Abstract
Background
Prehospital research has found little evidence in support of advanced cardiac life support (ACLS) for out‐of‐hospital cardiac arrest. However, these studies generally examine city‐based emergency medical services (EMS) systems. The training and experience of ACLS‐skilled paramedics differs internationally, and this may also contribute to negative findings. Additionally, the frequency of negative outcome in out‐of‐hospital cardiac arrest suggests that it is difficult to establish sufficient numbers to detect an effect.
Purpose
To examine the effect of ACLS on cardiac arrest in Queensland, Australia. Queensland has a population of 3.8 million and an area of over 1.7 million km2, and is served by a statewide EMS system, which deploys resources using a two‐tier model. Advanced treatments such as intubation and cardioactive drug administration are provided by extensively trained intensive care paramedics.
Methods
An observational, retrospective design was used to examine all cases of cardiac arrest attended by the Queensland Ambulance Service from January 2000 to December 2002. Logistic regression was used to examine the effect of the presence of an intensive care paramedic on survival to hospital discharge, adjusting for age, sex, initial rhythm, the presence of a witness and bystander cardiopulmonary resuscitation.
Results
The presence of an intensive care paramedic had a significant effect on survival (OR = 1.43, 95% CI = 1.02 to 1.99).
Conclusions
Highly trained ACLS‐skilled paramedics provide added survival benefit in EMS systems not optimised for early defibrillation. The reasons for this benefit are multifactorial, but may be the result of greater skill level and more informed use of the full range of prehospital interventions.
Early access to advanced cardiac life support (ACLS) is the final link in the “chain of survival” for out‐of‐hospital cardiac arrest (OHCA).1 ACLS generally includes interventions such as endotracheal intubation (ETI), intravenous cannulation and cardioactive drugs. As all levels of prehospital responders now commonly use defibrillation, it is more appropriate to consider it a basic life support (BLS) skill. There has been limited research support for improved outcomes from ACLS delivered for OHCA.
Previous studies have generally found no difference in survival to hospital discharge for patients treated by BLS paramedics versus ACLS‐skilled paramedics.2,3,4,5 However, a number of studies have demonstrated that ACLS‐skilled paramedics improve the likelihood of patients arriving at hospital with a spontaneous pulse.6,7,8 The largest and most recent study of the effect of ACLS‐skilled paramedics in the treatment of OHCA has been the third phase of the Ontario Prehospital Advanced Life Support study, which examined the incremental effect of ACLS in an emergency medical services (EMS) system with an optimised rapid defibrillation programme.9 The study demonstrated that survival rates for patients were not significantly affected by the introduction of an ACLS program. These findings, combined with the findings of previous studies, seem to add weight to the conclusion that there is no additional benefit of ACLS interventions in survival from OHCA, and that defibrillation remains the definitive treatment.
Studies examining the effect of the ACLS interventions themselves are equally pessimistic. Few studies demonstrate any positive effect on survival for ETI or adrenaline.10,11,12 It has been suggested that this may be because such treatments are generally used for patients who have not initially responded to defibrillation and who have a prolonged resuscitation, making them markers for a subset of patients with a poorer prognosis.13
However, some positive findings for ACLS have been reported. It has been found that two‐tier systems with both defibrillator‐equipped BLS and ACLS‐skilled paramedics report higher survival rates than those that operate one‐tier defibrillator‐equipped BLS systems alone,14,15,16 although the dispatch model also seems to moderate survival.17 Additionally, a positive effect on survival for time to ETI has been demonstrated, with patients who were intubated within 12 min having better outcomes than those intubated afterwards.18
Comparisons of outcomes from these studies are problematic. Interventions utilised and the extensiveness of training differ widely across EMS systems. ACLS training courses range from 10 to 75 weeks, and prerequisite experience or training is rarely specified. Secondly, studies have difficulty in disentangling the effect of greater skill and experience from the effect of the interventions themselves. Thirdly, there can be a systematic bias in two‐tier EMS systems, in which ACLS‐skilled paramedics are often called for the most severe cases and are therefore treating patients with poorer prognoses. Finally, only a small subset of the total treated population has a genuine prospect of successful resuscitation. As a result, improvements in patient outcome can be small and difficult to detect.
Although the Ontario Prehospital Advanced Life Support study examined the incremental effect of ACLS in an already optimised rapid‐defibrillation EMS system, many EMS systems do not meet this study's benchmark of defibrillating 90% of patients within 8 min. It is important to examine the effect of ACLS in systems that do not have an optimised rapid‐defibrillation programme, as in these cases ACLS may provide some incremental value. The purpose of the current study was to examine the effect of ACLS‐skilled paramedics on survival from OHCA in the context of a statewide EMS.
