Abstract
OBJECITIVE:
To determine the usefulness of positive and negative capsule endoscopies (CEs), and the impact of each on short- and long-term patient management.
METHODS:
Medical records were reviewed for 70 consecutive CE patients. Based on outcomes from referring physicians, it was determined whether CE was useful, partially useful or not useful at all in the overall patient management, and whether CE assisted in providing a diagnosis, and impacted on short-term long-term management.
RESULTS:
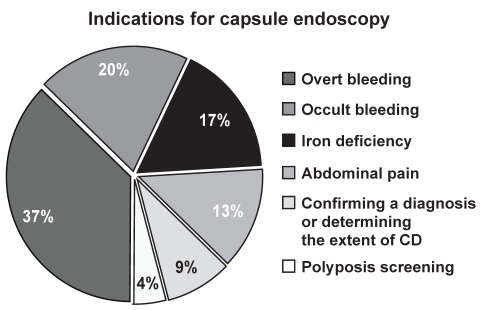
CE indications included overt bleeding (37%), occult bleeding (20%), iron deficiency (17%), abdominal pain and weight loss (13%), assessing the extent of or confirming a diagnosis of Crohn’s disease (9%) and screening for familial adenomatous polyposis (4%). Positive studies were seen in 58% of overt bleeds, 50% of occult bleeds, 33% of iron deficiencies and 33% of Crohn’s diseases. Overall, 28 studies (40%) were positive studies and 42 (60%) were negative studies. CE aided in diagnosis in 11 of 28 (39%) positive and 12 of 42 (29%) negative studies (P=0.35). Positive and negative CEs had an impact on short-term management in 12 of 28 (43%) versus 18 of 42 (43%) cases, respectively (P=1.0), and on long-term management in 14 of 28 (50%) versus 15 of 42 (36%) cases, respectively (P=0.23). For positive and negative studies, respectively, CE was considered useful in 12 of 28 (43%) versus 15 of 42 (36%) cases (39% overall), partially useful in 10 of 28 (36%) versus 10 of 42 (24%) cases (28% overall), and not useful at all in six of 28 (21%) versus 17 of 42 (40%) cases (33% overall).
CONCLUSIONs:
Although a negative CE may aid in making a definitive diagnosis in only 29% of patients, its effect on management and overall usefulness is similar to that of a positive CE. A physician’s decision on whether to order CE should not be based solely on the pretest probability of a positive examination but also on the clinical utility of a negative study.
Keywords: Capsule endoscopy, Crohn’s disease, Gastrointestinal bleeding
Abstract
OBJECTIF :
Déterminer l’utilité des endoscopies capsulaires (EC) positives et négatives et les répercussions de ces endoscopies sur la prise en charge à court et à long terme des patients.
MÉTHODOLOGIE :
On a examiné le dossier médical de 70 patients consécutifs ayant subi une EC. D’après les issues transmises par le médecin traitant, on a établi si l’EC avait été utile, partiellement utile ou inutile pour la prise en charge globale des patients et si l’EC avait contribué au diagnostic ou avait eu des répercussions sur la prise en charge à court ou à long terme.
RÉSULTATS :
Les indications d’EC incluaient un saignement extériorisé (37 %), un saignement occulte (20 %), une anémie ferriprive (17 %), des douleurs abdominales accompagnées d’une perte de poids (13 %), l’évaluation de l’étendue de la maladie de Crohn ou la confirmation du diagnostic (9 %) et le dépistage de la polypose adénomateuse familiale (4 %). On a obtenu des études positives dans 58 % des saignements extériorisés, 50 % des saignements occultes, 33 % des anémies ferriprives et 33 % des maladies de Crohn. Dans l’ensemble, 28 études (40 %) étaient positives et 42 (60%), négatives. L’EC a contribué au diagnostic de 11 (39 %) des 28 études positives et de 12 (29 %) des 42 études négatives (P=0,35). Les EC positives et négatives avaient des répercussions sur la prise en charge à court terme de 12 (43 %) des 28 cas par rapport à 18 (43 %) des 42 cas, respectivement (P=1,0) et sur la prise en charge à long terme de 14 (50 %) des 28 cas par rapport à 15 (36 %) des 42 cas, respectivement (P=0,23). Pour ce qui est des études positives et négatives, respectivement, l’EC a été considérée utile dans 12 (43 %) des 28 cas par rapport à 15 (36 %) des 42 cas (39 % dans l’ensemble), partiellement utile dans 10 (36 %) des 28 cas par rapport à 10 (24 %) des 42 cas (28 % dans l’ensemble) et inutile dans six (21 %) des 28 cas par rapport à 17 (40 %) des 42 cas (33 % dans l’ensemble).
