Abstract
Objective
To evaluate the convenience and utility of optic nerve ultrasonography (ONUS) in the evaluation of emergency patients with elevated intracranial pressure (EICP) due to traumatic or non‐traumatic causes.
Methods
This study was conducted between May 2005 and December 2005 in the emergency department of Meram Faculty of Medicine, Selcuk University. Patients with traumatic or non‐traumatic EICP were included in the study. Among these, 28 patients with EICP determined on cranial computed tomography (CCT) and a control group of 26 patients with no disease had the vertical and horizontal diameters of the optic nerves (ONs) of both eyes measured by ultrasonography (US). The measurements were done by wetting the closed eyelids and using a 7.5‐MHz linear probe.
Results
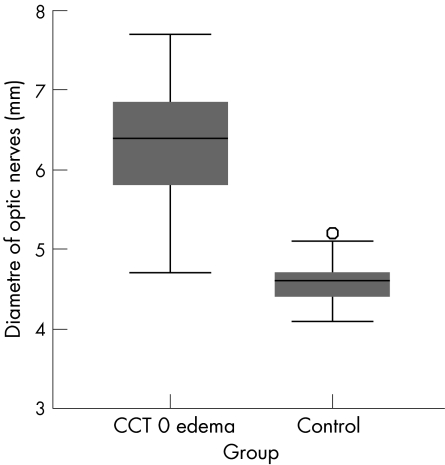
Horizontal and vertical diameters of both ONs of the 54 patients were measured and the averages calculated. The mean (SD) ON diameter for the group suspected of having EICP was found to be 6.4 (0.7) mm, and that for the control group to be 4.6 (0.3) mm. In the statistical analysis carried out between these two groups (t test), the difference was found to be significant at p<0.001.
Conclusions
In detection and follow‐up of EICP cases, such as cerebrovascular accident and trauma, ONUS is a practical, risk‐free, inexpensive, convenient and, if performed by experts, reliable method. As a result, although CCT may be more useful in diagnosis, ONUS may be more efficient in detecting EICP. In those cases where CCT and other conventional imaging methods are not available, ONUS can facilitate the diagnosis and help in treatment.
Owing to the increased burden faced by emergency services, monitoring methods have become more extensively used to accelerate patient circulation both in diagnosis and treatment. Ultrasonography (US) in particular has become an inseparable component of the emergency services.1
Patients with brain damage, which is most frequently based on traumatic and vascular causes and less frequently on intracranial mass or obstruction in the cerebrospinal fluid circulation, present to emergency services. Treatment in these patients depends on early diagnosis and hence on radiological monitoring, at the forefront of which is cranial computed tomography (CCT). Tomography, however, may not help in the early period in patients with elevated intracranial pressure (EICP), especially that resulting from vascular and traumatic causes. Furthermore, tomography is not available in every hospital, or this examination may sometimes not be performed because of instability in the patient's vital findings. In cases with EICP, dilation in optic nerve (ON) diameter and optic disc occurs, which may sometimes be observed during ophthalmoscopic evaluation.2,3,4 However, in most of these patients, the ophthalmoscopic evaluation is impossible or extremely difficult. As a result, in the last few years, optic nerve ultrasonography (ONUS) has been used more often in emergency services.5,6 In this study, the convenience and utility of ONUS were investigated in cases in whom EICP was likely to develop.
EICP may be present in emergency department patients with head trauma, hypoxia, intracranial haemorrhage and tumour complications. All of these groups may require rapid intervention.7,8 Early diagnosis of acute intracranial hypertension is essential to enable prompt, optimal treatment. The optic nerve sheath diameter (ONSD) is increased in EICP, and its measurement can be used to indirectly monitor increased intracranial pressure (ICP). 2,9
Although CCT may be available in most emergency departments, it may be unavailable for the detection of early EICP.5 CT uses ionising radiation. Initial head CT scan characteristics show a linear relationship to baseline ICP.10
The findings of EICP in CCT include:
changes in vertical sizes;
lessening in basilar cistern sizes;
narrowing or eliminating in sulci;
transfalcine herniation; and
changes in the rate of grey/white matter.10
Ocular US can detect pathology reflecting disease states outside of the eye, whereas evaluation of ONSD can detect EICP.11
Materials and methods
Study design and setting
This study was carried out prospectively on patients admitted to the Department of Emergency Medicine, Meram Faculty of Medicine, University of Selcuk, Turkey, from May 2005 to December 2005 with the findings of EICP on CCT, based on traumatic or non‐traumatic causes during normal working hours. They were enrolled once an increased ICP was shown on CCT. The study group included 28 patients (21 (75%) men of mean age 35.5 years). The control group included 26 healthy volunteers (21 (80%) men of mean age 34 years). All 54 participants were white. The patients presenting at emergency services underwent standard examination and treatment; ONUS was planned for those patients with brain injury, intracerebral haemorrhage, cerebral infarct and hypoxic brain with EICP findings on their CTT.
