Abstract
Aims
This study was conducted as a feasibility pilot for the Risk stratification Of Syncope in the Emergency department (ROSE) study. The secondary aim was to compare the performance of our existing emergency department (ED) guidelines with existing clinical decision rules (Osservatorio Epidemiologico sulla Sincope nel Lazio (OESIL) Score and San Francisco Syncope Rule; SFSR) at predicting short‐term (1 week and 1 month) and medium‐term (3 months) serious outcomes for patients with syncope presenting to the ED.
Methods
This was a prospective cohort study. All patients presenting with syncope aged ⩾16 years between 7 November 2005 and 7 February 2006 were prospectively enrolled.
Results
99 patients were recruited over a 3‐month period. 44 patients were admitted and 55 discharged from the ED. 11 patients had a serious outcome: 8 by 7 days and a further 3 by 3 months. Five patients died by 3 months and six others had an alternative serious outcome. All 11 patients had been admitted from the ED, 7 were at high risk, 4 were at medium risk and none were at low risk according to our existing ED guidelines. Percentages of serious outcomes were 0%, 2.9%, 8.0%, 22.7% and 37.5% for OESIL scores of 0, 1, 2, 3 and 4 respectively. 40 patients had none of the 5 SFSR high‐risk factors (0 serious outcomes = 0%) and 59 patients had an SFSR high‐risk factor (11 serious outcomes = 18.6%). The risk of serious outcome at 7 days, 1 month and 3 months was 8.1%, 8.1% and 11.1%, respectively.
Conclusions
A study to derive and validate a UK ED syncope clinical decision rule is feasible. This pilot study has evaluated the OESIL score, the SFSR and our existing ED guidelines, and has shown that each is able to identify an increased probability of medium‐term serious outcome in patients with syncope. The SFSR shows good sensitivity at the expense of an increase in admissions to hospital; however, our existing ED syncope guidelines and the OESIL Score, although being able to successfully risk stratify patients, are not sufficiently sensitive to be able to reduce admissions without missing patients at risk of a serious outcome. Undoubtedly there is a need for a simple UK‐derived clinical decision rule for patients presenting with syncope to enable safe, effective clinical care and to aid less experienced decision makers.
Syncope is a transient loss of consciousness with an inability to maintain postural tone followed by a spontaneous recovery.1 It accounts for 3% of emergency department (ED) visits and 1–6% of hospital medical admissions, affecting 6 per 1000 people per year.2,3 Clinical assessment of syncope is difficult owing to the heterogeneous nature of underlying causes, ranging from benign neurocardiogenic syncope to potentially fatal arrhythmias.
In 1983, Kapoor et al4 published the first prospective syncope study. The 12‐month mortality was 14%. Mortality was greatest in patients in whom a cardiovascular cause was identified (30%). Subsequent studies have shown that underlying heart disease in patients with syncope is associated with a poor prognosis.5 Recent emphasis has focused on risk stratification of patients with syncope. Although guidelines have been issued,6,7,8,9,10 evidence with respect to ED management is sparse. There are five risk stratification studies.11,12,13,14,15,16 All involved small numbers of patients and used different characteristics and outcome measures in their risk stratification tools. Only one study, US‐based, looked at short‐term adverse outcome,15,16 which is relevant to emergency medicine practice. No studies have been examined in a UK population.
With growing pressures on acute medical beds and an increasingly elderly population, a large study of this common presenting symptom is needed to identify high‐risk populations requiring further investigation and low‐risk patients who may be discharged safely. Accurate identification of patients would enable specific targeting of resources and prevent excessive investigation of patients with benign causes.
This study was conducted as a pilot for the Risk stratification Of Syncope in the Emergency department (ROSE) study. The primary aim was to demonstrate the feasibility of study recruitment and to test the study method before the main ROSE study. The secondary aim was to compare the performance of existing clinical decision rule (CDRs; The Osservatorio Epidemiologico sulla Sincope nel Lazio (OESIL) score and San Francisco Syncope Rule (SFSR)) with our existing departmental syncope guidelines (based on the European Society of Cardiology,9,10 the American College of Physicians (ACP)6,7 and the American College of Emergency Physicians guidelines8; table 1) to predict short‐term (7 days and 1 month) and medium‐term (3 month) serious outcomes for patients with syncope presenting to a UK ED.
