Abstract
Background
Recent evidence shows a substantial short‐term risk of ischaemic stroke after transient ischaemic attack (TIA). Identification of patients with TIA with a high short‐term risk of stroke is now possible through the use of the “ABCD Score”, which considers age, blood pressure, clinical features and duration of symptoms predictive of stroke.
Aim
To evaluate the ability of dichotomising the ABCD Score to predict stroke at 7 and 90 days in a population with TIA presenting to an emergency department.
Methods
A retrospective audit was conducted on all probable or definite TIAs presenting to the emergency department of a metropolitan hospital from July to December 2004. The ABCD Score was applied to 98 consecutive patients with TIA who were reviewed for subsequent strokes within 90 days. Patients obtaining an ABCD Score ⩾5 were considered to be at high risk for stroke.
Results
Dichotomising the ABCD Score categorised 48 (49%) patients with TIA at high risk for stroke (ABCD Score ⩾5). This high‐risk group contained all four strokes that occurred within 7 days (sensitivity 100% (95% confidence interval (CI) 40% to 100%), specificity 53% (95% CI 43% to 63%), positive predictive value 8% (95% CI 3% to 21%) and negative predictive value 100% (95% CI 91% to 100%)), and six of seven occurring within 90 days (sensitivity 86% (95% CI 42% to 99%), specificity 54% (95% CI 43% to 64%), positive predictive value 12.5% (95% CI 5% to 26%) and negative predictive value 98% (95% CI 88% to 100%)). Removal of the “age” item from the ABCD Score halved the number of false‐positive cases without changing its predictive value for stroke.
Conclusion
In this retrospective analysis, dichotomising the ABCD Score was overinclusive but highly predictive in identifying patients with TIA at a high short‐term risk of stroke. Use of the ABCD Score in the emergency care of patients with TIA is simple, efficient and provides a unique opportunity to prevent stroke in this population of patients.
Transient ischaemic attack (TIA) is no longer considered a benign condition. Recent evidence estimates the risk of ischaemic stroke after a TIA to be as high as 5% at 48 h, 10% at 1 month and 20% at 12 months.1 This substantial short‐term risk now requires TIA to be treated as a medical emergency, with urgent evaluation and management, particularly for those at highest risk of subsequent stroke.2 The identification of patients at high short‐term risk is particularly important to emergency departments such as those of Australia and the UK that do not admit all presenting patients with TIA. The detection of these high‐risk patients is now possible through the use of clinical features that have been developed into a scoring system called the “ABCD score” (which considers age, blood pressure, clinical features and duration of symptoms).3
The ABCD Score is a simple six‐point scoring system (table 1) that was derived in a population‐based cohort of patients with TIA in the Oxfordshire Community Stroke Project using variables that were previously reported as independent predictors of stroke after a TIA. The authors validated the score in two independent cohorts: the Oxford Vascular Study and a hospital clinic cohort. Validation of the ABCD Score found that most strokes (95%) occurred in those with a total score of five or six. These data suggest that the ordinal scoring of the ABCD could be dichotomised into high‐risk (score ⩾5) and low‐risk (score ⩽4) groups.
Table 1 ABCD Scoring System.
| Variable definition | Score |
|---|---|
| Age (years) | |
| <60 | 0 |
| ⩾60 | 1 |
| Blood pressure (mm Hg) | |
| SBP >140 or DBP ⩾90 | 1 |
| Clinical features | |
| Any unilateral weakness (face/hand/arm/leg) | 2 |
| Speech disturbance (without motor weakness) | 1 |
| Other | 0 |
| Duration of symptoms (min) | |
| <10 | 0 |
| 10–59 | 1 |
| >60 | 2 |
DBP, diastolic blood pressure; SBP, systolic blood pressure.
Presently, only one external validation of the ABCD Score has been published, which found the score to have limited use in the risk stratification of patients with TIA.4 However, the results of this validation study were limited by inclusion criteria that may have missed many strokes occurring within 24 h of the TIA event, resulting in a low number of stroke events (<2%). Further, the study used an outcome measure (a composite of stroke or death, vessel stenosis or a cardioembolic source) and timeframe (90 days) different from the original study. These limitations warrant further evaluation of the ABCD Score in a clinical setting. The aim of this validation study was to assess the ability of dichotomising the ABCD Score to predict stroke at 7 and 90 days in a probable or definite population with TIA presenting to an emergency department in a metropolitan hospital.
Methods
Patients and setting
The hospital is a 426‐bed tertiary university teaching hospital, located in a metropolitan city in Australia (Box Hill Hospital, Melbourne, Victoria, Australia). The emergency department assesses about 38 000 patients per year and admits 350–400 patients with stroke to the stroke unit. At the time of this study, there were no specific protocols in the emergency department for the treatment or admission of patients with TIA.
