Abstract
Objective
To use observational methods to objectively evaluate the organisation of triage and what issues may affect the effectiveness of the process.
Design
A two‐phase study comprising observation of 16 h of triage in a London hospital emergency department and interviews with the triage staff to build a qualitative task analysis and study protocol for phase 2; observation and timing in triage for 1870 min including 257 patients and for 16 different members of the triage staff.
Results
No significant difference was found between grades of staff for the average triage time or the fraction of time absent from triage. In all, 67% of the time spent absent from triage was due to escorting patients into the department. The average time a patient waited in the reception before triage was 13 min 34 s; the average length of time to triage for a patient was 4 min 17 s. A significant increase in triage time was found when patients were triaged to a specialty, expected by a specialty, or were actively “seen and treated” in triage. Protocols to prioritise patients with potentially serious conditions to the front of the queue had a significantly positive effect on their waiting time. Supplementary tasks and distractions had varying effects on the timely assessment and triage of patients.
Conclusions
The human factors method is applicable to the triage process and can identify key factors that affect the throughput at triage. Referring a patient to a specialty at triage affects significantly the triage workload; hence, alternative methods or management should be suggested. The decision to offer active treatment at triage increases the time taken, and should be based on clinical criteria and the workload determined by staffing levels. The proportion of time absent from triage could be markedly improved by support from porters or other non‐qualified staff, as well as by proceduralised handovers from triage to the main clinical area. Triage productivity could be improved by all staff by becoming aware of the effect of the number of interruptions on the throughput of patients.
In 2001, the Department of Health published the paper Reforming emergency care1 and introduced a compulsory national target for England. The target required that emergency departments work for a maximum time of 4 h in the emergency department for 98% of patients by April 2004. This time limit produced significant changes in the way many departments and hospitals dealt with their workload in the emergency department, and included many initiatives to reduce the total time and redirect patients with low acuity to alternative healthcare providers. One of the most noteworthy changes was the review of the process of “triage” and the change of the primary objective of triage—to allocate the patient to the most appropriate practitioner or area within the healthcare system, thus producing different streams or queues of patients waiting for dedicated teams of workers. Therefore, patients are explicitly triaged to the minors or majors area, and to see an emergency department doctor, emergency nurse practitioner or specialty doctor in one of those areas. Like the idea of “streaming” borrowed from manufacturing and industrial processes, the process of “triage” has been intended to manage risk in emergency care by evaluating the clinical condition of the incoming ambulatory patients and prioritising them to be seen according to their clinical need. This depends on the working diagnosis made by the assessing nurse and the perceived immediate needs of the patient, and had the effect of allocating some patients to the lowest priority category, effectively saying they could wait until all other patients had been seen. This category would clearly have an effect on the 4‐h target, and thus the triage process has been adjusted with less emphasis on prioritisation and more emphasis on “front loading” the patients' pathway. Thus, the essential investigations may be ordered from triage, or the relevant specialties are immediately informed of the arrival of their expected patient, thus minimising the “fallow” time waiting in the department for key points of the pathway to occur.
As a result of streaming and reforming emergency care, some patients are now given definitive simple treatment in the triage area and/or are given advice regarding self‐care or an alternative more appropriate healthcare provider. In this emergency department, this process is referred to as “see and treat”, which differs from the traditional interpretation of this term—wherein patients who present with minor injuries or illnesses are not triaged formally but are simply taken in time order by the practitioners working in the “minors” area of the department and seen, assessed and discharged by the one practitioner.2
Thus, the process locally defined as “see and treat” accounts for around 6% of the patients who present to the emergency department studied. Full evaluation of the patient's condition and the decision to discharge from triage without a more complex assessment, or after administration of simple treatment, could be expected to affect the flow through the triage process as it would in itself take longer. In the study department, triage is undertaken by nurses working at E grade (at least 1 year of emergency medicine experience) or above, and who have received targeted training and mentoring. See and treat is not taught as a separate skill; nurses who undertake triage are expected to redirect patients and give advice within their own scope of practice. Nurses are not currently allowed to give take home prescriptions, but can give single‐dose simple analgesia under patient group directives. Tetanus prescriptions are to be given by a medical practitioner.