Methods
Design
The study was a retrospective, observational design and examined data from all patients who were treated for OHCA by the Queensland Ambulance Service (QAS) for the years 2000–2.
Data collection and management
Data were collected according to Utstein guidelines.19 Only those cases where resuscitation was attempted were included in the analyses. Patients <18 years of age and patients with a cardiac arrest of non‐cardiac aetiology were excluded from the study. Cardiac aetiology was presumed for men >40 and women >50 years of age when determination of aetiology was not possible from the available information.
For each case of cardiac arrest, ambulance records were uploaded from a centralised database and audited for accuracy against a hard copy of the ambulance report form. The ambulance report form collects information in both a code‐based and a narrative script format. In addition, a specific cardiac arrest form is completed to capture core Utstein variables. By comparing these sources of information, the auditing process is able to produce high levels of data accuracy and completeness, allowing for correction of coding errors and capture of missing information. Although there is some variation in the data provided on these capture forms, they typically give a detailed account of the incident. Where multiple crews attend the same patient, case details are recorded on one form.
Paramedics use a time stamp on the dispatch system to record times, which are later recorded manually on the ambulance report form. Therefore, information regarding time intervals is synchronised throughout the service and is generally accurate and reliable.
Ambulance records were linked to hospital records, using probabilistic matching, to ascertain survival to discharge information.
Data collection and analyses were performed as part of routine ambulance monitoring and quality assurance procedures. Therefore, ethical approval was not required. Ethical approval was obtained for linkage of ambulance data with hospital data to determine survival outcomes.
Population and setting
The setting for the current study was the state of Queensland, the second largest state in Australia. Queensland has a population of approximately 3.84 million people, covers an area of 1 734 513 km2, and is geographically diverse.20 Most of the population is scattered along the eastern seaboard; however, over half the state's population resides in the capital city. There are 13 cities across the state with populations in excess of 50 000.
EMS system
The QAS is a statewide service. For the purpose of the current study, paramedic skill level was dichotomised with intensive care paramedics (ICPs) classified as ACLS‐skilled paramedics and all other levels classified as non‐ACLS‐skilled paramedics (or non‐ICPs). ICPs may deliver the full range of OHCA pre‐hospital interventions including ETI and a range of cardioactive drugs. Other skill levels may provide CPR, defibrillation and basic airway care including oropharyngeal and laryngeal mask airways. All QAS crews are equipped with defibrillators and trained in their use. For the purposes of this research, the skill level required for each case was that of an officer with the highest skill level on scene.
In Queensland, paramedics must have 2 years of field experience after their initial 3 years of paramedic training to be eligible to apply for ICP training. The ICP course is a one‐year, full‐time course that combines university‐based classroom education, placement in hospital emergency departments and operating theatres, and extensive field experience. During their training, intensive care students also work alongside an ICP mentor in real patient care settings. The programme not only engages paramedics in psychomotor skill rehearsal of advanced clinical interventions but also heavily emphasises the use of clinical judgement and reflection in the use of these interventions.
ICPs and non‐ICPs operate within a two‐tier EMS system in Queensland. In some urban areas, this means ICPs are floating and are often second to the scene of an arrest. Current dispatch protocols automatically deploy an ICP to a suspected arrest if one is available. No allowance is made for the likely prognosis of the patient, as this cannot be accurately predicted by the dispatcher. ICPs are assigned to ambulance stations according to regional directives, and, therefore, there is an uneven dispersion of ACLS providers across the state. Consequently, the two‐tier system might be optimised in certain areas, and in other areas with less ACLS providers the two tiers may operate more as a one‐tier system, with ACLS providers called to attend the nearest incident regardless of its severity.
Data analyses
Preliminary analyses examined the relationship between the key explanatory and outcome variables, and demographic and prehospital factors, using χ2 analyses. Arrests witnessed by paramedics were excluded from the analyses as they were seen to constitute a distinct group of patients who have a much better prognosis and are more likely to respond to BLS. The primary analysis examined the relationship between skill level (ICP v non‐ICP) and survival to hospital discharge, using logistic regression.