Table 1 Our emergency department's existing syncope guidelines based on the European Society of Cardiology,9,10 American College of Physicians6,7 and American College of Emergency Physicians guidelines8.
| High risk (admit) | Medium risk (consider discharge with early outpatient review) |
|---|---|
| History findings | |
| Palpitations related to syncope | Age >60 years |
| Associated chest pain | No prodromal symptoms |
| Associated headache | Previous myocardial infarct |
| Related to exertion | Known history of valvular heart disease |
| Family history of sudden death at <60 years | Known angina/coronary artery disease |
| Previous history of VT/VF/cardiac arrest | Known history of congestive cardiac failure |
| Examination findings | |
| Systolic heart murmur heard | >20 mm Hg drop on standing |
| Signs of heart failure present | Diastolic heart murmur heard |
| Systolic BP <90 mm Hg | Ventricular pause >3 s on carotid sinus massage |
| Suspicion of pulmonary embolism | Trauma associated with collapse |
| AAA detected | |
| New neurological signs on examination | |
| Suspicion of CVA or SAH | |
| FOB present on PR | |
| Other suspicions of GI bleed | |
| ECG findings | |
| Mobitz type II heart block | Right bundle branch block |
| Wenkebach heart block | QRS duration >120ms |
| Bifascicular block | Old T wave/ST segment changes |
| Complete heart block | Frequent pre‐excited QRC complexes |
| Sinus pause >3 s | Q waves unchanged from old ECG |
| New ST elevation ventricular tachycardia | Atrial fibrillation or flutter |
| Sinus bradycardia <50 | PR >200 ms (first‐degree heart block) |
| Sinoatrial block | |
| QTc >450 ms | Low risk (consider discharge) |
| NEW T wave/ST segment changes | None of the above characteristics |
| Brugadas (ST segment elevation V1–V3) | |
| Arrhythmogenic right ventricular dysplasia |
AAA, abdominal aortic aneurysm; BP, blood pressure; CVA, cerebrovascular accident; FOB, faecal occult blood; GI, gastrointestinal; PR, rectal examination; SAH, subarachnoid haemorrhage; VF, ventricular fibrillation; VT, ventricular tachycardia.
Methods
Setting
The ED of the Royal Infirmary of Edinburgh, UK (85 000 adult attendances per annum).
Inclusion criteria
All patients presenting with syncope aged ⩾16 years between 7 November 2005 and 7 February 2006 were prospectively enrolled into the study.
Exclusion criteria
Patients aged <16 years, those previously recruited and those with a history of seizure with prolonged post‐ictal phase were excluded. Patients who were unable to give either written or verbal informed consent were also excluded.
Enrolment into study
ED nurses identified potentially eligible patients and a data collection form was placed with the patient's records. The treating doctor was responsible for deciding whether the patient had had an episode of syncope after the initial assessment. All doctors involved in the study had undergone a 15‐min training session on criteria associated with a diagnosis of syncope. A decision to enrol a patient was not overturned later by the study team and enrolled patients were analysed on an intention‐to‐treat basis. The study team reviewed the notes of any patient who had been initially flagged by the triage nurse, but later rejected by the doctor. Only nine patients were rejected in this manner. Reasons for the doctor rejecting a patient were inability to obtain consent, patients being found collapsed for an unknown period of time or patients presenting with a likely seizure.
Assessment
All patients underwent a standardised assessment using 31 predetermined variables (11 focused on clinical features, 9 on medical history and 11 on current medication), 28 examination variables and 26 ECG variables. These were selected after careful systematic review of the literature to identify characteristics previously shown to be associated with serious outcome. After a full history and examination, all patients underwent a 12‐lead ECG, lying and standing blood pressures were recorded and a “BM stix” glucose estimation. Patients who were at medium or high risk according to our ED's existing syncope guidelines also had full blood count, urea, creatinine, glucose, electrolytes and C reactive protein measured. Patients still in the ED at 12 h were defined as admitted. Patients were admitted, referred to medical outpatient departments or discharged according to our ED's existing syncope guidelines, and a study information form was completed. Patients admitted to the hospital or who attended the medical outpatient department underwent evaluations for any clinical or historical findings suggestive of a cause of syncope at the discretion of the treating consultant, including 24‐h ECG tape and echocardiography investigations.
Endpoint measures
Primary end point was a serious outcome at 1 week, 1 month and 3 months. Serious outcomes were predefined and were all‐cause death, acute myocardial infarction (history of chest pain or ECG changes and troponin I >2), life‐threatening arrhythmia (documented on monitor or ECG during inpatient stay or on outpatient Holter monitoring and requiring treatment), pulmonary embolus (confirmed on ventilation perfusion lung scan/CT pulmonary angiography and requiring treatment), cerebrovascular accident/subarachnoid haemorrhage (CT or lumbar puncture diagnosis), haemorrhage requiring a blood transfusion of two units or more during inpatient stay and an acute surgical procedure or endoscopic intervention secondary to a suspected cause of syncope.
