility, interpersonal interactions, and ambulatory blood pressure. Psychosomatic Medicine. 2003;65:1003–1011. doi: 10.1097/01.psy.0000097329.53585.a1. [DOI] [PubMed] [Google Scholar]
- Brummett BH, Babyak MA, Mark DC, Williams RB, Siegler IC, Clapp-Channing N, et al. Predictors of smoking cessation in patients with a diagnosis of coronary artery disease. Journal of Cardiopulmonary Rehabilitation. 2002;22:143–147. doi: 10.1097/00008483-200205000-00003. [DOI] [PubMed] [Google Scholar]
- Bryant FB, Smith BD. Refining the architecture of agression: A measurement model for the Buss-Perry Agression Questionnaire. Journal of Research in Personality. 2001;35:138–167. [Google Scholar]
- Bunde J, Suls J. A quantitative analysis of the relationship between the Cook-Medley Hostility Scale and traditional coronary artery disease risk factors. Health Psychology. 2006;25:493–500. doi: 10.1037/0278-6133.25.4.493. [DOI] [PubMed] [Google Scholar]
- Buss AH, Perry M. The aggression questionnaire. Journal of Personality and Social Psycholology. 1992;63:452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Contrada RL, Jussim L. What does the Cook-Medley hostility scale measure? In search of an adequate measurement model. Journal of Applied Social Psychology. 1992;22:615–627. [Google Scholar]
- Cook WW, Medley DM. Proposed Hostility and Pharasaic-Virtue scales for the MMPI. Journal of Applied Psychology. 1954;38:414–418. [Google Scholar]
- Costa PT, Zonderman AB, McCrae RR, Williams RB. Cynicsm and paranoid alienation in the Cook Medley Ho Scale. Psychosomatic Medicine. 1986;48:283–285. doi: 10.1097/00006842-198603000-00014. [DOI] [PubMed] [Google Scholar]
- Covey LS, Glassman AH, Stetner F. Depression and depressive symptoms in smoking cessation. Comprehensive Psychiatry. 1990;31:350–354. doi: 10.1016/0010-440x(90)90042-q. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence: Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2000. [Google Scholar]
- Fredrickson BL, Maynard KE, Helms MJ, Haney TL, Siegler IC, Barefoot JC. Hostility predicts magnitude and duration of blood pressure response to anger. Jorunal of Behavioral Medicine. 2000;23:229–243. doi: 10.1023/a:1005596208324. [DOI] [PubMed] [Google Scholar]
- Gidron Y, Davidson K. Development and preliminary testing of a brief intervention for modifying CHD-predictive hostility components. Journal of Behavioral Medicine. 1996;19:203–220. doi: 10.1007/BF01857766. [DOI] [PubMed] [Google Scholar]
- Gidron Y, Davidson K, Bata I. The short-term effects of a hostility-reduction intervention on male coronary heart disease patients. Health Psychology. 1999;18:416–420. doi: 10.1037//0278-6133.18.4.416. [DOI] [PubMed] [Google Scholar]
- Ginsberg D, Hall SM, Reus VI, Muñoz RF. Mood and depression diagnosis in smoking cessation. Experimental and Clinical Psychopharmacology. 1995;3:389–395. [Google Scholar]
- Greenglass ER, Julkunen J. Cook-Medley hostility, anger, and the Type A behavior pattern in Finland. Psychological Reports. 1991;68:1059–1066. doi: 10.2466/pr0.1991.68.3c.1059. [DOI] [PubMed] [Google Scholar]
- Han K, Weed NC, Calhoun RF, Butcher JN. Psychometric characteristics of the MMPI-2 Cook-Medley hostility scale. Journal of Personality Assessment. 1995;65:567–585. doi: 10.1207/s15327752jpa6503_15. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes J, Hatsukami DK. Errors in using tobacco withdrawal scale. Tobacco Control. 1998;7:92–93. doi: 10.1136/tc.7.1.92a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Iribarren C, Sidney S, Bild DE, Liu K, Markovitz JH, Roseman JM, et al. Association of hostility with coronary artery calcification in young adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. JAMA. 2000;283:2546–2551. doi: 10.1001/jama.283.19.2546. [DOI] [PubMed] [Google Scholar]
- Jamner LD, Shapiro D, Jarvik ME. Nicotine reduces the frequency of anger reports in smokers and nonsmokers with high but not low hostility: an ambulatory study. Experimental and Clinical Psychopharmacology. 1999;7:454–463. doi: 10.1037//1064-1297.7.4.454. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Brown RA, Ramsey SE, Niaura R, Abrams DB, Goldstein MG, et al. Negative mood, depressive symptoms, and major depression after smoking cessation treatment in smokers with a history of major depressive disorder. Journal of Abnormal Psychology. 2002;111:670–675. doi: 10.1037//0021-843x.111.4.670. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Lachance HR, Strong DR, Ramsey SE, Monti PM, Brown RA. The commitment to quitting smoking scale: Initial validation in a smoking cessation trial for heavy social drinkers. Addictive Behaviors. 2007;32:2420–2424. doi: 10.1016/j.addbeh.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Metrik J, LaChance HR, Ramsey SE, Abrams DB, Monti PM, Brown RA. Addressing heavy drinking in smoking cessation treatment: A randomized clinical trial. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0012717. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Niaura R, Brown RA. Hostility in smokers with past major depressive disorder: Relation to smoking patterns, reasons for quitting, and cessation outcomes. Nicotine & Tobacco Research. 2004;6:809–818. doi: 10.1080/1462220042000282546. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Zvolensky MJ, Goldstein MG, Brown RA. Principles of Addiction Medicine. 3. Arlington, VA: American Society of Addiction Medicine; 2003. Behavioral interventions in nicotine dependence; pp. 891–904. [Google Scholar]
- Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Predicting relapse back to smoking: contrasting affective and physical models of dependence. Journal of Consulting and Clinical Psychology. 2002;70:216–227. [PubMed] [Google Scholar]
- Krueger RF. Phenotypic, genetic, and nonshared environmental parallels in the structure of personality: a view from the multidimensional personality questionnaire. Journal of Personality and Social Psychology. 2000;79:1057–1067. doi: 10.1037//0022-3514.79.6.1057. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Barefoot JC, Williams RB, Siegler IC. Personality measures as predictors of smoking initiation and cessation in the UNC Alumni Heart Study. Health Psychology. 1994;13:149–155. doi: 10.1037//0278-6133.13.2.149. [DOI] [PubMed] [Google Scholar]
- Llabre MM, Spitzer S, Siegel S, Saab PG, Schneiderman N. Applying latent growth curve modeling to the investigation of individual differences in cardiovascular recovery from stress. Psychosomatic Medicine. 2004;66:29–41. doi: 10.1097/01.psy.0000107886.51781.9c. [DOI] [PubMed] [Google Scholar]
- Lubin B, Van Whitlock R. Development of a measure that integrates positive and negative affect and personality: the Comprehensive Personality and Affect Scales. Journal of Clinical Psychology. 2002;58:1135–1156. doi: 10.1002/jclp.10042. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Determinants of relapse: Implications for the maintenance of behavior change. In: Davidson PO, Davidson SM, editors. Behavioral Medicine: Changing Health Lifestyles. New York: Brunner/Mazel; 1980. pp. 410–452. [Google Scholar]
- Miller SB, Friese M, Dolgoy L, Sita A, Lavoie K, Campbell T. Hostility, sodium consumption, and cardiovascular response to interpersonal stress. Psychosomatic Medicine. 1998;60:71–77. doi: 10.1097/00006842-199801000-00016. [DOI] [PubMed] [Google Scholar]
- Miller TQ, Smith TW, Turner CW, Guijarro ML, Hallet AJ. A meta-analytic review of research on hostility and physical health. Psychological Bulletin. 1996;119:322–348. doi: 10.1037/0033-2909.119.2.322. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. The physicians’ guide to helping patients with alcohol problems (Vol. NIH Publication No. 95-3769) National Institutes of Health; 1995. [Google Scholar]
- Niaura RS, Shadel W, Britt D, Abrams DB. Response to social stress, urge to smoke, and smoking cessation. Addictive Behaviors. 2002;27:241–250. doi: 10.1016/s0306-4603(00)00180-5. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Kenford SL, Smith SS, Fiore MC, Baker TB. Listening to nicotine: Negative affect and the smoking withdrawal conundrum. Psychological Science. 1997;8:184–189. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roberts BW, Caspi A, Moffitt TE. The kids are alright: growth and stability in personality development from adolescence to adulthood. Journal of Personality and Social Psychology. 2001;81:670–683. [PubMed] [Google Scholar]
- Shapiro D, Jamner LD, Goldstein IB. Daily mood states and ambulatory blood pressure. Psychophysiology. 1997;34:399–405. doi: 10.1111/j.1469-8986.1997.tb02383.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: A situational analysis. Journal of Consulting and Clinical Psychology. 1982;50:71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- Smith TW, Frohm KD. What’s so unhealthy about hostility? Construct validity and psychosocial correlates of the Cook and Medley Ho scale. Health Psychology. 1985;4:503–520. doi: 10.1037//0278-6133.4.6.503. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R - Non-patient edition (SCID-NP, Version 1.0) Washington, DC: American Psychiatric Press; 1990. [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Jorgensen RS. Assessing the MMPI-based Cook-Medley Hostility scale: the implications of dimensionality. Journal of Personality and Social Psychology. 1996;6:1281–1287. doi: 10.1037//0022-3514.70.6.1281. [DOI] [PubMed] [Google Scholar]
- Strong DR, Kahler CW, Greene RL, Schinka J. Isolating a primary dimension with the Cook Medley Hostility Scale: A Rasch analysis. Personality & Individual Difference. 2005;39:21–33. [Google Scholar]
- Suarez EC, Harlan E, Peoples MC, Williams RB., Jr Cardiovascular and emotional responses in women: the role of hostility and harassment. Health Psychology. 1993;12:459–468. doi: 10.1037//0278-6133.12.6.459. [DOI] [PubMed] [Google Scholar]
- Suarez EC, Kuhn CM, Schanberg SM, Williams RB, Jr, Zimmermann EA. Neuroendocrine, cardiovascular, and emotional responses of hostile men: the role of interpersonal challenge. Psychosomatic Medicine. 1998;60:78–88. doi: 10.1097/00006842-199801000-00017. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Brief manual for the Multidimensional Personality Questionnaire. University of Minnesota; Minneapolis: 1982. pp. 1031–1010. Unpublished manuscript. [Google Scholar]
- Tremblay PF, Ewart LA. The Buss and Perry Aggression Questionnaire and its relation to values, the Big five, provoking hypothetical situations, alcohol consumption patterns, and alcohol expectancies. Personality and Individual Differences. 2005;38:337–346. [Google Scholar]
- Vandervoort DJ, Pamela K, Hamilton SE. Some correlates of health locus of control among multicultural individuals. Current Psychology: Developmental, Learning, Personality, Social. 1997;16:167–178. [Google Scholar]
- West RJ, Hajek P, Belcher M. Severity of withdrawal symptoms as a predictor of outcome of an attempt to quit smoking. Psychological Medicine. 1989;19:981–985. doi: 10.1017/s0033291700005705. [DOI] [PubMed] [Google Scholar]