Traditional targets for the emergency department included the promise to patients laid out in “Your Guide to the NHS”3 that on arrival in an emergency department “you should be assessed by a nurse or doctor, depending on how urgent your case is, within 15 min of your arrival…”. Although these data are no longer collected centrally, it remains an aspiration of the study department on the basis that it should reduce the risk of seriously ill patients remaining unidentified in the waiting room for extended periods.
The requirements of the triage task itself impose a degree of time pressure on the triage staff. They must spend adequate time collecting information from the current patient to make the best possible triage decision, but also not delay those waiting in reception who are, as yet, of unknown criticality.
A number of studies have examined the time required for triage, the factors affecting the time taken and the effects on the overall care process. In the US, Paulson4 carried out a retrospective review study of the effect of nurse qualification level on triage waiting time. In this, the average time to triage (defined as the time from sign‐in to the start of triage) was 17 min for a licensed nurse (data from 1998) and 15 min for unlicensed assisting personnel. The time from triage to treatment was considerably reduced (from 127 to 54 min) when the more qualified nurses were assigned for triage. Thus, the minimal time saved in the wait for triage by using less‐skilled staff greatly reduces the productivity of the overall care process. Lindley‐Jones and Finlayson5,6 showed that when x rays were ordered by triage staff, walking‐wounded patients had their treatment completed quicker without compromising service quality. The extension of triage nurse responsibilities from “test ordering” to “see and treat” offers further potential for greater efficiency7 in the overall pathway. However, there is potentially a risk of an influx of patients who are more suitable for primary care but who are attracted by the short waiting times and efficient service, causing stress and overwork for the staff.8
Using a systems approach to examine the triage process provides an objective non‐judgemental evaluation of the triage process. This systems approach requires the involvement of the people who carry out the work on a daily basis to define the current tasks and associated issues and identify feasible solutions to their own problems as opposed to solutions imposed by senior management.
This study seeks to use human factors methods to objectively evaluate the tasks within the process of triage, identify factors that have an influence on the effectiveness of the process with regard to the total time, defined by (1) time to triage an individual patient and (2) waiting time for triage. It does not seek to quantify the contribution of effective triage to the overall time in the department, nor to quantify the accuracy or effectiveness of triage by any other measure. This further aims to identify whether these methods are feasible and useful in the healthcare context.
Methods
A two‐phase study was carried out in a London emergency department in 2004. The study department sees 70 000 adult patients per year, of whom approximately 35% are brought by ambulance and the remaining arrive by public or private transport and present to the reception/triage area. Children's attendances are seen within a separate children's department from 08:00 to 20:00 h, and thus are excluded from this study.
The patient reception and registration desk is based in the main waiting room, beside the single triage room. The minors area of the department where mainly ambulant patients with simple injuries or minor illness are seen is located adjacent to the reception area and is easily accessible directly from the waiting area. The majors and resuscitation areas where the more seriously ill patients or patients with significant injuries are seen can be accessed only by a walk of approximately 35 m. There is no direct visual connection between the majors/resuscitation areas and the triage/reception area although there is a telephone extension in the triage room. The triage room is not equipped with a washbasin or drug cupboard, and supply of dressings is minimal. The triage room has an electrocardiogram and other equipment for monitoring vital signs. All x rays and blood tests are ordered via the departmental computerised patient record, and emergency team assistants are available to take blood when requested. The usual wait for a blood test once ordered is around 40 min, and that for x rays around 30 min. All patients who present to the reception desk are triaged in the main triage room, patients brought by ambulance undergo an initial assessment by the nurse in the majors/resuscitation room and a small proportion of these are redirected for further assessment to the main triage, the rest remaining in the majors/resuscitation area for further assessment. The layout of the department is shown in Appendix A (http://available at emj bmj.com/supplemental).
Triage notes are recorded on the computerised system, and the computer records the time the triage screen is closed at the time of triage—this may be some minutes after the start of triage if the triage itself takes a considerable period of time. The department runs a policy that if the waiting time for triage exceeds 15 min, a second triage desk be opened within the reception area.
Phase 1 incorporated the development of a task analysis of the triage process and an observation protocol. Phase 2 involved applying the observation protocol to the triage task to clarify and document the issues affecting the flow of the triage process. Data were collected according to the protocol constructed and analysed to determine the major influences on the time waiting for triage, time for the triage process and factors relating to these time periods.