Once 3 months had elapsed after ED attendance for all patients, the hospital computer system was interrogated to see whether the patients had returned to any hospital in the Lothian region. The hospital records were acquired and scrutinised for all patients who had attended the ED or outpatient department or who had been admitted as inpatients. All deceased patients were identified via the hospital computer system, which is directly linked with the national death register and primary care patient records. Hospital notes were scrutinised to determine whether each patient with syncope had had a serious outcome within 3 months of their attendance to the ED. All patients could be followed up, and all hospital notes and records could be traced. For any patient residing outside the Lothian region, either their general practitioner or the patient was contacted.
The presence or absence of an SFSR high‐risk factor and the patient's OESIL score was determined by the study team from specifically prospectively acquired information on the data collection form. The OESIL score is based on four characteristics: age >65 years, a clinical history of cardiovascular disease, syncope without prodromal symptoms and an abnormal ECG. The presence of each characteristic scores one. One‐year mortality has been shown to increase with increasing score.13 The SFSR defines high‐risk patients as those having any one of the five risk factors: abnormal ECG (non‐sinus rhythm or new abnormality), anaemia (haematocrit <30%), a complaint of shortness of breath, systolic hypotension (<90 mm Hg) and a history of congestive cardiac failure.15,16 The patient's ED guideline risk group (high, medium and low) was determined by the study doctor after an initial assessment.
Review of missed patients
To determine the recruitment rate of patients into the study, a retrospective search of all ED electronic patient records (EPRs) between 7 November 2005 and 7 February 2006 was conducted looking for the keywords “syncope”, “collapse”, “faint”, “loss of consciousness” or “loc” appearing anywhere on the EPR. All EPRs with one of these terms were then hand searched and a decision was made from the notes whether the patient fitted the study's inclusion criteria. A list was compiled of all patients who fitted the study inclusion criteria, along with their demographic details, and compared using Chi‐squared and Mann‐Whithey U tests with those patients who had been enrolled into the study.
Statistical analysis
All patient data were entered into a specially designed Microsoft Access database and exported into Excel for statistical analysis. A power calculation was not performed for the pilot study; however, it was decided that 100 patients would be sufficient for the primary aim. Sensitivity, specificity, predictive values and likelihood ratios were calculated for existing CDRs, current ED guidelines and some selected patient characteristics, and serious and non‐serious outcome groups were compared using Fisher's exact test (table 2).
Table 2 Sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, negative likelihood ratio and p value of emergency department guidelines, Osservatorio Epidemiologico sulla Sincope nel Lazio Score, San Francisco Syncope Rule and some selected characteristics.
| PPV | NPV | Sensitivity | Specificity | PLR | NLR | p Value | |
|---|---|---|---|---|---|---|---|
| High‐risk group (based on ED guidelines) | 0.219 | 0.940 | 0.636 | 0.716 | 2.239 | 0.508 | 0.035* |
| High‐ or medium‐risk group (based on ED guidelines) | 0.133 | 1.000 | 1.000 | 0.182 | 1.222 | 0 | 0.203 |
| One of SFSR risk factors present | 0.186 | 1 | 1 | 0.455 | 1.835 | 0.000 | 0.006* |
| OESIL >0 | 0.124 | 1.000 | 1.000 | 0.114 | 1.128 | 0.000 | 0.597 |
| OESIL >1 | 0.182 | 0.977 | 0.909 | 0.489 | 1.778 | 0.186 | 0.011* |
| OESIL >2 | 0.267 | 0.957 | 0.727 | 0.750 | 2.909 | 0.364 | 0.003* |
| OESIL >3 | 0.375 | 0.912 | 0.273 | 0.943 | 4.800 | 0.771 | 0.426 |
| Abnormal ECG | 0.158 | 0.952 | 0.818 | 0.455 | 1.500 | 0.400 | 0.111 |
| History of CV disease | 0.222 | 0.931 | 0.545 | 0.761 | 2.286 | 0.597 | 0.065 |
| Age >65 years | 0.190 | 1 | 1 | 0.466 | 1.872 | 0 | 0.002* |
| History of CCF | 0.500 | 0.897 | 0.091 | 0.989 | 8 | 0.920 | 0.211 |
CCF, congestive cardiac failure; CV, cardiovascular; ED, emergency department; Hx, history; NLR, negative likelihood ratio; NPV, negative predictive value; OESIL, Osservatorio Epidemiologico sulla Sincope nel Lazio; PLR, positive likelihood ratio; PPV, positive predictive value; SFSR, San Francisco Syncope Rule.