Consecutive patients with TIA presenting to the emergency department between July and December 2004 were identified from a medical records database. Patients with a primary emergency department diagnosis of TIA made by a doctor in the emergency department, as indicated in the database or medical notes in the emergency department, were included. Patients with symptoms lasting >24 h were excluded from analysis. This population was chosen to reflect emergency department clinical practice and capture all probable patients presenting with a TIA event.
Data collection and analysis
A standardised form was used to extract data from medical records in the emergency department. Data collected included age, sex, blood pressure at the time of admission, duration of TIA symptoms, presence of unilateral weakness (of face, hand, arm or leg), speech disturbance (dysarthria, dysphasia or both) and presence of risk factors. These data were used to determine the ABCD Score for each patient, which was performed blinded to the 90 day follow‐up.
Follow‐up was obtained by review of medical records (64%) and telephone inquiry (36%) for stroke events within 90 days of admission of the TIA event. The definition of stroke was any stroke (by World Health Organization criteria5) occurring after the full resolution of the initial TIA event. Data were collected and analysed by experienced research nurses. This study was part of a quality assurance audit of patients with TIA and was exempt from requiring ethical approval.
Owing to the retrospective nature of the data collection, published methods were followed to reduce potential bias.6 These included using an experienced abstractor, clear inclusion and exclusion criteria, clear definitions and extraction points for data collection, a standardised data collection form, description of sampling methods, random independent review of data and a predetermined plan for missing data.
Data were entered into a Microsoft Access database and analysed using SPSS for Windows, V. 10.0.1. Frequencies of each item in the score were determined. Scores were dichotomised into high‐risk and low‐risk groups, and the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of each group's ability to predict stroke was calculated for the 7‐day and 90‐day follow‐up periods.
Results
For the 6‐month study period, follow‐up was available for 98 of 102 (96%) patients who presented with a primary emergency department medical diagnosis of TIA. The mean age of the 98 included patients was 73 years (SD 14.5 years), and 50% were women. Risk factors among patients included hypertension (54%), hypercholesterolaemia (32%), diabetes (18%) and atrial fibrillation (12%).
The median time from onset of symptoms to presentation at hospital was 135 min (range 25 min to 48 h). The neurology team was consulted for 44 (45%) cases. Most patients, 53 (54%), were discharged directly from the emergency department. Only 22% of those retrospectively categorised at high risk by the ABCD Score were admitted to hospital. Within 7 days of the TIA event, four patients had strokes, and this number increased to seven by 90 days (table 2). Most of the patients (three of four) with strokes in the 7‐day follow‐up period had been discharged directly from the emergency department without a formal neurology review.
Table 2 Details of patients experiencing stroke within 90 days of the transient ischaemic attack.
| Age (years) | Sex | ABCD Score | Days to stroke | Admitted to hospital for TIA event | Neurology consult in ED | |
|---|---|---|---|---|---|---|
| 1 | 56 | M | 5 | 1 | N | Y |
| 2 | 78 | M | 6 | 1 | N | N |
| 3 | 42 | F | 5 | 2 | N | N |
| 4 | 59 | M | 5 | 3 | N | N |
| 5 | 88 | M | 6 | 64 | Y | Y |
| 6 | 49 | M | 2 | 84 | Y | Y |
| 7 | 72 | M | 6 | 90 | Y | N |
ABCD, age, blood pressure, clinical features and duration of symptoms; ED, emergency department; F, female; M, male; N, no; TIA, transient ischaemic attack; Y, yes.
The most common clinical features of the ABCD Score were age ⩾60 years (79%), duration of symptoms >60 min (79%), increased blood pressure (73%) and unilateral weakness (57%; table 3). The only feature seen in all patients with subsequent strokes at both 7 and 90 days was duration of symptoms >60 min. Increased blood pressure and unilateral weakness were also seen in all four strokes occurring within 7 days.
Table 3 Frequency of scores and number of strokes.
| Item definition | Frequency n (%) | Stroke events (n) | |
|---|---|---|---|
| 7 days | 90 days | ||
| Age (years) | |||
| <60 | 21 (21) | 3 | 4 |
| ⩾60 | 77 (79) | 1 | 3 |
| Blood pressure (mm Hg) | |||
| SBP>140 or DBP ⩾90 | 72 (73) | 4 | 6 |
| Clinical features | |||
| Any unilateral weakness (face/hand/arm/leg) | 56 (57) | 4 | 6 |
| Speech disturbance (without motor weakness) | 19 (19) | 0 | 0 |
| Other | 23 (23) | 0 | 1 |
| Duration of symptoms (min) | |||
| <10 | 12 (12) | 0 | 0 |
| 10–59 | 9 (9) | 0 | 0 |
| >60 | 77 (79) | 4 | 7 |
DBP, diastolic blood pressure; SBP, systolic blood pressure.