Phase 1: a human factors researcher (ML) carried out 12 interviews with 10 nurses (5 E grades, 4 charge nurses/sisters), 1 emergency nurse practitioner and a consultant emergency physician, all of whom were experienced at triage within the department. The content of the interview was to describe the triage process and any issues perceived to affect this process. This formed a preliminary “task analysis” of the triage process—a technique used in human factors to describe the goals of a process and the tasks and subtasks required to achieve these goals.9,10 This was further developed through 16 h of observations over 11 days from August to October 2004, during which 97 patients were observed in the waiting room and triage area being triaged by 12 different triage staff (5 E grades, 2 F grades, 2 G grades, 2 emergency nurse practitioners and 1 consultant emergency physician). All sampling was opportunistic.
For the purpose of the study, the time the patient entered the triage area was taken as the start time for triage and the time the patient left the triage room was taken as the end of triage.
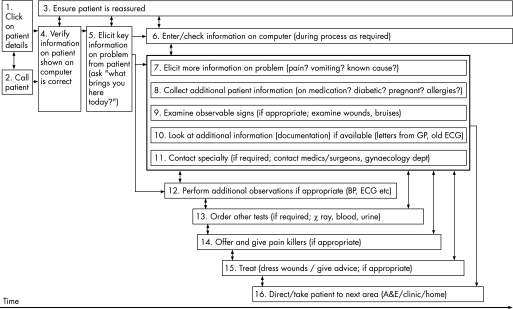
These data were used to produce a generic representational flowchart for the triage process, which was then finalised after review with the staff involved (fig 1). This was used to prioritise the relevant individual tasks embedded within the triage process that both take time and enhance patient safety, and to develop a list of factors as a protocol for phase 2.
Figure 1 Organisational flow chart of the triage process. A&E, accident and emergency; BP, blood pressure; ECG, electrocardiogram; GP, general physician.
Phase 2: The human factors researcher (ML) recorded data over 1870 min by observing 16 different members of staff carrying out the triage task. The sessions were undertaken during weekdays between 09:00 and 18:00 h using an opportunistic sample.
For each member of staff, the following information was recorded:
length of triage session observed;
number of patients triaged within the observed period;
time absent from the triage booth within observed period; and
grade of triage staff.
The information collected about the patient is shown in the appendix.
For this phase, analyses were planned to record the time taken, number of observation sessions taken and number of patients triaged in the observation period by each grade of triage staff. Also, the time absent and mean rate of patients for grade of staff were to be analysed.
Analyses were also planned for the average time spent waiting for triage and the duration of the triage process, and how these compared between the area and type of practitioner to whom the patient was sent.
Retrospective analyses were carried out on the tasks, events and factors influencing the productivity of the triage process—many of these analyses were expected on the basis of the data from phase 1, but it could not be predicted which would occur in phase 2 so a reanalysis was required.
For both phases, oral consent was obtained from staff members before the beginning of an observation period and for each patient before the start of the triage process. Patient data were anonymised at the data collection phase to ensure confidentiality. Staff identification information was coded for analysis. Ethical approval was obtained for the study from the local research ethics committee.
Results
Phase 1
See figure 1.
Phase 2
In Phase 2, the triage process was observed for 257 patients over a period of 2 months (Jan/Feb 2005). Table 1 shows the breakdown of the grade of staff and the mean results for the sessions.
Table 1 Observations taken in triage.
| E grade | F grade | G grade | ENP | Consultant emergency physician | Total | |
|---|---|---|---|---|---|---|
| Number of observation sessions | 10 | 5 | 3 | 4 | 1 | 23 |
| Number of different staff | 7 | 4 | 2 | 2 | 1 | 16 |
| Mean period (range) observing staff type, (min) | 71 (9–143) | 76 (6–144) | 125 (80–160) | 78 (19–167) | 92 | 81.3 (6–167) |
| Mean (range) number of patients triaged in observation session | 9.6 (1–20) | 12.2 (1–22) | 15.0 (5–20) | 10.25 (1–24) | 14 | 11.2 (1–24) |
ENP, emergency nurse practitioner.