CONCLUSION :
Même si une EC négative peut contribuer à poser un diagnostic définitif chez seulement 29 % des patients, son effet sur la prise en charge et l’utilité globale est similaire à celles de l’EC positive. La décision du médecin de demander une EC ne doit pas se fonder seulement sur la probabilité d’examen positif avant l’intervention mais également sur l’utilité clinique d’une étude négative.
Capsule endoscopy (CE) is an emerging technique for investigating the small bowel. It is currently indicated as part of the workup for obscure gastrointestinal (GI) bleeding (obscure-overt or obscure-occult), undiagnosed iron deficiency anemia, Crohn’s disease (CD), polyposis syndromes and cancer, celiac disease, for monitoring after small bowel transplant and, occasionally, for undiagnosed abdominal pain or diarrhea (1–11). Since its development, numerous studies (8,12–23) have compared the diagnostic yield of CE with other modalities commonly used to investigate the small bowel. Many such studies have shown CE to be more sensitive and more efficacious compared with either push enteroscopy (12,14–20) or small bowel follow-through (13,16,17). The sensitivity and specificity of CE have been cited to be as high as 89% and 95%, respectively (20). Although many studies have attempted to estimate the effectiveness of CE based on its diagnostic yield, few studies to date have considered the utility of a negative CE. In fact, some studies (24) have considered a negative CE to be a failure.
Currently, practitioners weigh the probability of a positive CE against the expense of the study. Thus, the pretest probability of having a positive study is heavily considered. Data exist on how positive CE leads to therapeutic measures, which, in turn, lead to positive clinical outcomes. However, data are lacking on the outcomes of patients with a negative CE. It is also somewhat more difficult to ascertain the value of a negative test. Previous studies have used objective measures such as whether a negative test leads to other tests or therapeutic interventions. A negative CE, although not confirming a specific diagnosis, may still be useful, because it allows the physician to cease a certain line of investigation, thereby impacting patient care. However, this is more difficult to quantify. There are also few published data regarding how often CE alters clinical management, something that has been poorly defined in previous studies. The objective of the present study was to determine how frequently a positive or negative CE assisted in making a diagnosis, how it affected clinical management and whether it was considered useful by the referring physician.
METHODS
A retrospective chart review was carried out on 70 consecutive patients who underwent CE at the Health Sciences Centre (Winnipeg, Manitoba) over a period of 30 months. The physicians who referred the patients for CE were surveyed. The patients’ family physicians were also contacted, when possible, for follow-up information. All CEs were read and interpreted by one physician (CNB). The CE studies were read and interpreted based on accepted nomenclature. The referring physicians were asked the following four questions for each patient: did CE assist in making a diagnosis? did CE change the short-term management? did CE change the long-term management? and, was CE useful, partially useful or not useful at all?
A change in management included the pursuit of a specific endoscopy or imaging study, surgery or medication. However, ceasing to pursue further investigations was also interpreted as a change in management. Moving beyond the consideration of a specific diagnosis (ie, confirming or finalizing a diagnosis of CD, or moving past this consideration) also qualified as a change in management. Outcomes were determined after a mean follow-up period of 7.3 months (range zero to 24 months). χ2 tests were used to compare proportions and a P value of less than 0.05 was considered to be statistically significant.