*Significant at the 5% level, Fisher's exact test.
Results
Ninety‐nine consecutive adult patients were recruited over a 3‐month period between 7 November 2005 and 7 February 2006. It was thought that 100 patients had been enrolled; however, one patient episode had been erroneously duplicated during data entry. In all, 44 patients were admitted to the hospital and 55 were discharged from the ED. Of the 11 patients with a serious outcome, 8 had developed this by 7 days and 3 further patients had developed a serious outcome by 3 months. In all, therefore, 11 patients had a serious outcome by 3 months. Of these, five patients died and six had an alternative serious outcome. All 11 had been admitted to hospital from the ED. The percentage risk of serious outcome at 7 days, 1 month and 3 months was 8.1%, 8.1% and 11.1%, respectively.
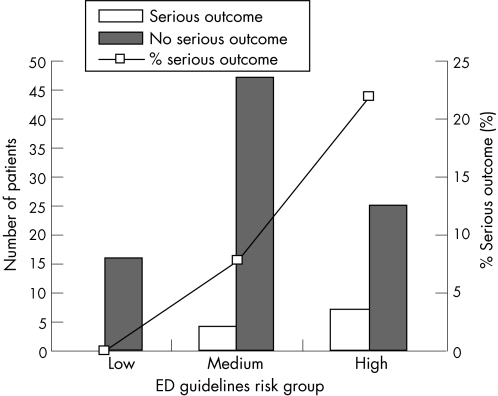
Current ED guidelines
In all, 32 patients were at high risk, 51 at medium risk and 16 at low risk according to our existing ED guidelines. Of the patients with a serious outcome, seven were at high risk, four were at medium risk and none was at low risk. A total of 7 of 32 (22%) high‐risk patients, 4 of 51 (8%) medium‐risk patients and 0 of 16 (0%) low‐risk patients had a serious outcome (fig 1). In all, 19 of the 51 medium‐risk patients were admitted to hospital and no patient with a subsequent serious outcome was discharged directly from the ED. Admission of all high‐risk patients only (by ED guidelines) would have led to 12 fewer admissions; however, 4 patients with serious outcomes would have been discharged. Admission of all medium‐ and high‐risk patients only would have led to 39 further admissions but would have detected all patients with serious outcomes.
Figure 1 The number of patients from each emergency department (ED) guidelines risk group for serious and not serious 3‐month outcomes, and percentage of serious outcome for each ED guidelines risk group.
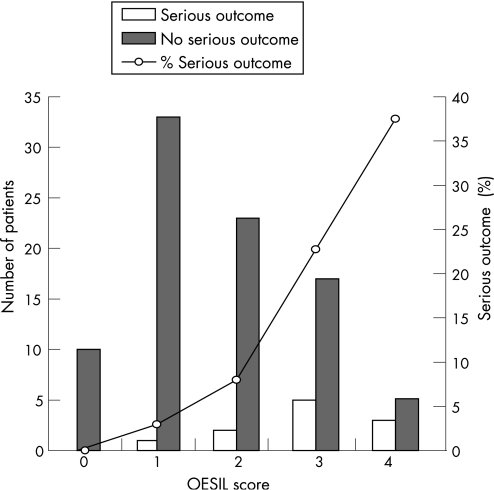
OESIL score
A total of 10 patients had an OESIL score of 0 (no serious outcomes), 34 had an OESIL score of 1 (1 serious outcome), 25 had an OESIL score of 2 (2 serious outcomes), 22 had an OESIL score of 3 (5 serious outcomes) and 8 patients had an OESIL score of 4, of which 3 had a serious outcome (fig 2).
Figure 2 Graph showing number of patients with each Osservatorio Epidemiologico sulla Sincope nel Lazio (OESIL) score for serious and not serious 3‐month outcomes, and percentage of serious outcome for each OESIL score.