Patient time in triage
Patient waiting in reception for triage
The mean time (min) that a patient waits from being registered on the computer in the reception to when he/she enters the triage booth for the first time is 13 min 34 s (n = 254, 95% confidence interval (CI) 12 min 21 s– to 14 min 47 s). This figure includes six patients whose triage was delayed because they were not in attendance in the waiting area when called into triage. Excluding these, the average is 13 min 21 s (95% CI 12 min 11 s to 14 min 31 s). There was no difference between the triage staff types for the times a patient was waiting in reception (Kruskal–Wallis test: χ2 = 7.76, df = 4, p = 0.10). The second triage desk was not opened at any time during the study periods, despite the long waits for triage.
Time taken to triage patients
The mean time for triage (min)—from entry to the triage booth to departure—is 4 min 19 s (n = 247).
Triage to specific areas
Table 2 shows the times taken to triage a patient to specific areas of the department and to specific types of practitioner within those areas. No patients were triaged to the resuscitation room from the waiting room triage area.
Table 2 Time in triage categorised according to the staff and area assigned responsibility for triaged patients.
| Type of practitioner | ||||||||
|---|---|---|---|---|---|---|---|---|
| ED | ENP | GP | Specialty staff | Triage—see and treat | All staff | |||
| Area responsible for the patient | ||||||||
| Majors | ||||||||
| Mean time | 4.6 | 5.3 | 4.7 | |||||
| 95% CI | 4 to 5.2 | 3.6 to 7 | 4.1 to 5.2 | |||||
| n | 81 | 7 | 88 | |||||
| Minors | ||||||||
| Mean time | 3.6 | 3.2 | 4 | 4.5 | 3.6 | |||
| 95% CI | 3.2 to 4.0 | 2.5 to 3.9 | 2 to 6 | 2–7 | 3.2 to 3.9 | |||
| n | 84 | 23 | 2 | 4 | 113 | |||
| Other area internal to the hospital | ||||||||
| Mean time | 6.6 | 6.6 | ||||||
| 95% CI | 5.3 to 7.9 | 5.3 to 7.9 | ||||||
| n | 12 | 12 | ||||||
| Alternate care provider (outside the hospital) | ||||||||
| Mean time | 4.7 | 5.9 | 5.3 | |||||
| 95% CI | 3.4 to 6.0 | 3.8 to 8 | 4.1 to 6.6 | |||||
| n | 9 | 10 | 19 | |||||
| Home | ||||||||
| Mean time | 4.8 | 4.8 | ||||||
| 95% CI | 3.2 to 6.4 | 3.2 to 6.4 | ||||||
| n | 15 | 15 | ||||||
| All areas | ||||||||
| Mean time | 4.1 | 3.2 | 4.6 | 5.8 | 5.2 | 4.3 | ||
| 95% CI | 3.8 to 4.5 | 2.5 to 3.9 | 3.4 to 5.7 | 94.8 to 6.8 | 4 to 6.5 | 4 to 4.6 | ||
| n | 165 | 23 | 11 | 23 | 25 | 247 | ||
ED, emergency department; ENP, emergency nurse practitioner; GP, general practitioner.
Significant differences were found in the times taken to triage a patient between the areas to which a patient was triaged (Kruskal–Wallis χ2 = 25.0, df = 4, p = 0.001) as well as the persons responsible for their care (χ2 = 18.7, df = 4, p = 0.001). Within groups, there was a significant difference between those triaged to the emergency department staff in the majors and in the minors (Mann–Whitney U = 2701.5, p = 0.02).
Triage to specialty
However, there was no significant difference in triaging a patient to an alternate care provider outside the hospital compared with an internal specialty area within the hospital (Mann–Whitney U = 79.5, p = 0.16). There was a significant increase in triage time for those triaged to the responsibility of specialty staff (anywhere in the hospital) compared with those triaged to the responsibility of the emergency department staff (Mann–Whitney U = 1077.5, p = 0.001).
There was no significant difference in triage time between those patients who were triaged to different areas but who were all to be seen by the specialty staff (Kruskal–Wallis χ2 = 2.5, p = 0.28).