RESULTS
Of the 70 CE studies, 43 were performed on women and 27 were performed on men. The mean age of patients studied was 56.7 years old. The indications for the 70 CE studies are shown in Figure 1, and include overt bleeding (n=26, 37%), occult bleeding (n=14, 20%), iron deficiency anemia (n=12, 17%), abdominal pain and weight loss (n=9, 13%), to assess the extent of CD or confirm a diagnosis of the disease (n=6, 9%), and screening for polyposis syndromes or cancer (n=3, 4%). Of the 12 subjects with an indication of iron deficiency anemia, seven were women, and of these, three were menstruating (all were older than 40 years of age). None of these 12 subjects was a vegetarian or had obvious dietary reasons for low iron intake.
Figure 1).
Breakdown of 70 capsule endoscopy studies, based on indication. Overt bleeding was the most frequent indication for capsule endoscopy, followed by occult bleeding, iron deficiency, unexplained abdominal pain, confirming a diagnosis or determining the extent of Crohn’s disease (CD), and finally, screening for polyposis syndromes
Of the six CEs performed for CD, five were suspected cases, while one was diagnosed before CE. Of the 70 studies, 20 (29%) were incomplete (cecum not identified), with five never leaving the stomach. Of these five cases, three patients were on large doses of narcotics and one had known gastroparesis. Fifteen studies ended somewhere in the ileum: seven of those subjects were taking large amounts of narcotics (one was paraplegic), five were performed on hospitalized patients and two were diabetic. One other subject, with a history of abdominal radiation, had delayed small bowel retention of the capsule for over two years, until she presented with an acute small bowel obstruction at the site of capsule retention and died from postoperative complications.
Twenty-eight studies (40%) were positive and 42 studies (60%) were negative. The average age for positive studies was 62.4 years old, and for negative studies, the average age was 52.9 years old. The diagnostic yield of CE according to indication is shown in Table 1. Fifteen of 26 CEs (58%) performed for the indication of overt bleeding were positive, seven of 14 CEs (50%) performed for occult bleeding were positive, four of 12 CEs (33%) performed for iron deficiency were positive, and two of six CEs (33%) performed to assess the extent of CD or confirm the diagnosis of the disease were positive. In contrast, none of the CEs performed for the indication of abdominal pain and weight loss were positive (zero of nine), and none of the CE studies performed to screen for polyposis syndromes or cancer were positive (zero of three). Of the three menstruating women with an indication of iron deficiency anemia, all had negative studies. It is possible that their iron deficiency was secondary to their menstruation and that their CEs were truly negative.
TABLE 1.
Diagnostic yield of capsule endoscopy (CE) based on indication
| Indication |
Diagnostic yield of CE |
||
|---|---|---|---|
| Positive, n (%) | Negative, n (%) | Total, n | |
| Overt bleeding | 15 (58) | 11 (42) | 26 |
| Occult bleeding | 7 (50) | 7 (50) | 14 |
| Iron deficiency | 4 (33) | 8 (67) | 12 |
| Crohn’s disease | 2 (33) | 4 (67) | 6 |
| Polyposis screening | 0 (0) | 3 (100) | 3 |
| Abdominal pain | 0 (0) | 9 (100) | 9 |
The highest diagnostic yield was associated with the indication of overt bleeding, followed by occult bleeding, iron deficiency anemia and confirming a diagnosis of Crohn’s disease (or determining extent). Screening for polyposis syndromes and unexplained abdominal pain were both associated with a diagnostic yield of zero
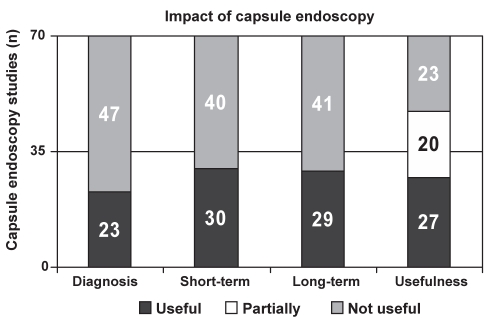
Overall, CE aided in the diagnosis of 23 of 70 patients (33%), impacted on short-term management in 30 of 70 patients (43%) and impacted on long-term management in 29 of 70 patients (41%). CE was found to be useful in 27 of 70 cases (39%), partially useful in 20 of 70 cases (28%) and not useful at all in 23 of 70 cases (33%) (Figure 2).