Box 1: Causes of increased optic nerve sheath diameter (ONSD)
In patients without EICP 12
Optic neuritis
Arachnoid cyst of the optic nerve
Optic nerve trauma
Anterior orbital or cavernous sinus mass
In patients with EICP 13
Any tumour or space‐occupying lesions of the CNS
Pseudotumour cerebri
Decreased CSF resorption (eg, venous sinus thrombosis, inflammatory processes, meningitis, subarachnoid haemorrhage)
Increased CSF production (tumours)
Obstruction of the ventricular system
Cerebral oedema, encephalitis
Craniosynostosis
Notes: CNS, central nervous system; CSF, cerebrospinal fluid; EICP, elevated intracranial pressure; ONSD, optic nerve sheath diameter
This study was conducted by a single US‐certified emergency medicine expert, who in addition has performed ONUS on more than 100 volunteers. For the US to be monitored, a 7.5 MHz linear US probe was used. The patient, his/her relatives and the control group were informed about the study and their consent was obtained. The control group included age‐ and sex‐matched healthy volunteers.
Methods and measurements
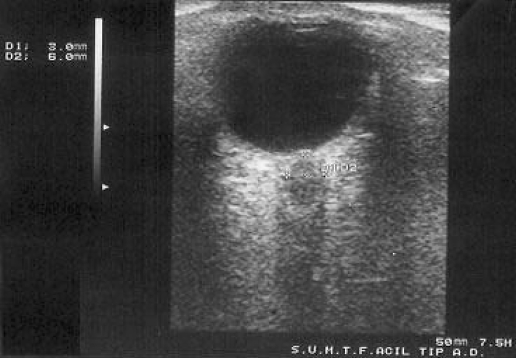
Patients with no EICP but with increased ON diameter were excluded from the study. Box 1 shows the causes of dilation in ON diameter in those with EICP.12,13 An ample amount of gel was applied to a 7.5 MHz‐linear US probe and then placed in a disposable plastic bag, thus preventing the feeling of discomfort in the eye due to the contamination and gel. The outer sides of the eyelids were wetted with water in order to facilitate penetration of the US waves. This method was more comfortable when compared with the standard method in which gel and probe are directly applied onto the eyelid, more reliable in terms of contagious diseases and more convenient in monitoring the ON vertically. With this technique, vertical and horizontal diametres of the ON in both eyes were measured four times.5 Since the measurements were done by a single person, concordance among them was good. ONSD was measured 3 mm behind the point where the ON entered the globe (fig 1).2,5,9
Figure 1 Optic nerve sheath diameter measured 3 mm behind the point where the optic nerve entered the globe.
Primary data analysis
The mean (SD) values of ONSD measurements were compared between EICP and control groups by two‐independent group t test, and a significant difference was determined between the two groups (t = 24.131; p<0.001). All statistical analyses were performed using SPSS V.12.0 program.
Sensitivity analysis
Since these measurements were done by one individual, the four ONSD values of both groups were evaluated in detail in terms of their concordance. In this evaluation, the concordance correlation coefficient formula, which is used in non‐categorical data, was applied.14
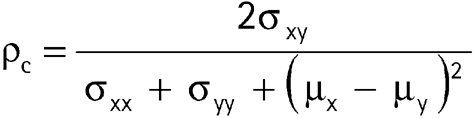 |
The values in hand were examined accordingly (table 1). A value >0.90 showed concordance among the measurements. In 5/6 evaluations this value was >0.90, and in only one evaluation was it slightly <0.90, thus proving agreement between our measurements.
Table 1 Concordance correlation coefficient*.
| Right horizontal–right vertical | 0.942 |
| Right horizontal–left horizontal | 0.929 |
| Right horizontal–left vertical | 0.89 |
| Right verticalleft horizontal | 0.917 |
| Right vertical–left vertical | 0.938 |
| Left vertical–left horizontal | 0.944 |
*Values >0.90 indicate concordance of the measurements.
Bland–Altman plots were used to demonstrate concordance between ONSD measurements. Figure 2 presents all possible pairwise concordance plots. The values, related with plots, as mean (2 SD) differences, are presented in table 2. As seen in table 1 and fig 2, Bland–Altman plots and the concordance correlation values agree on concordance between ONSD measurements. Differences between values were evenly distributed around the mean along the entire range of values.
Figure 2 Bland–Altman plots. RHor, right horizontal; RVer, right vertical.