Within this study, there was an overall increase in the time to triage patients who were deemed by triage as requiring specialty care (Mann–Whitney U = 1929, n = 29, p = 0.001), but no difference in triage time regarding whether the specialties accepted or refused the patients (Mann–Whitney U = 49.5, p = 0.30).
Together, these statistics imply that any contact with speciality—whether the patient is to be seen within the emergency department or within the specialty area within the hospital—causes an increase in triage time.
Triage of general practitioner‐referred patients
In all, 4 of the 247 patients arrived in the triage area with a letter of referral from a general practitioner to the inpatient specialty, but the specialties did not accept responsibility for these patients. The time for triage for these patients was consistent with that for specialty referral, but the end result was triage to be seen by the emergency department staff. In addition, there were 13 patients who did not have referral letters but who were referred directly to specialties as it was thought that this was most appropriate, and these patients were accepted by the inpatient specialty teams.
To consider the impact of the local “see and treat” process, the data from triage “see and treat” were merged with those advised to see their own general practitioner—giving a total of 34 patients who were seen and treated—or who left the department directly after the triage process concluded. Using this group, there was no significant difference in the time taken to see and treat patients from the time taken to see those patients who were subsequently seen within the department (Mann–Whitney U = 3022, p = 0.1). However, patients who received active treatment in triage (wound dressing, arranging tests and occasional prescriptions) took significantly longer to triage than those patients who were triaged into the department (Mann–Whitney U = 298.5, p = 0.02).
Tasks, events and factors influencing the productivity of triage
The process of triage is complex and unique in its content for individual patients; hence, it cannot be defined in a consistent order or uniformly. As a result, generic productivity cannot be assessed by timing the individual subtasks. Therefore, instead, the frequency with which subtasks were performed within triage was analysed for the statistical effect on the overall time of triage—as shown in table 3. Table 4 illustrates the occurrence of events that do not directly contribute to the streaming process and completion of the objectives of triage, as well as factors that could have a negative influence on quality and productivity and those that could be seen to distract and/or delay the triage staff in their tasks.
Table 3 Tally chart of examinations carried out and tests ordered in triage.
| Factors | Yes | No | Missing data |
|---|---|---|---|
| Tasks carried out in triage | |||
| Visual examination carried out of injury/sign | 112 | 138 | 7 |
| Examine documentation (reading letters from GPs or notes from the patient's previous admissions) | 37* | 214 | 6 |
| Observations and tests carried out in triage | |||
| ECG carried out | 22* | 232 | 3 |
| Measure temperature | 37* | 213 | 7 |
| Measure O2 saturations | 44* | 207 | 6 |
| Measure pulse | 43* | 208 | 6 |
| Measure blood pressure | 38 | 212 | 7 |
| Measure blood glucose | 5 | 244 | 8 |
| Tests ordered to be carried out within the department | |||
| Order urine test | 20 | 228 | 9 |
| Order x rays | 21 | 228 | 8 |
| Order blood tests | 0 | 248 | 9 |
ECG, electrocardiogram; GP, general practitioner.
*Shown to be related to a significant increase in triage time where time data were recorded: Mann–Whitney U test p<0.05 (n = 251 for examining documentation, measuring O2 saturations, measuring pulse; n = 253 for ECG, n = 250 for measuring temperature).
Table 4 Tally chart of occurrences and distractions in the triage process.