Results
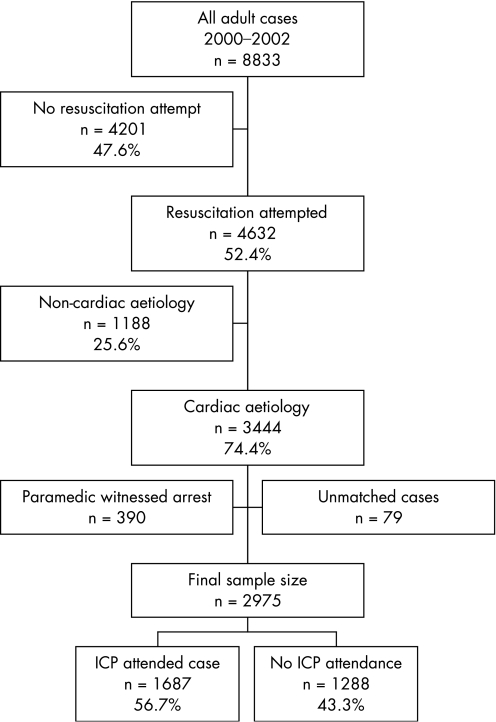
Over the 3 years of the study period, a total of 8833 adult patients received treatment by QAS for an OHCA. Of these, 3054 patients met the inclusion criteria for this study (resuscitation attempted by paramedics, arrest of presumed cardiac aetiology, arrest not witnessed by paramedic). Matching with hospital data was unsuccessful in 79 (2.6%) cases, leaving a total sample size of 2975. ICPs attended 1687 (56.7%) of these cases; 1288 (43.3%) patients were treated without ICP attendance. Figure 1 presents these data.
Figure 1 Utstein template of all study cases in 2000–2.
χ2 analyses compared patients treated by ICPs with those treated by non‐ICPs in terms of age, sex, initial rhythm, witnessed arrest and bystander CPR. Table 1 shows these results.
Table 1 χ2 results of demographic and prehospital factors of those treated by intensive care paramedics and non‐intensive care paramedics.
| Characteristic | ICPs | Non‐ICPs | p value |
|---|---|---|---|
| n | 1687 | 1288 | – |
| Mean (SD) age, years | 68.3 (13.5) | 69.1 (13.4) | 0.10 |
| Male sex | 1195 (70.9) | 909 (70.6) | 0.85 |
| Witnessed arrest | 1080 (65.6) | 792 (63.1) | 0.16 |
| Shockable rhythm | 786 (46.7) | 580 (45.2) | 0.41 |
| Bystander CPR | 952 (56.6) | 646 (50.3) | 0.001 |
ICPs, intensive care paramedics; non‐ICPs, non‐intensive care paramedics.
Values given in parenthesis are %, unless otherwise specified.
Table 2 presents results of χ2 analyses comparing survival between patients treated by non‐ICPs and those treated by ICPs.
Table 2 χ2 results examining the relationship between intensive care paramedics and non‐intensive care paramedics and survival.
| Survival factors | ICPs | Non‐ICPs | p value |
|---|---|---|---|
| n | 1687 | 1288 | – |
| Pulse at hospital arrival | 355 (21.2) | 109 (8.5) | 0.001 |
| Survival to hospital discharge | 113 (6.70) | 60 (4.66) | 0.03 |
| Died | 1574 (93.3) | 1228 (95.3) | 0.01 |
ICPs, intensive care paramedics; non‐ICPs, non‐intensive care paramedics.
Values given in parenthesis are %, unless otherwise specified.
Transportation and admission to hospital
The rates of transportation and admission to hospital for the two groups were compared using χ2 analyses (table 3).
Table 3 χ2 analyses examining rates of transport and hospital admission for intensive care paramedics and non‐intensive care paramedics.
| ICPs | Non‐ICPs | p value | |
|---|---|---|---|
| n | 1687 | 1288 | – |
| Transported to hospital | 566 (33.5) | 656 (50.9) | 0.001 |
| Admitted to hospital | 411 (24.4) | 336 (26.1) | 0.28 |
ICPs, intensive care paramedics; non‐ICPs, non‐intensive care paramedics.
Values given in parenthesis are %, unless otherwise specified.
Skill level and survival
In the main analysis, binary logistic regression analysis was used to model the probability of survival to hospital discharge in patients attended by ICPs compared with those not attended by ICPs (referent group) after adjusting for age, sex, initial rhythm, presence of a witness and bystander CPR. Secondary analyses included only those transported to hospital to exclude those patients with a very poor prognosis, and from among patients admitted to hospital. Table 4 shows the odds ratios and 95% confidence interval for skill level adjusted for sex, age, initial rhythm, presence of a witness and bystander CPR for these three analyses. In all models, the contribution of skill level was significant (p<0.05) when assessed using the likelihood ratio χ2 test.
