Abstract
Objective
To identify reasons for delay in management of patients with cauda equina syndrome (CES) and to determine commonly presented features of CES.
Methods
Retrospectively, the presenting features and management of patients treated for CES over a 4‐year period were reviewed.
Results
Reasons for delay in treatment were identified in over half of the patients.
Discussion
Most patients do not present with all the characteristic features of CES. Sacral sensory loss is a sensitive and relatively specific sign for diagnosing CES.
Patients with cauda equina syndrome (CES) characteristically present with a history of lower back pain, bilateral sciatica, motor and sensory disturbance including sacral and perianal anaesthesia, and sphincter disturbance. It may progress to permanent sensory loss, motor loss and incontinence.1,2,3 Emergent decompression of CES is important in improving the outcome. A meta‐analysis involving 322 patients from 104 studies showed that considerable improvements in sensory, motor and sphincter deficits were possible if surgery was performed within 48 h.4
Many patients presenting with CES do not receive an urgent referral to a specialist. Difficulties in diagnosis may arise because of the variability of the clinical features that are present on attendance to the emergency department, and also because of the association of urinary retention and constipation with pain and opioid analgesia.
The purpose of this study was to identify reasons for delay in management and to see which features of this syndrome patients present with.
Methods
Retrospectively, the case notes of patients transferred to St George's Hospital, London neurosurgical centre between 2001 and 2005 with a confirmed diagnosis of CES on magnetic resonance imaging were reviewed.
Results
In all, 32 patients with CES (53% men; mean age 46.8 years, range 20–80 years) presented to nine different emergency departments. Table 1 shows the proportion of patients presenting with particular symptoms and signs.
Table 1 Clinical features of patients presenting with cauda equina syndrome (n = 32).
| Lower back pain n = 32 | Sciatica n = 25 | Sensory loss | Motor loss n = 31 | Motor reflex loss | Sphincters | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Legs n = 30 | Sacral n = 27 | Perianal n = 24 | Knee n = 22 | Ankle n = 22 | Urinary symptoms n = 31 | Rectal symptoms n = 31 | Decreased anal tone n = 23 | ||||
| 94 | 44 (bi) | 30 (bi) | 85 | 75 | 32 (bi) | 9 (bi) | 46 (bi) | 84 | 35 | 78 | |
| 48 (uni) | 37 (uni) | 32 (uni) | 14 (uni) | 18 (uni) | |||||||
bi, bilateral symptoms or signs; uni, unilateral symptoms or signs.
All values are percentages.
In all, 6 (19%) patients presented with the symptom cluster of lower back pain, bilateral sciatica, motor loss, sacral sensory loss and sphincter disturbance.
On those patients operated on (n = 29), the mean length of time from presentation to operation was 31.3 h (range 6–76 h) and 90% of patients were operated on within 48 h. Three patients were not operated on, two of whom were deemed to have been referred too late for surgical intervention to be worthwhile and one patient who developed unrelated medical problems.
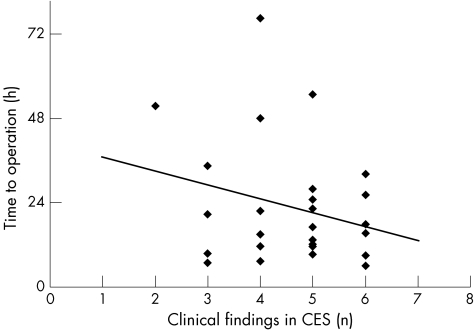
Figure 1 shows that there is some correlation between the time from presentation to operation and the number of clinical features of CES documented on presentation.
Figure 1 Number of clinical findings in patients with cauda equina syndrome (CES) versus time to operation. Clinical findings defined as lower back pain, sciatica, motor loss, sensory loss, reflex loss and sphincter disturbance.
Reasons for delay
Table 2 lists the clearly identifiable reasons for surgical treatment delay in about half of the patients.
Table 2 Reasons identified for delay in management of cauda equina syndrome.
| Patient‐related factors | |
| Presented too late | 1 |
| Complicating medical comorbidity | 2 |
| Physician‐related factors | |
| CES not considered | 4 |
| Referral to inappropriate specialty | 2 |
| Inappropriate initial management | 2 |
| Inappropriate advice from neurosurgical or orthopaedic team | 2 |
| Other factors | |
| No beds in the tertiary centre | 2 |
| Mechanical failure of MRI scanner | 1 |
CES, cauda equina syndrome; MRI, magnetic resonance imaging.
Discussion
Delays in the treatment of CES were most often due to delay in making the diagnosis. Predictably, this was more likely when fewer features of CES were established at the time of presentation.
Only 19% of patients presented with the characteristic combination of bilateral sciatica, lower limb weakness, saddle anaesthesia and sphincter disturbance. Table 1 shows that the strongest presenting features of CES are lower back pain, sacral sensory loss and urinary symptoms.
Conclusion
Patients may not clearly manifest all the characteristic features of CES. Diagnosis is also complicated by sphincter disturbance due to pain and opioid‐based analgesia. By highlighting the importance of examining for sacral sensory loss as a sensitive and relatively specific sign that is quick and easy to examine for, clinicians will be quicker in recognising it and thus improve outcomes in patients with CES.
Abbreviations
CES - cauda equina syndrome
Footnotes
Competing interests: None.
References
- 1.Jennett W B. A study of 25 cases of compression of the cauda equina by prolapsed intervertebral discs. J Neurol Neurosurg Psychiatry 195619109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malloch J D. Acute retention due to intervertebral disc prolapse. Br J Urol 196537578. [DOI] [PubMed] [Google Scholar]
- 3.Shapiro S. Cauda equina syndrome secondary to lumbar disc herniation. Neurosurgery 199332743–747. [DOI] [PubMed] [Google Scholar]
- 4.Ahn U M, Ahn N U, Buchowski J M.et al Cauda equina syndrome secondary to lumbar disc herniation. A meta‐analysis of surgical outcomes. Spine 2000251515–1522. [DOI] [PubMed] [Google Scholar]