| Factors | Yes | No | Missing data |
|---|---|---|---|
| Supplementary task factors | |||
| Temporary dressing given before waiting for full ED examination | 6 | 250 | 1 |
| Time spent in preparing documentation for patient | 25* | 230 | 2 |
| Triage staff absent when patient is in triage | 22* | 234 | 1 |
| Information sought to support the triage task decision making | 16* | 238 | 3 |
| Support factors | |||
| Specialty giving undesirable response | 5 | 250 | 2 |
| Problems with phone/bleep contact (wrong/not answering) | 7 | 248 | 2 |
| Porter problems | 4 | 251 | 2 |
| Triage staff escorting patient into the department | 65* | 180 | 12 |
| Patient factors influencing triage task complexity | |||
| Patient gives an “inappropriate history” as recorded by triage staff on computer | 11 | 244 | 2 |
| Patient is relabelled from code given at reception to code given at triage | 76 | 176 | 5 |
| Labelled from chest pain to other code | 6 | ||
| Labelled from other code to chest pain | 7 | ||
| Patient does not have the appropriate documents | 3 | 252 | 2 |
| Patient has language problems | 54 | 201 | 2 |
| Patient behaves violently (verbal or physical) | 0 | 255 | 2 |
| Patient has experience/knowledge in clinical practice | 6 | 249 | 2 |
| Equipment‐related factors | |||
| Patient requiring wheelchair | 7 | 248 | 1 |
| Equipment missing or failed in triage | 8 | 247 | 2 |
| Addressed by leaving triage | 6 | ||
| Addressed by suboptimal triage process | 2 | ||
| Computer problems | 12* | 243 | 2 |
| Drugs cupboard keys missing | 0 | 254 | 3 |
| Interruptions | |||
| Triage staff is interrupted by paramedic/external staff (eg, hospital suppliers, staff visitors) | 6 | 249 | 2 |
| Triage staff is interrupted by ED/local hospital staff | 25 | 230 | 2 |
| Triage staff is interrupted by patient/family member | 28 | 227 | 1 |
| Interrupted by phone calls relating to current patient | 15* | 240 | 2 |
| Specialty expected | 5 | ||
| Not expected but triaged to a specialty | 4 | ||
| Interrupted by phone calls not relating to current patient (other patient/issue) | 23* | 232 | 2 |
ED, emergency department.
*Shown to be related to a significant increase in triage time when the time data were recorded: Mann–Whitney p<0.05 (n = 255 for preparing documentation, triage staff absent when patient in triage, computer problems, phone calls relating to current patient, phone calls not related to current patient; n = 254 for where information is sought to support the triage task, n = 244 for when the triage staff escorted the patient into the department).
Staff triage data
Table 5 shows the data of the actions of the staff as recorded over the whole observational sessions. From the number of observation sessions involving each staff grade, the number of different staff each session involved and the mean period observed, was recorded the time that the triage staff were away from the triage area and the number of patients triaged in the observed period were recorded. From this, the fraction of time absent (both when a patient is present in triage and between patients) and the actual rate at which patients were triaged could be calculated.
Table 5 Staff triage session timing.
| E grade | F grade | G grade | ENP | Consultant | Total | |
|---|---|---|---|---|---|---|
| Mean fraction of time absent (95% CI) | 0.13 (0.03 to 0.22) | 0.11 (0.05 to 0.18) | 0.18 (0.04 to 0.31) | 0.12 (0.09 to 0.15) | 0.25 | 0.14 (0.09 to 0.18) |
| Observed min–max | 0–0.45 | 0–0.2 | 0.05–0.28 | 0.09–0.16 | 0–0.45 | |
| Mean rate of triage—patients/hour (95% CI) | 7.8 (6.8 to 9.15) | 10.1 (8.77 to 11.39) | 6.8 (3.59 to 10.01) | 7.2 (4.44 to 9.96) | 9 | 8.4 (7.28 to 9.1) |
| Observed min–max | 5.4–12 | 9–12.6 | 3.6–9 | 3–9 | 3–12.6 |
ENP, emergency nurse practitioner.
The average fraction of time absent for all grades was 0.14 (a period of just >8 min/h). No significant differences were found in the fraction of time absent between the grades of staff or individual staff members (Kruskal–Wallis: grades—χ2 = 2.71, df = 4, p = 0.61; individuals—χ2 = 16.04, df = 15, p = 0.38).
The “rate” of triaging patients was on average 8.2 patients/h (one patient every 7 min and 9 s, including the necessary time for preparation between patients).
There was no difference between grades of staff or individual staff members on the rate of triage (Grades: χ2 = 7.63, df = 4, p = 0.11; individuals χ2 = 18.29, df = 15, p = 0.25), although it should be remembered that there would be variation in the case mix of the patients seen.
Discussion
The study has shown that observation of a process and human factors analysis can help determine areas for future work and research as well as assist staff in understanding their work patterns. There were no complaints about the presence of a researcher, and no patient refused to enter the study. Staff members readily participated in the interview process and freely discussed their thought processes. Although there might have been an effect on some of the behaviours owing to the presence of the researcher, there is no evidence that this significantly altered the results of the observations.