Figure 2).
Number of cases that capsule endoscopy aided in making a diagnosis, affected short-term management and affected long-term management. In addition, the utility of capsule endoscopy studies are shown, divided into categories of useful, partially useful or not useful at all
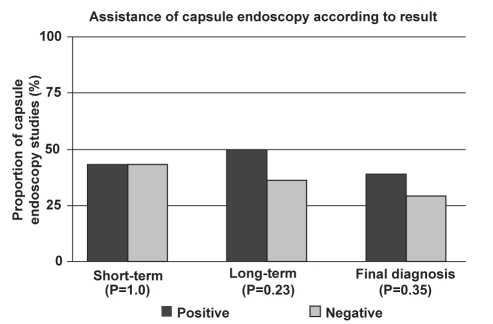
In the studies that were positive, CE aided in the diagnosis of 11 of 28 patients (39%), impacted on short-term management in 12 of 28 patients (43%) and impacted on long-term management in 14 of 28 patients (50%) (Figure 3). Positive studies were found to be useful in 12 of 28 cases (43%), partially useful in 10 of 28 cases (36%) and not useful at all in six of 28 cases (21%) (Figure 4).
Figure 3).
Proportion of capsule endoscopy (CE) studies that impacted on short-term management, long-term management and aided in a final diagnosis. Data are divided into two groups based on CE study result (positive versus negative). P values demonstrate no statistically significant difference based on these criteria
Figure 4).
Graphic demonstrating the utility of capsule endoscopy (CE) studies, divided into categories of useful, partially useful or not useful at all. Data are divided into two groups based on CE study result (positive versus negative). P values demonstrate no statistically significant difference based on these criteria
In the studies that were negative, CE aided in the diagnosis of 12 of 42 patients (29%), impacted on short-term management in 18 of 42 patients (43%) and impacted on long-term management in 15 of 42 patients (36%) (Figure 3). Negative studies were found to be useful in 15 of 42 cases (36%), partially useful in 10 of 42 cases (24%) and not useful at all in 17 of 42 cases (40%) (Figure 4).
DISCUSSION
The most common indications for CE in our patients were blood loss related (overt bleeding, occult bleeding and iron deficiency). Although this study was not intended to evaluate the indications for CE, these findings were consistent with previous literature (3,7,8, 14–21). Other common indications were to assess the extent of CD or confirm a diagnosis of the disease, indicators that are increasing in popularity (8–11,13,25).
The indication with the highest diagnostic yield was that of overt bleeding, followed by occult bleeding and iron deficiency. Also of note in our study is that the indication of abdominal pain and weight loss did not yield any positive studies. In spite of this, six of nine studies for that indication were thought to be either useful or partially useful by the referring physician. This is likely because a negative CE helped to rule out any serious pathology such as CD. Of the three studies that were performed to investigate for polyposis syndromes, none were positive. Not surprisingly, all three studies were deemed useful by the referring physician.
An incomplete CE was defined as failure to visualize the cecum. Of the 70 CEs performed, 20 (29%) were incomplete. This is more frequent than in some previously published reports. We suspect that the use of narcotics, as well as being hospitalized at the time of CE (hence, being sedentary), may place a patient at increased risk for delayed GI motility and, consequently, capsule retention.
Overall, CE aided in making a diagnosis in one-third of cases. There was no statistically significant difference in how frequently CE aided diagnosis in positive versus negative studies (39% and 29% respectively; P=0.35). There was also no statistically significant difference between how often CE impacted on short-term management (positive studies, 43%; negative studies, 43%; P=1.0) or long-term management (positive studies, 50%; negative studies, 36%; P=0.23).
The utility of CE was quite high in this study. Of all CEs performed, 67% were found to be either useful or partially useful (39% and 28%, respectively). There was no statistically significant difference between positive and negative CEs based on utility. Forty-three per cent of positive studies were deemed useful compared with 36% of negative CEs (P=0.55). Seventy-nine per cent of positive CEs were thought to be useful or partially useful (43% and 36%, respectively), compared with 60% (36% useful and 24% partially useful) of negative CEs (P=0.096).