Table 2 Mean (95% CI) and the confidence limits for Bland–Altman plots.
| Mean of differences | SE of differences | SD of differences | 95% CI for mean differences, mean (1.96 SE) | Confidence limits for Bland–Altman plots, mean (2 SD) | |
|---|---|---|---|---|---|
| Right horizontal–right vertical | −0.108 | 0.049 | 0.339 | −0.204 (−0.012) | −0.786 (0.569) |
| Right horizontal–left horizontal | −0.177 | 0.049 | 0.351 | −0.273 (−0.080) | −0.879 (0.526) |
| Right horizontal–left vertical | −0.177 | 0.065 | 0.451 | −0.305 (−0.05) | −1.079 (0.725) |
| Right vertical–left horizontal | −0.087 | 0.063 | 0.421 | −0.210 (0.036) | −0.929 (0.756) |
| Right vertical–left vertical | −0.040 | 0.054 | 0.365 | −0.147 (0.067) | −0.770 (0.690) |
| Left vertical–left horizontal | −0.089 | 0.052 | 0.351 | −0.192 (0.014) | −0.791 (0.613) |
Results
Characteristics of study subjects
The mean right eye ON horizontal diameter of these 28 patients was 6.3 (0.6) mm and the mean vertical diametre was 6.4 (0.6) mm; the mean left eye ON horizontal diameter was 6.4 (0.8) mm and the mean vertical diameter was 6.4 (0.8) mm. The average of all measurements of the ONs of 28 patients who had EICP according to CCT was 6.4 (0.7) mm.
The mean (SD) age of the 26 people in the control group was 33.4 (16) years. The mean right eye ON horizontal diameter of these 26 patients was 4.5 (0.2) mm and the mean vertical diameter was 4.5 (0.3) mm, whereas the mean left eye ON horizontal diameter was 4.7 (0.2) mm and the mean vertical diameter was 4.7 (0.3) mm. The average of all measurements of the ONs of this 26‐person group was 4.6 (0.3) mm (fig 3).
Figure 3 Optic nerve diameters in each group. CCT, cranial computed tomography.
Main results
The ON diameter of all subjects in the control group was evaluated as normal, whereas the ON diameter of all patients with brain oedema in their CCT was wider. As seen in fig 3, the mean diameters of optic nerves on CCT of patients with oedema were found to be higher than in controls.
Limitations
While ONUS is quite useful for application in patients with high intracranial pressure, it does not give information about the aetiology. The study population included patients admitted to the emergency department during normal working hours only. Clear and precise limits cannot be seen in US, which can cause different results even with measurements calculated on the same ON. The possibility for error also occurs due to the small size of the measurements (ie, 1/10 mm). Other factors affecting the reliability of the technique are the experience of the person taking the ON measurements by means of US, the quality of the device and the movement of the patient. Possible reasons for an increase in ONSD without EICP should be kept in mind.
Discussion
In previous studies, the first pathophysiological case reported to have developed after EICP has been cited as a case with oedema that occurred in the optic disc.3,4 The use of US in cases related to EICP has increased due to the expansion of US.5 Whereas US may not be as helpful as CCT in establishing the cause of intracranial lesions, it may be more successful in monitoring EICP in the early period.3
Hayreh,15 in his experimental study, noted that the first finding in EICP was dilation in the optic disc. His results support the finding of oedema on ONUS of all the patients in our study who had oedema in CCT. Later studies of Hayreh also support this.3,4 Compared with other evaluations, measurement of ON diameter is the quickest means for detecting EICP, and the easiest technique for this purpose in use today is US.
In the study carried out by Gangemi et al16 evaluating 40 patients with EICP syndrome due to various causes, ON was evaluated by means of the echographic technique. Their results showed that an increase in the ON diameter in EICP was observed earlier than any ophthalmoscopic finding.16 There are also other studies supporting this finding.11,17 Gangemi et al16 used the echographic technique instead of US. Determination of increased ONSD can be considered superior to other techniques as an indicator of EICP, and increased ONSD emerges earlier than the other findings evaluated by ophthalmoscopy.16
A relationship between the ONSD and ICP has been observed previously in a clinical setting as well. Normal ONSD measured by US has been reported to range from 4.7 to 5.0 mm.12,18 In the CCT of our study, there was a remarkable difference between the ONSD in patients with EICP findings and in the control group with no such findings. The mean (SD) of the four ON measurements (right vertical, right horizontal, left vertical and left horizontal) in the control group was 4.6 (0.3) mm vs 6.4 (0.7) mm in those with EICP (fig 3). Measurements obtained in the control group are close to and support values reported in previous studies.