This study has highlighted some important issues in the management and implementation of the triage process.
Main findings
Factors affecting triage time
The triage process was longer for patients who were expected by specialties and/or triaged to specialties, although it might have been expected that they would be easier to sort as the pathway was predetermined. This process generally required supplementary phone communications which took considerable time, and although there was generally evidence that the general practitioner had recorded vital signs, the triage staff chose to repeat these and thus no time was saved. Although repetition of this process may improve the quality of care for this individual patient, there is a risk that the delay caused may impede care for other patients waiting. Notification of the arrival of a specialty‐expected patient could be undertaken by clerical staff after a preliminary review by the triage nurse to ensure patient safety and after initial investigations are ordered—thus, vital signs could be taken by the specialty staff without causing delays to patients of unknown criticality.
Ordering x rays was not a feature that had any significant effect on the time to triage; hence, assuming that this foresight improves the overall efficiency of the pathway supports the conclusions of Lindley‐Jones and Finlayson5 that ordering x rays in triage should be continued.
Given that active “see and treat” significantly increases the triage time while reducing the number of patients waiting to be seen within the clinical area, thought must be given to the potential effect on the overall patient throughput by tying up the triage practitioners for long periods with any individual patient.
It could be suggested that the department should develop clear clinical criteria for “see and treat”, as well as process management criteria for when see and treat would be useful and when it would cause delays to most patients.
Waiting time
Although there was no difference between the rate of triage between grades of staff, there was a significant difference in waiting times to be triaged between staff, and thought should be given to the most appropriate practitioner undertaking triage and the departmental response when the number of patients presenting outstrips the capacity to triage in a timely way. The department policy to open a second triage desk was not activated as during busy times there were no spare staff available to undertake triage. Alternatives to the problem of waiting for triage need to be found, including reducing the average time taken for triage and reducing delays. The average time for triage of <5 min indicates that up to 12 patients could be triaged per hour if there were no other delays or absences from triage. The rate of triage of a mean of 8 patients/h may be more realistic, and builds in the capacity to undertake the occasional see and treat as well as to respond to the unwell patient by immediate transfer to the clinical area.
Time absent from triage
Staff spend on average just over 8 min/h away from the triage area, a period that could be used to triage at least one more patient and a delay that risks breaching the 15‐min waiting time criteria. Most of this absent time consistently involved escorting patients into the majors areas of the department. It should be noted that 67% of the total time that the triage staff were absent was because of their escorting the patients into the main department area, a task that could be carried out by a porter. Also, 17% of the time was spent to collect equipment such as drugs, water or dressings—something that could be tackled with checks at handover—14% of the time was spent to obtain or convey information, and 1% was spent on clinically necessary tasks such as “washing hands to treat a specific problem”. This task has probably evolved due to a lack of available porters, and is affected by the layout of the emergency department. Although it would be desirable to have slack in the system to allow staff to catch up, a consistently used task that causes a “lag” could be best distributed to other staff. Staff in interviews emphasised the importance of oral handover of findings and plan, as emphasised in other studies,11 and reflect the limitations of the computerised system in recording the triage staff analyses of the problem and decision making.
Limitations
Timing method
In this study, the time data relied to a large degree on the computerised record of triage—this restricted the data to being recorded at the last minute—whereas in many cases using “seconds” data would give a more accurate reflection of how time is used.
Patient sample
A factor that must be taken into account though is the variability created by the sample of patients. This study was not carried out as a scientific “repeated measures” study, so staff performance cannot be compared. As the study was an opportunistic observational study, no attempt was made to compare the sample population with the overall population in terms of sex and age. It is therefore possible that there was overall a different spread of patients to the mean for the department. Similarly, sampling patients at night and weekends may have given more information on other influences on the triage process, including the out‐of‐hours case mix, potentially disruptive patient behaviour and a generally busier department. It is notable that none of the patients were violent, which could be an attribute of the sampling time or potentially a Hawthorne effect as a result of the presence of the researcher completing the observational study. However, as the study is based on observation of human factors, these limitations do not invalidate the findings from the data obtained.
Effect on outcome
The quality of triage with respect to its perceived correctness downstream or its effect on speed of treatment for each patient was not assessed within this study.