Few studies have looked at how CE affects clinical management (21–23,25–27). van Tuyl et al (26) estimated that in cases of obscure GI bleeding, CE influenced clinical decisions in approximately 40% of patients. We found similar results with CE affecting short-term management and long-term management in 43% and 42% of patients, respectively. Rastogi et al (22) found that of 44 CE studies, 18 were positive, and a specific intervention or change in management, based on the CE findings, was implemented in 12 of 44 cases (28%). They also followed the patients for a mean of 6.7 months, and found that only seven patients (16%) had a clinically meaningful change in outcome. However, these two studies only considered whether further testing or treatment was performed, and did not take into consideration ceasing a certain line of investigation. In a study by Chong et al (25), of 47 subjects who had CE for upper GI bleeding, 18 (38%) had a change in management. This is also similar to our findings. None of the above studies offered a definition for ‘change in management’, and only one study surveyed the referring physician (25). Not surveying the referring physician allows room for bias, because it is the authors that make the decision instead of the physician. In our study, by surveying the referring physicians, there was a reduced chance for bias.
No published studies to date have assessed the utility of a negative CE study. Although a negative CE may aid in making a definitive diagnosis in only 29% of cases, we found its effect on management and overall usefulness to be similar to that of a positive CE. It is possible that if we assessed a greater number of CEs, we may find that there would be a greater usefulness of positive versus negative CE results. It is possible that a study with adequate power would show a difference in impact favouring positive studies. The lack of significant difference in outcomes between positive and negative studies does not prove that they are of similar value. However, we believe our findings support the utility of some negative studies. Therefore, in assessing CE, this possibility needs to be considered when weighing the cost-effectiveness of this investigative tool.
We have found value in a considerable number of negative CE results in the setting where CE was used as the last step in the workup of abdominal pain or for querying CD, and clinicians considered the CE useful, even if negative. The literature suggests that CE studies performed for the indication of chronic abdominal pain rarely yield a positive diagnosis (2,28). Bardan et al (2) looked at 20 such patients, and none had diagnostic lesions on CE. In a study by Tatar et al (28) of 200 CE cases, 41 were for the indication of abdominal pain. They found lesions that were diagnostic by CE in only 17%. Even our preliminary results suggest that an indication of abdominal pain rarely leads to a positive diagnosis; however, a negative result can lead to the end of a diagnostic trail.
Questions are arising as to where CE belongs temporally in the stepwise approach to obscure bleeding. The answer certainly hinges on the cost-effectiveness of the study and, specifically, the cost versus utility of CE as a diagnostic tool. CE is not therapeutic, so subsequent intervention or re-examination of a previously examined segment of the GI tract may be required. Detection rates are also analyzer dependent, because those with more experience with CEs interpret studies faster and may have higher detection rates. The utility of negative studies, however, for the indication of obscure bleeding requires long-term follow-up to ensure that the study was not falsely negative in regard to important small bowel lesions. The sensitivity of CE varies depending on indication. If intraoperative endoscopy is considered the gold standard, the sensitivity of CE for obscure-overt and obscure-occult GI bleeding is very high. However, the false-negative rate increases for nonbleeding indications. Also, the ability of CE to rule out a diagnosis depends on the pretest probability. In patients that have a low or intermediate pretest probability, especially for overt or occult GI bleeding, CE can be very useful in helping the clinician decide to cease pursuing a certain line of investigation. However, if the pretest probability is high, then a negative CE may be less useful, because the likelihood that it is falsely negative is increased. Recently, Jones et al (29) reported on repeat CE for obscure GI bleeding when the initial CE was negative or nondiagnostic. They demonstrated additional findings in 75% of repeat CEs. The indications for repeat CE were mainly recurrent GI bleeding and limited visualization.
CONCLUSIONS
A physician’s decision about whether to order CE should not be based solely on the pretest probability of a positive examination but also on the clinical utility of a negative study.