Table 4 Logistic regression analyses examining the effect of skill level on survival to hospital discharge.
| OR | 95% CI | |
|---|---|---|
| All patients | 1.43 | 1.02 to 1.99 |
| Transported patients only | 2.33 | 1.64 to 3.31 |
| Admitted patients only | 1.62 | 1.12 to 2.36 |
Presence of ICP and time intervals
Response time was defined as the time from receiving the call to arrival at scene. On‐scene time was defined as the interval between arrival at patient and departure from scene. Time to defibrillation was calculated from the time of receiving the call to the time of first shock by paramedics. This analysis was conducted only on those cases that presented with an initial shockable rhythm (ventricular fibrillation or ventricular tachycardia). Time to shock interval could not be calculated in 152 (11.1%) cases because of missing data on time of first shock. It has been reported that defibrillation outcomes are optimised if the first shock is delivered within 4–6 min of arrest.21,22 Therefore, an additional between‐group analysis was conducted to compare the number of patients shocked within 5 min. Table 5 provides the results of these analyses.
Table 5 Key time intervals for intensive care paramedics and non‐intensive care paramedics.
| Time interval | ICPs | Non‐ICPs | p value |
|---|---|---|---|
| Mean (SD) response time, min | 8.40 (5.0) | 8.89 (11.9) | 0.125 |
| Mean (SD) on‐scene time | 31.46 (18.6) | 22.38 (20.4) | 0.001 |
| Mean (SD) time to first shock, min | 9.44 (4.7) | 10.07 (5.9) | 0.039 |
| Number of patients shocked within 5 min(%) | 92 (13.6%) | 94 (17.4%) | 0.067 |
ICPs, intensive care paramedics; non‐ICPs, non‐intensive care paramedics.
Discussion
The finding that the ACLS‐skilled paramedics significantly improve a patient's likelihood of survival in a statewide EMS system is noteworthy. To the authors' knowledge, this is one of the few studies to find a significant positive effect for advanced skill level on survival to hospital discharge. The effect increases markedly when examining only those transported to hospital. This, along with lower rates of transport for ICPs, suggests that ICPs are better able to select those patients for whom resuscitation is viable. As ICPs are able to provide a comprehensive range of ACLS interventions on scene, they can elect not to transport patients unresponsive to these treatments. Cases not attended by ICPs do not have the benefit of this knowledge, and so must decide on the appropriateness of transport based on case history and response to defibrillation and other BLS measures. As such they transport more patients, including some with a poor prospect of recovery. The patients in the admitted patient subgroup are assessed independently by hospital staff and may be thought of as having equivalent viability. Even in this cohort, patients treated by an ICP show an enhanced survival effect. This suggests that the survival effect seen cannot be attributed to differing resuscitation protocols.
This study made no attempt to disentangle the effect of advanced skill level and ACLS interventions. Previous research has failed to demonstrate an increase in survival associated with prehospital endotracheal intubation or adrenaline.10,23 This suggests that the improvement in survival seen here is not due to the advanced procedures used. Greater levels of education and training received by ICPs in Queensland may enable them to deliver both BLS and ACLS interventions more effectively. A study of intubation in an American EMS system found that tubes were incorrectly placed as much as 25% of the time.24 It seems plausible that an increased level of training would reduce the occurrence of such errors and improve ACLS delivery.
Alternatively, when ICPs and a BLS crew attend the same case, the full range of interventions could be performed with greater efficiency and effectiveness owing to the number of trained personnel on scene. The detrimental effects of interruptions to chest compressions on coronary perfusion pressure are well known.25 In cases where more paramedics attend the patient, it is likely that the frequency and duration of interruptions to chest compressions will be reduced.
The finding that cases attended by ICPs had longer on‐scene time was expected, and is probably due to either the primary crew delaying transport while awaiting ICP back‐up or the time required to perform ACLS procedures. The results presented here show that those patients who had longer scene times had a better outcome. This suggests that when highly skilled paramedics are available, full resuscitation at the scene may be preferable to rapid transport, as delay to ACLS is minimised. However, if the patient does not respond to treatment at the scene, rapid transport is unlikely to improve the outcome. This argument is supported when we consider that although a substantial number of patients among the non‐IC group arrive at hospital pulseless and go on to be admitted, few of these patients survive to hospital discharge. These patients may have been admitted after initially responding well to ACLS procedures performed in the hospital emergency department, but the low survival to discharge rate suggests that this effect is transitory. This finding provides support for ACLS as a critical component of enhanced survival, most effective when it is delivered early.