Dichotomising the ABCD Score categorised 48 (49%) patients at high risk for stroke (table 4). The high‐risk group contained all four strokes that occurred within 7 days (sensitivity 100% (95% confidence interval (CI) 40% to 100%), specificity 53% (95% CI 43% to 63%), PPV 8% (95% CI 3% to 21%) and NPV 100% (95% CI 91% to 100%)) and six of the seven strokes that occurred within 90 days (sensitivity 86% (95% CI 42% to 99%), specificity 54% (95% CI 43% to 64%), PPV 12.5% (95% CI 5% to 26%) and NPV 98% (95% CI 88% to 100%)).
Table 4 The proportions of strokes occurring by 7 and 90 days stratified by the ABCD Score on admission (n = 98).
| ABCD Score | Patients, n (%) | Strokes, n (%) | |
|---|---|---|---|
| 7 days | 90 days | ||
| 0 | 1 (1) | 0 | 0 |
| 1 | 6 (6) | 0 | 0 |
| 2 | 7 (7) | 0 | 1 (14) |
| 3 | 21 (22) | 0 | 0 |
| 4 | 15 (15) | 0 | 0 |
| 5 | 28 (29) | 3 (75) | 3 (43) |
| 6 | 20 (20) | 1 (25) | 3 (43) |
| Total | 98 (100) | 4 | 7 |
The single stroke occurring in the 90‐day follow‐up that was retrospectively classified as low risk (ABCD Score = 2) was a posterior circulation stroke, in a patient who failed to renew a prescription for an antithrombotic drug after a failed vertebral stenting procedure.
Owing to the large number of patients (79%) aged ⩾60 years and the low number of stroke events for this variable, a retrospective analysis was performed to determine if the removal of this item would decrease the number of false‐positive cases identified at high risk of stroke. The removal of age decreased the number of patients incorrectly identified at high risk of stroke (false‐positive cases) from 44 to 21 at 7 days and from 42 to 19 at 90 days, without changing the score's ability to predict stroke. Owing to the small sample size and the small number of strokes, it was not possible to perform a logistic regression analysis for item redundancy.
In the study sample, three non‐stroke‐related deaths occurred as outpatients in the 90‐day follow‐up period, of which one (ventricular fibrillation arrest) was identified as a high short‐term risk of stroke by the ABCD Score.
Discussion
This is the first study to apply a dichotomised version of the ABCD Score to a cohort of probable or definite patients with TIA presenting to an emergency department. In our sample, the ABCD Score, although overinclusive, accurately predicted 100% of strokes that occurred within 7 days and 86% within 90 days in patients with TIA identified as high risk.
The specificity of the ABCD Score could potentially be improved by the removal of the age item. Most of our patients (79%) were aged ⩾60 years. The removal of the age item from the score decreased the false‐positive cases detected by more than half, with no change to the prediction of stroke at either 7 or 90 days. Although this finding is in keeping with the original validation phase conducted by the authors of the ABCD Score, who found that age was not a significant predictor of stroke in their validation cohort (hazard ratio 1.36 (95% CI 0.32 to 5.86), p value 0.68), substantiation in a larger prospective study is required before the age item could reliably be removed from the ABCD Scoring System.
Also of interest in the development of the ABCD Score was that atrial fibrillation was not of predictive value. This was confirmed in our sample, where only 12 (12%) patients either reported a history of atrial fibrillation or atrial fibrillation was observed on the electrocardiogram at the time of presentation. Of these patients, only one went on to have a stroke in the 7‐day follow‐up period, and this patient was identified as high risk by the ABCD Score.
The proportion of patients (79%) with duration of symptoms >60 min was higher in this study than in population‐based studies.3 This may be unique to patients presenting to the emergency department, as similar findings are seen in other hospital‐based studies,4,7 and may limit the findings of this study to that population.
The incidence of stroke in our population with TIA was 4% at 7 days and 7% at 90 days, matching data from larger hospital‐based7,8 and population‐based studies.9,10 The short‐term risk of stroke after TIA is in fact greater than the risk of myocardial infarction in patients presenting with acute and chronic chest pain.10,11 The urgency of the evaluation of chest pain is a standard of care that now needs to be applied to patients with TIA, particularly those deemed at high risk of stroke.