Acknowledgments
Dr Charles Bernstein is supported in part by a Crohn’s and Colitis Foundation of Canada Research Scientist Award.
REFERENCES
- 1.Kornbluth A, Legnani P, Lewis BS. Video capsule endoscopy in inflammatory bowel disease: Past, present, and future. Inflamm Bowel Dis. 2004;10:278–85. doi: 10.1097/00054725-200405000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Bardan E, Nadler M, Chowers Y, Fidder H, Bar-Meir S. Capsule endoscopy for the evaluation of patients with chronic abdominal pain. Endoscopy. 2003;35:688–9. doi: 10.1055/s-2003-41520. [DOI] [PubMed] [Google Scholar]
- 3.Schulmann K, Hollerbach S, Willert J, Kraus K, Schmiegel W. Detection of occult gastrointestinal bleeding disorders by video capsule endoscopy (M2A) of the small bowel. Gastroenterology. 2002;122:A329. (Abst) [Google Scholar]
- 4.Petroniene R, Dubcenco E, Baker JP, et al. Performance evaluation of the Given Diagnostic Imaging System in diagnosing celiac disease. Gastroenterology. 2002;122:A329. (Abst) [Google Scholar]
- 5.de Franchis R, Rondonotti E, Abbiati C, et al. Capsule enteroscopy in small bowel transplantation. Dig Liver Dis. 2003;35:728–31. doi: 10.1016/s1590-8658(03)00417-1. [DOI] [PubMed] [Google Scholar]
- 6.de Mascarenhas-Saraiva MN, da Silva Araujo Lopes LM. Small-bowel tumors diagnosed by wireless capsule endoscopy: Report of five cases. Endoscopy. 2003;35:865–8. doi: 10.1055/s-2003-42625. [DOI] [PubMed] [Google Scholar]
- 7.Delvaux M, Gay G. Capsule endoscopy in 2005: Facts and perspectives. Best Pract Res Clin Gastroenterol. 2006;20:23–39. doi: 10.1016/j.bpg.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Scapa E, Jacob H, Lewkowicz S, et al. Initial experience of wireless-capsule endoscopy for evaluating occult gastrointestinal bleeding and suspected small bowel pathology. Am J Gastroenterol. 2002;97:2776–9. doi: 10.1111/j.1572-0241.2002.07021.x. [DOI] [PubMed] [Google Scholar]
- 9.Voderholzer WA, Beinhoelzl J, Rogalla P, et al. Small bowel involvement in Crohn’s disease: A prospective comparison of wireless capsule endoscopy and computed tomography enteroclysis. Gut. 2005;54:369–73. doi: 10.1136/gut.2004.040055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fireman Z, Mahajna E, Broide E, et al. Diagnosing small bowel Crohn’s disease with wireless capsule endoscopy. Gut. 2003;52:390–2. doi: 10.1136/gut.52.3.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herrerias JM, Caunedo A, Rodriguez-Tellez M, Pellicer F, Herrerias JM. Capsule endoscopy in patients with suspected Crohn’s disease and negative endoscopy. Endoscopy. 2003;35:564–8. doi: 10.1055/s-2003-40241. [DOI] [PubMed] [Google Scholar]
- 12.Appleyard M, Fireman Z, Glukhovsky A, et al. A randomized trial comparing wireless capsule endoscopy with push enteroscopy for the detection of small-bowel lesions. Gastroenterology. 2000;119:1431–8. doi: 10.1053/gast.2000.20844. [DOI] [PubMed] [Google Scholar]
- 13.Costamagna G, Shah SK, Riccioni ME, et al. A prospective trial comparing small bowel radiographs and videocapsule endoscopy for suspected small bowel disease. Gastroenterology. 2002;123:999–1005. doi: 10.1053/gast.2002.35988. [DOI] [PubMed] [Google Scholar]
- 14.Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002;34:685–9. doi: 10.1055/s-2002-33446. [DOI] [PubMed] [Google Scholar]