Many patients present to emergency services with EICP. CCT is first among the techniques used for detection of EICP, but it does not demonstrate early EICP findings. The first finding in an EICP case is dilation in ON diameter.3 As a result, ONUS can be more useful than CCT, perhaps not in diagnosis, but in detecting EICP. For unconscious patients with no diagnosis, ONUS can be very helpful in eliminating an EICP cause and in leading these patients to CCT. ONUS is radiation‐free and non‐invasive, and has certain features which increase its convenience—portability, easy application, low cost, repeatability on request, bedside application, short application time and applicability even in the presence of unstable vital findings.
ONUS can also be used in the evaluation of an increase in ICP before lumbar puncture is applied, in the occasions of disaster, in the early evaluation of EICP and in follow‐up when it is difficult to reach CCT. However, knowing when a lumbar puncture will be dangerous is very important, as these patients are not always scanned, especially in emergency departments in the rest of the world. It can also help to identify the first patients to be sent for CCT. In light of this information, we recommend ONUS as a very useful and practical method in the evaluation and follow‐up of ICP.
Abbreviations
CCT - cranial computed tomography
EICP - elevated intracranial pressure
ICP - intracranial pressure
ON - optic nerve
ONSD - optic nerve sheath diameter
ONUS - optic nerve ultrasonography
US - ultrasonography
Footnotes
Competing interests: None declared.
References
- 1.Mateer J, Plummer D, Heller M.et al Model curriculum for physician training in emergency ultrasonography. Ann Emerg Med 19942395–102. [DOI] [PubMed] [Google Scholar]
- 2.Newman W D, Hollman A S, Dutton G N.et al Measurement of optic nerve sheath diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. Br J Ophthalmol 2002861109–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayreh M S, Hayreh S S. Optic disc edema in raised intracranial pressure. I. Evolution and resolution. Arch Ophthalmol 1977951237–1244. [DOI] [PubMed] [Google Scholar]
- 4.Hayreh S S. Optic disc edema in raised intracranial pressure. V. Pathogenesis. Arch Ophthalmol 1977951553–1565. [DOI] [PubMed] [Google Scholar]
- 5.Blaivas M, Theodoro D, Sierzenski P R. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med 200310376–381. [DOI] [PubMed] [Google Scholar]
- 6.Jang T, Aubin C. The use of serial ocular ultrasonography in the care of patients with head injury. Ann Emerg Med 200545336–337. [DOI] [PubMed] [Google Scholar]
- 7.Munch E C, Bauhuf C, Horn P.et al Therapy of malignant intracranial hypertension by controlled lumbar cerebrospinal fluid drainage. Crit Care Med 200129976–981. [DOI] [PubMed] [Google Scholar]
- 8.Blaivas M, Theodoro D. Comparison of perceived and actual times spent by residents performing ultrasound examinations on patients. Acad Emerg Med 200310397–399. [DOI] [PubMed] [Google Scholar]
- 9.Ballantyne J, Hollman A S, Hamilton R.et al Transorbital optic nerve sheath ultrasonography in normal children. Clin Radiol 199954740–742. [DOI] [PubMed] [Google Scholar]
- 10.Miller M T, Pasquale M, Kurek S.et al Initial head computed tomographic scan characteristics have a linear relationship with initial intracranial pressure after trauma. J Trauma 200456967–972. [DOI] [PubMed] [Google Scholar]
- 11.Hansen H C, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg 19978734–40. [DOI] [PubMed] [Google Scholar]
- 12.Ossoinig K C. Standardized echography of the optic nerve. Doc Ophthalmol Proc Ser 1993553–99. [Google Scholar]
- 13.Miller N R, Newman N J. eds. The essentials. Walsh & Hoyt's clinical neuro‐ophthalmology. 5th edn. Baltimore: Lippincott Williams & Wilkins, 1998
- 14.King T S, Chinchilli V M. A generalized concordance correlation coefficient for continuous and categorical data. Stat Med 2001202131–2147. [DOI] [PubMed] [Google Scholar]
- 15.Hayreh S S. Pathogenesis of edema of the optic disc. Doc Ophthalmol 196824289–411. [DOI] [PubMed] [Google Scholar]
- 16.Gangemi M, Cennamo G, Maiuri F.et al Echographic measurement of the optic nerve in patients with intracranial hypertension. Neurochirurgia 19873053–55. [DOI] [PubMed] [Google Scholar]
- 17.Galetta S, Byrne S F, Smith J L. Echographic correlation of optic nerve sheath size and cerebrospinal fluid pressure. J Clin Neuroophthalmol 1989979–82. [PubMed] [Google Scholar]
- 18.Guthoff R.Ultrasound in ophthalmologic diagnosis. A practical guide. New York: Thieme, 1991