Quality improvement initiatives
In response to the study, there have been several initiatives including a rota change to allow a float nurse to be available to do secondary triage, an increased emphasis on handwashing and better equipment available in the second triage area.
Conclusions
This study has shown that taking a systems approach is feasible in the emergency department and can help to identify both problems and feasible solutions in a non‐judgemental manner. Although only looking at a small part of the process, the study has helped the department in identifying possible areas for future improvement, including the management of specialty‐expected patients and clearer guidance for their “see and treat” process as well as the improvements listed above. Other processes within the department may benefit from such human factors analysis, including decision making in “grey cases” and referral processes for observation or clinical decision units. Although the results may not be generalisable, it is hypothesised that the methods would be feasible and useful in other emergency departments.
Supplementary Material
Acknowledgements
We thank Charles Vincent of the Clinical Safety Research Unit of Imperial College, Professor Arun Gupta, Consultant Intensivist, and Dr Adrian Boyle, Consultant Emergency Physician at Addenbrooke's Hospital, for their advice and support. We also thank the staff of the Accident and Emergency department at St Mary's Hospital for their participation in the work.
Appendix 1: List of patient information collected
For each patient contact, the following information was recorded.
Time measures:
Time from registration to being called for triage—obtained from the computer
Duration of triage—from when they enter the triage booth to when they leave—obtained from the computer
Time spent alone within the triage area—obtained from direct observation.
Features of the triage process:
Grade of staff member triaging
Did the patient miss his/her first call into triage?
Patient code assigned at reception (chest pain, shortness of breath, unwell adult, etc)
Patient code assigned at triage (chest pain, shortness of breath, unwell adult, etc)
Was the patient relabelled from reception to triage?
Area assigned for patient's care (specialty, minors, majors, emergency nurse practitioner, home, etc)
Was the patient triaged to “see and treat”?—If so, was this advice or active treatment?
Observations carried out in triage (ECG, blood pressure, O2, pulse, glucose, temperature, etc)
Tests ordered to be carried out within the department (urine, x ray, blood)
Supplementary tasks carried out in triage (temporary dressings, preparation of documentation, etc)
Support factors that may have affected triage (problems with specialties, porters, etc)
Patient factors that may have affected triage (language problems, missing documents relevant to their triage, patient having clinical knowledge)
Equipment‐related factors that may have affected triage (requirements for wheelchair, failed or missing equipment in triage)
Interruptions (paramedic, other patients, phone‐calls).
Footnotes
Funding: This work was funded by the Department of Health Patient Safety Research Programme.
Competing interests: None.
Ethical approval: Ethical approval was obtained from the Local Research Ethics Committee, St.Mary's Hospital, London, UK.
References
- 1.Department of Health Reforming emergency care: first steps to a new approach. Crown Copyright. London: DOH, 2001
- 2.Cooke M W, Arora P, Mason S. Discharge from triage: modelling the potential in different types of emergency department. Emerg Med J 200320131–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Service Your guide to the NHS. Crown Copyright. London: NHS, 2001
- 4.Paulson D L. A comparison of wait times and patients leaving without being seen when licensed nurses versus unlicensed assistive personnel perform triage. J Emerg Nurs. 2004;30: 4, 307–11, [DOI] [PubMed]
- 5.Lindley‐Jones M, Finlayson B J. Triage nurse requested x rays—are they worthwhile? J Accid Emerg Med 200017103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindley‐Jones M, Finlayson B J. Triage nurse requested x rays—the results of a national survey. J Accid Emerg Med 200017108–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooke M W, Wilson S, Pearson S. The effect of a separate stream for minor injuries on accident and emergency department waiting times. Emerg Med J 20021928–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leaman A M. See and treat: a management driven method of achieving targets or a tool for better patient care? One size does not fit all. Emerg Med J 200320118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirwan B, Ainsworth L.A guide to task analysis. London: Taylor & Francis, 1992
- 10.Shepherd A.Hierarchical task analysis. London: Taylor & Francis, 2001
- 11.Behara R, Wears R, Perry S.et al A conceptual framework for studying the safety of transitions in emergency care. Adv Patient Saf 20052309–2321. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.