Abstract
This article reports the time course and clinical features of acute ethanol poisoning in an elderly man who had previously abstained from alcohol. Several hours after ingestion, severe hypotension and hypothermia developed, and the consciousness level was reduced. Supportive measures were sufficient to allow the patient's blood pressure and temperature to recover by 24 h post ingestion. The clinical manifestations of ethanol toxicity are often confounded by coexistent drug ingestion and variable periods of unconsciousness before arrival at hospital. This case highlights that hypotension and hypothermia may be explained on the basis of severe ethanol poisoning alone, in the absence of any other contributing factors. Clinical features of poisoning may be delayed by several hours and, therefore, patients presenting at the hospital should be considered for observation for at least 4 h after consumption of potentially toxic quantities. More severe toxicity should be anticipated in patients who normally abstain from alcohol.
An 80‐year‐old man presented at the Emergency Department, Royal Infirmary of Edinburgh, 1 h after acute ingestion of 750 ml vodka (40% alcohol by volume), as corroborated by the patient's wife. He had longstanding depression, and had taken deliberate drug overdoses 15 and 30 years earlier. The patient had abstained from alcohol for many years, and his only regular drug was mirtazepine 30 mg nightly. On initial assessment, the consciousness level was reduced, and he was responsive only to painful stimuli. Respiratory rate was 27/min, pulse 75/min, blood pressure 155/91 mm Hg and temperature 35.5°C; other detailed physical examinations were normal. Investigations showed venous bicarbonate 19 mmol/l, glucose 6.3 mmol/l and creatinine kinase 133 U/l; electrolytes, liver biochemistry, full blood count and coagulation time were normal. A resting electrocardiogram and chest radiograph were normal, and neither paracetamol nor salicylates were detected in the serum. Urinary toxicology screening was negative, and a passive breath alcohol concentration was 2.16%.
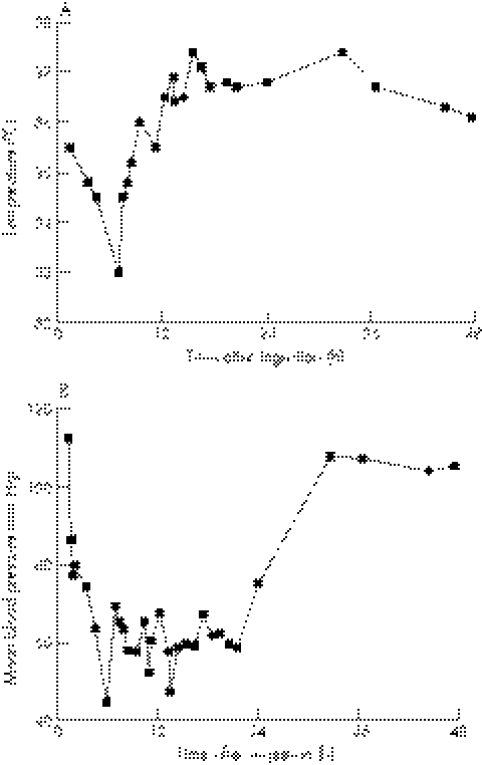
Within 30 min of arrival, the patient's consciousness level deteriorated and he became unresponsive. Blood pressure was 102/65 mm Hg, temperature 34.8°C, cough reflex intact and ventilatory effort satisfactory. Arterial blood analysis showed H+ 44 mmol/l, Paco2 5.1 kPa, Pao2 18.4 kPa, bicarbonate 21 mmol/l and lactate 1.9 mmol/l. His airway was secured with a nasopharyngeal tube, and resuscitation was by intravenous hydration, passive warming and supplemental oxygen. Close observation and supportive measures were directed at ensuring adequate hydration, normal electrolyte balance and tissue oxygenation. The patient's consciousness level, blood pressure and temperature gradually improved over 24 h (fig 1). There were no discernable effects on renal function, electrocardiographic variables or residual cognitive function. Plasma ethanol concentrations were 148 mmol/l (682 mg/dl) and 50 mmol/l (230 mg/dl) at 1.5 h and 21.5 h post ingestion, respectively.
Figure 1 (A) Mean blood pressure and (B) tympanic temperature with respect to time after alcohol ingestion. Mean blood pressure calculated as diastolic blood pressure+⅓(systolic blood pressure−diastolic blood pressure).