An unexpected finding was that cases attended by ICP crews had a significantly reduced time to first shock. As response times between the groups did not differ significantly, it seems that the reduced time to shock is a function of paramedic behaviour after arrival on scene. This time difference is unlikely to result of faster rhythm recognition or defibrillator activation by ICPs, as non‐ICP crews will often deliver the initial shock before the arrival of the ICP crew. Although the difference in defibrillation interval is statistically significant, it seems unlikely that the size of the difference would have a noticeable effect on patient outcome. An interval of around 5 min to defibrillation has been suggested as a critical period.21,22 Cases attended by ICP crews were not significantly more likely to deliver shocks within this 5‐min interval. Therefore, it is unlikely that the differences in time to first shock would account for the difference in survival observed.
The finding that bystander CPR was significantly associated with the presence of an ICP is interesting, and cannot be explained by clinical protocols or dispatch methods. Had no bystander CPR been performed, the BLS crew may have ceased resuscitation sooner and the ICP crew may not have been dispatched. However, when the presence of bystander CPR was controlled for, the presence of an ICP still significantly increased the likelihood of patient survival. Consequently, bystander CPR alone cannot account for the improvement in survival observed in this study.
The purpose of this paper was to examine the effect of ACLS‐skilled paramedics in the context of a statewide EMS system. The finding that ACLS‐skilled paramedics have a positive effect on survival suggests that advanced training in areas where defibrillation cannot be delivered within optimal time frames is critical to improving survival rates. The more extensive training and education of ACLS‐skilled paramedics not only allows effective ACLS intervention but may also optimise the effectiveness of BLS interventions.
Due to the observational and retrospective nature of this study, we cannot draw firm conclusions about what produced the increase in survival for those patients attended by ICPs. We are unable to determine what specific effect ACLS treatments had on patient outcome. Nor can we separate the effect of the intervention from the skill level of the paramedic providing it. Therefore, the survival effect seen may be due to a function of paramedic skill, the treatments provided or another uncontrolled factor. A number of alternative explanations could be proposed for our findings. ICPs tend to be deployed in areas of higher population. Although the results seen here might be influenced by a function of population density, the intuitive markers for such an effect, rates of witnessed arrest and response time did not differ significantly between the groups.
The survival effect probably cannot be explained by differing resuscitation protocols related to skill level. Both study groups are bound by the same criteria for the commencement of resuscitation. ICPs do have more scope to discontinue resuscitation at the scene, and this is reflected in the lower transport rates for this group. More experienced paramedics are probably more skilled at recognising cases of obvious death, and so when an ICP is first on scene, he or she may be less likely to begin resuscitation. It is not clear whether such an effect would have influenced the results here, as frequently ICPs arrive on scene after the primary crew has begun resuscitation. Finally, this study did not control for post‐resuscitation or in‐hospital care, both of which may have affected the outcome.
Further research is required to disentangle the effects of ACLS from the effects of advanced training alone. The impact or added benefit of ACLS in EMS systems that are decentralised or geographically dispersed, and where optimal defibrillation time frames cannot be met, warrants continued attention.
Abbreviations
ACLS - advanced cardiac life support
BLS - basic life support
EMS - emergency medical services
ETI - endotracheal intubation
ICPs - intensive care paramedics
OHCA - out‐of‐hospital cardiac arrest
QAS - Queensland Ambulance Service
Footnotes
Competing interests: None.