- 15.Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: A comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut. 2003;52:1122–6. doi: 10.1136/gut.52.8.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marmo R, Rotondano G, Piscopo R, Bianco MA, Cipolletta L. Meta-analysis: Capsule enteroscopy vs. conventional modalities in diagnosis of small bowel diseases. Aliment Pharmacol Ther. 2005;22:595–604. doi: 10.1111/j.1365-2036.2005.02625.x. [DOI] [PubMed] [Google Scholar]
- 17.Triester SL, Leighton JA, Leontiadis GI, et al. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100:2407–18. doi: 10.1111/j.1572-0241.2005.00274.x. [DOI] [PubMed] [Google Scholar]
- 18.Mata A, Bordas JM, Feu F, et al. Wireless capsule endoscopy in patients with obscure gastrointestinal bleeding: A comparative study with push enteroscopy. Aliment Pharmacol Ther. 2004;20:189–94. doi: 10.1111/j.1365-2036.2004.02067.x. [DOI] [PubMed] [Google Scholar]
- 19.Adler DG, Knipschield M, Gostout C. A prospective comparison of capsule endoscopy and push enteroscopy in patients with GI bleeding of obscure origin. Gastrointest Endosc. 2004;59:492–8. doi: 10.1016/s0016-5107(03)02862-1. [DOI] [PubMed] [Google Scholar]
- 20.Saurin JC, Delvaux M, Gaudin JL, et al. Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: Blinded comparison with video push-enteroscopy. Endoscopy. 2003;35:576–84. doi: 10.1055/s-2003-40244. [DOI] [PubMed] [Google Scholar]
- 21.Pennazio M, Santucci R, Rondonotti E, et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: Report of 100 consecutive cases. Gastroenterology. 2004;126:643–53. doi: 10.1053/j.gastro.2003.11.057. [DOI] [PubMed] [Google Scholar]
- 22.Rastogi A, Schoen RE, Slivka A. Diagnostic yield and clinical outcomes of capsule endoscopy. Gastrointest Endosc. 2004;60:959–64. doi: 10.1016/s0016-5107(04)02226-6. [DOI] [PubMed] [Google Scholar]
- 23.Sturniolo GC, Di Leo V, Vettorato MG, D’Inca R. Clinical relevance of small-bowel findings detected by wireless capsule endoscopy. Scand J Gastroenterol. 2005;40:725–33. doi: 10.1080/00365520510015511. [DOI] [PubMed] [Google Scholar]
- 24.Swain P, Fritscher-Ravens A. Role of video endoscopy in managing small bowel disease. Gut. 2004;53:1866–75. doi: 10.1136/gut.2003.035576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chong AK, Taylor A, Miller A, Hennessy O, Connell W, Desmond P. Capsule endoscopy vs. push enteroscopy and enteroclysis in suspected small-bowel Crohn’s disease. Gastrointest Endosc. 2005;61:255–61. doi: 10.1016/s0016-5107(04)02571-4. [DOI] [PubMed] [Google Scholar]
- 26.van Tuyl SA, Stolk MF, Timmer R. Clinical application of video capsule endoscopy. Scand J Gastorenterol Suppl. 2003:24–8. doi: 10.1080/00855920310002654. [DOI] [PubMed] [Google Scholar]
- 27.Chong AK, Taylor AC, Miller AM, Desmond PV. Initial experience with capsule endoscopy at a major referral hospital. Med J Aust. 2003;178:537–40. doi: 10.5694/j.1326-5377.2003.tb05354.x. [DOI] [PubMed] [Google Scholar]
- 28.Tatar EL, Shen EH, Palance AL, Sun JH, Pitchumoni CS. Clinical utility of wireless endoscopy: Experience with 200 cases. J Clin Gastroenterol. 2006;40:140–4. doi: 10.1097/01.mcg.0000196185.11802.b2. [DOI] [PubMed] [Google Scholar]
- 29.Jones BH, Fleischer DE, Sharma VK, et al. Yield of repeat wireless video capsule endoscopy in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100:1058–64. doi: 10.1111/j.1572-0241.2005.40722.x. [DOI] [PubMed] [Google Scholar]