After recovery from the acute effects, the patient disclosed that he had intended to commit suicide by drowning, and had consumed alcohol for courage. He was unfamiliar with alcoholic beverages, so had tasted gin, whiskey and vodka, and, after finding vodka least offensive, drank the contents of a 750 ml bottle neat.
However, the patient became too intoxicated to carry out his plan. He denied concomitant drug ingestion. He was transferred to a psychiatric hospital for further assessment.
Discussion
This case emphasises the importance of hypotension and hypothermia as direct consequences of acute ethanol ingestion. These findings are in contrast with the minimal haemodynamic effects reported after consumption of moderate quantities of alcohol in elderly patients.1 Lack of alcohol tolerance, due to his usual abstinence, and exposure to high ethanol concentrations are probably responsible for the severe toxicity observed in this patient. An important aspect of this report is that the timing and quantity of alcohol ingested were clearly reported and corroborated, and the patient had not coingested any other drug and he did not regularly consume alcohol. Further, we were able to observe the clinical features from soon after ingestion until completely recovered. Lack of confounding factors, which are commonly present in patients who present at the emergency department after alcohol ingestion, allowed an unusual opportunity to establish the features directly attributable to acute ethanol ingestion.
Alcohol consumption is a major contributor to excess morbidity and mortality, and imposes a substantial healthcare burden to emergency departments and medical assessment units.2 Features of acute ethanol ingestion include slurred speech, ataxia, electrolyte imbalance and hypoglycaemia. Plasma ethanol concentrations of 76–98 mmol/l (350–450 mg/dl) are characteristically associated with severe toxicity, including seizures, arrhythmia, respiratory depression and profound metabolic acidosis.3 Concentrations >98 mmol/l (450 mg/dl) are potentially fatal, and associated with coma, respiratory arrest and circulatory collapse.3 There is a positive correlation between clinical effects and blood alcohol concentrations.4 Nonetheless, tolerance is an important factor determining the effects of acute ethanol ingestion, and clinical effects are more pronounced in alcohol‐naive patients who may experience severe toxicity at blood alcohol concentrations <22 mmol/l (100 mg/dl).
Maximum toxicity occurred at around 6 h post ingestion, suggesting that patients who present at hospital after consuming potentially toxic quantities of ethanol should be observed for at least 4–6 h after ingestion. Two‐point kinetic analysis found that plasma ethanol concentrations were decreasing at 5 mmol/l/h (23 mg/dl/h). This is consistent with previously reported values of 3 mmol/l/h (15 mg/dl/h) in non‐alcohol‐dependent adults, and 4–5 mmol/l/h (17–22 mg/dl/h) in alcohol‐intoxicated patients attending the emergency department.3,4 Clinical management consists of supportive care and close observation until the blood alcohol concentrations decrease to a non‐toxic levels. Haemodialysis may improve ethanol clearance, and should be considered in cases of severe poisoning, although evidence of improved clinical outcome is lacking.
In conclusion, acute ethanol ingestion may cause severe effects, including hypothermia, hypotension and reduced consciousness, especially in alcohol‐naive patients. Clinical effects might not become apparent until several hours after ingesting potentially toxic quantities of ethanol. Therefore, consideration should be given to monitoring the patient for at least 4 h after ingestion. Intensive supportive care is needed until ethanol concentrations fall to non‐toxic levels.
Acknowledgements
We thank Lisa Galloway, Royal Infirmary of Edinburgh, Edinburgh, UK, for her help in preparing the manuscript.
Footnotes
Competing interests: None declared.
References
- 1.Stott D J, Dutton M, Murray G D.et al Hemodynamic effects of a single moderate dose of alcohol in elderly subjects. J Stud Alcohol 199152377–379. [DOI] [PubMed] [Google Scholar]
- 2.James A, Madeley R, Dove A. Violence and aggression in the emergency department. Emerg Med J 200623431–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eckardt M J, File S E, Gessa G L.et al Effects of moderate alcohol consumption on the central nervous system. Alcohol Clin Exp Res 199822998–1040. [DOI] [PubMed] [Google Scholar]
- 4.Brennan D F, Betzelos S, Reed R.et al Ethanol elimination rates in an ED population. Am J Emerg Med 199513276–280. [DOI] [PubMed] [Google Scholar]