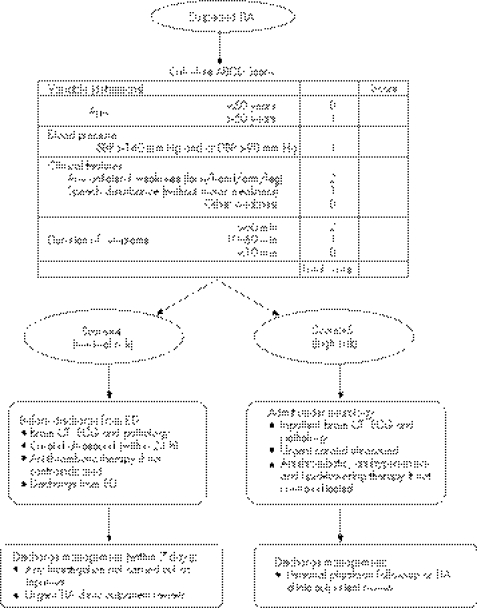
The findings of this study have resulted in a dramatic policy change in the management of TIA in our hospital. A clinical pathway (fig 1) using the ABCD Score has been introduced to the emergency department to triage the investigations and treatment for probable or definite patients with TIA, and is being prospectively analysed. In this pathway, a low ABCD Score does not require admission, but specific investigations must take place before discharge from the emergency department and the patient is seen in the outpatient TIA clinic within 7 days. A higher ABCD Score (5 or 6) requires urgent neurology consultation in the emergency department to determine the accuracy of diagnosis and to prioritise inpatient investigations. Prompt evaluation is important to ensure that symptoms have fully resolved, and also provides a unique opportunity to potentially prevent stroke in this population.12
Figure 1 Clinical pathway for patients suspected with transient ischaemic attack. ABCD, age, blood pressure, clinical features and duration of symptoms; CT, computed tomography; DBP, diastolic blood pressure; ECG, electrocardiography; ED, emergency department; SBP, systolic blood pressure; TIA, transient ischaemic attack.
A retrospective rather than prospective study was chosen to evaluate the ABCD Score owing to the extensive evidence of the high short‐term risk of stroke in patients with TIA. A prospective evaluation of the ABCD Score, without any clinical intervention, would not be ethically appropriate. The limitations and bias associated with a retrospective study of this type must be noted when interpreting our results, particularly as this study did not examine the effect of different treatment regimens on outcomes.
Conclusion
In conclusion, TIAs are now considered a medical emergency. Retrospectively, dichotomising the ABCD TIA score is highly predictive in identifying patients with TIA presenting to the emergency department at high short‐term risk of stroke. The rapid identification and treatment of high‐risk patients may provide a unique opportunity to prevent stroke in this patient population.
Acknowledgements
We thank the Emergency Department, Box Hill Hospital, Melbourne, Victoria, Australia, for their cooperation and assistance in developing the TIA clinical pathway.
Abbreviations
ABCD - age, blood pressure, clinical features and duration of symptoms
NPV - negative predictive value
PPV - positive predictive value
TIA - transient ischaemic attack
Footnotes
Competing interests: None.
References
- 1.Albucher J F, Martel P, Mas J L. Clinical practice guidelines: diagnosis and immediate management of transient ischemic attacks in adults. Cerebrovasc Dis 200520220–225. [DOI] [PubMed] [Google Scholar]
- 2.Johnston S C. Clinical practice. Transient ischemic attack. N Engl J Med 20023471687–1692. [DOI] [PubMed] [Google Scholar]
- 3.Rothwell P M, Giles M F, Flossmann E.et al A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet 200536629–36. [DOI] [PubMed] [Google Scholar]
- 4.Cucchiara B L, Messe S R, Taylor R A.et al Is the ABCD score useful for risk stratification of patients with acute transient ischemic attack? Stroke 2006371710–1714. [DOI] [PubMed] [Google Scholar]
- 5.Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 197654541–553. [PMC free article] [PubMed] [Google Scholar]
- 6.Worster A, Bledsoe R D, Cleve P.et al Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med 200545448–451. [DOI] [PubMed] [Google Scholar]
- 7.Johnston S C, Gress D R, Browner W S.et al Short‐term prognosis after emergency department diagnosis of TIA. JAMA 20002842901–2906. [DOI] [PubMed] [Google Scholar]
- 8.Hill M D, Yiannakoulias N, Jeerakathil T.et al The high risk of stroke immediately after transient ischemic attack: a population‐based study. Neurology 2004622015–2020. [DOI] [PubMed] [Google Scholar]
- 9.Coull A J, Lovett J K, Rothwell P M. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ 2004328326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lovett J K, Dennis M S, Sandercock P A.et al Very early risk of stroke after a first transient ischemic attack. Stroke 200334e138–e140. [DOI] [PubMed] [Google Scholar]
- 11.Johnston S C. Editorial comment—transient ischemic attacks are emergencies. Stroke 200536724. [PubMed] [Google Scholar]
- 12.Johnston D C, Hill M D. The patient with transient cerebral ischemia: a golden opportunity for stroke prevention. Can Med Assoc J 20041701134–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]