References
- 1.Cummins R O, Ornato J P, Thies W H.et al Improving survival from sudden cardiac arrest: the “chain of survival” concept: a statement for health professionals from the advanced cardiac life support subcommittee and the emergency cardiac care committee, American Heart Association. Circulation 1991831832–1847. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen‐Van‐Tam J S, Dove A F, Bradley M P.et al Effectiveness of ambulance paramedics versus ambulance technicians in managing out of hospital cardiac arrest. J Accid Emerg Med 199714142–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guly U M, Mitchell R G, Cooket al Paramedics and technicians are equally successful at managing cardiac arrest outside of hospital. BMJ 19953101091–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell R G, Guly U M, Raineret al Can the full range of paramedic skills improve survival from out of hospital cardiac arrests? J Accid Emerg Med 199714274–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rainer T H, Marshall R, Cusack S. Paramedics, technicians, and survival from out of hospital cardiac arrest. J Accid Emerg Med 199714278–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mann C J, Guly H. Paramedic interventions increase the rate of return of spontaneous circulation in out of hospital cardiac arrests. J Accid Emerg Med 199714149–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soo L H, Gray D, Younget al Influence of ambulance crew's length of experience on the outcome of out‐of‐hospital cardiac arrest. Eur Heart J 199920535–540. [DOI] [PubMed] [Google Scholar]
- 8.Kriegsman W E, Mace S E. The impact of paramedics on out‐of‐hospital cardiac arrests in a rural community. Prehosp Emerg Care 19982274–279. [DOI] [PubMed] [Google Scholar]
- 9.Stiell I G, Wells G A, Field B.et al Ontario prehospital advanced life support study group. Advanced cardiac life support in out‐of‐hospital cardiac arrest. N Engl J Med 2004351647–656. [DOI] [PubMed] [Google Scholar]
- 10.Bur A, Kittler H, Sterz F.et al Effects of bystander first aid, defibrillation and advanced life support on neurologic outcome and hospital costs in patients after ventricular fibrillation cardiac arrest. Intensive Care Med 2001271474–1480. [DOI] [PubMed] [Google Scholar]
- 11.Maheshwari A, Mehrotra A, Gupta A K.et al Prehospital ACLS—Does it work? Emerg Med Clin North Am 200220759–770. [DOI] [PubMed] [Google Scholar]
- 12.Wang H E, Kupas D F, Paris P M.et al Preliminary experience with a prospective, multi‐centered evaluation of out‐of‐hospital endotracheal intubation. Resuscitation 20035849–58. [DOI] [PubMed] [Google Scholar]
- 13.Adams J N, Sirel J, Marsden K.et al Heartstart Scotland: the use of paramedic skills in out of hospital resuscitation. Heart 199778399–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nichol G, Stiell I G, Laupacis A.et al A cumulative meta‐analysis of the effectiveness of defibrillator‐capable emergency medical services for victims of out‐of‐hospital cardiac arrest. Ann Emerg Med 199934517–525. [PubMed] [Google Scholar]
- 15.Persse D E, Key C B, Bradley R N.et al Cardiac arrest survival as a function of ambulance deployment strategy in a large urban medical services system. Resuscitation 20035997–104. [DOI] [PubMed] [Google Scholar]
- 16.Nichol G, Detsky A S, Stiell I G.et al Effectiveness of emergency medical services for victims of out‐of‐hospital cardiac arrest: a meta‐analysis. Ann Emerg Med 199627700–710. [DOI] [PubMed] [Google Scholar]
- 17.Pepe P E, Abramson N S, Brown C G. ACLS—Does it really work? Ann Emerg Med 1994231037–1041. [DOI] [PubMed] [Google Scholar]
- 18.Shy B D, Rea T D, Becker L J.et al Time to intubation and survival in prehospital cardiac arrest. Prehosp Emerg Care 20048394–399. [DOI] [PubMed] [Google Scholar]
- 19.Cummins R O, Chamberlain D A, Abramson N S.et al Recommended guidelines for uniform reporting of data from out‐of‐hospital cardiac arrest: the Utstein style. Ann Emerg Med 199120861–874. [PubMed] [Google Scholar]
- 20.Australian Bureau of Statistics National regional profile‐ Queensland. Cat no. 1379.0.55. 001 Australian Government in Canberra, Australia 2003
- 21.Cone D C. The eight‐minute defibrillation response interval debunked: or is it? Ann Emerg Med 200342251–255. [DOI] [PubMed] [Google Scholar]
- 22.Weisfeldt M L, Becker L B. Resuscitation after cardiac arrest: a 3‐phase time‐sensitive model. JAMA 20022883035–3038. [DOI] [PubMed] [Google Scholar]
- 23.Nolan J P, de Latorre F J, Steen P A.et al Advanced life support drugs: do they really work? Curr Opin Crit Care 20028212–218. [DOI] [PubMed] [Google Scholar]
- 24.Katz S H, Falk J L. Misplaced endotracheal tubes by paramedics in an urban medical services system. Ann Emerg Med 20013732–37. [DOI] [PubMed] [Google Scholar]
- 25.Kern K B, Hilwig R W, Berg R A.et al Importance of continuous chest compressions during cardiopulmonary resuscitation. Circulation 2002105645–649. [DOI] [PubMed] [Google Scholar]