Percentages of serious outcomes were 0%, 2.9%, 8%, 22.7% and 37.5% for OESIL scores of 0, 1, 2, 3 and 4, respectively (fig 2). This compares with 0%, 0.8%, 19.6%, 34.7% and 57.1% for 12‐month mortality in Colivicchi et al's13 paper. Use of the OESIL score with a cut‐off for admission of an >0 instead of existing guidelines would have led to 55 further admissions, with no patients having serious outcomes being discharged. An OESIL score >1 would have led to 11 further admissions, with 1 patient having a serious outcome being discharged. An OESIL score >2 would have led to 14 fewer admissions, with 3 patients having serious outcomes being discharged and an OESIL score >3 would have led to 36 fewer admissions, with 8 patients having serious outcomes being discharged.
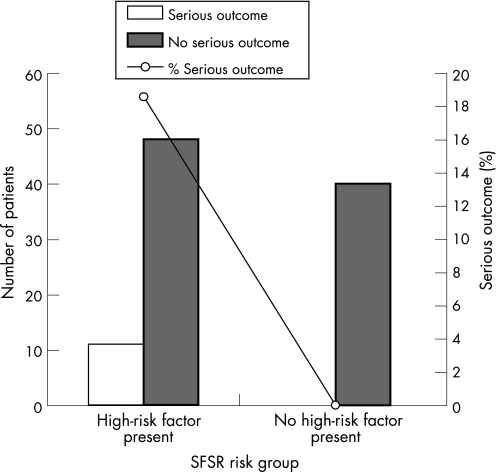
San Francisco Syncope Rule
A total of 40 patients had none of the 5 SFSR risk factors (with no serious outcomes = 0%) and 59 patients had an SFSR high‐risk factor present (11 serious outcomes = 18.6%; fig 3). Use of the SFSR instead of existing guidelines would have led to 15 further admissions, with no improvement in sensitivity on current practice in our ED.
Figure 3 The number of patients with each San Francisco Syncope Rule (SFSR) risk group for serious and not serious 3‐month outcomes, and percentage of serious outcome for each SFSR risk group.
Study pick‐up rate and comparison of study group and “missed” group
A total of 263 patients presenting between 7 November 2005 and 7 February 2006 were identified from the EPR search as fitting the study's inclusion criteria. The study therefore managed to pick up 37.6% of patients eligible for inclusion. There were 74 men (45%) and 90 women in the “missed group” compared with 48 men (48%) and 51 women in the “study group” (p = 0.6, NS, χ2 test). Neither the ages of the study group nor of the missed group were normally distributed. The median age of the study group was 71 years (interquartile range (IQR) 47–81) and that of the missed group was 62.5 years (IQR 29–78; p = 0.047, significant at the 5% level, Mann–Whitney U test).
Discussion
This study was conducted as a pilot for the ROSE study. It is the first prospective study on syncope within UK ED practice and the first attempt to evaluate existing clinical decision rules in the UK. The primary aim of the study was to assess the process of patient recruitment and to test the study method and feasibility of data collection before the main ROSE study.
A power calculation was not performed before the pilot, and we acknowledge that the study did not enrol a cohort of patients large enough to derive a clinical decision rule, one of the aims of the main ROSE study. The secondary aim of the study was to compare the performance of our current ED guidelines with the OESIL score and the SFSR at predicting short‐ and medium‐term serious outcomes. Again, because of the small size of the study, we have only conducted a statistical analysis of serious outcome at 3 months. The findings of this pilot study, although requiring cautious interpretation, are important.
This study only recruited 37.6% of eligible patients. Conducting ED research such as this is difficult; however, the recruitment rate will need to be improved for the main study. Closer analysis reveals that the “missed” group had a lower median age than the “study” group and that the distribution of risk groups in the “study” group is skewed towards the more serious end of the scale. This suggests that the treating doctors were not enrolling younger patients with simple low‐risk vasovagal faints. This has probably led to a higher serious outcome rate. If this is repeated in the main study, it may mean that any derived clinical rule may not be applicable to this group, albeit a low‐risk one. This problem must therefore be addressed in the main study by further training of recruiters and an improved method of picking up all eligible patients.
Using a 7‐day event rate of 10%, a power calculation performed to determine sample size requirements for a large prospective derivation and a validation study suggested that 500 patients would need to be recruited into a derivation cohort and 500 into a validation cohort. With improvements in our recruitment processes, we estimate that this is feasible over 2 years.
There are few studies on syncope based on in UK EDs. In 1999 Thakore et al17 looked at practice in one UK ED and showed that few patients had relevant syncope symptoms documented or an ECG recorded. In all, 28% of patients with an abnormal ECG and 40% with a history of organic heart disease were sent home from the ED. Prior to our study, the only UK ED study of syncope outcome was conducted by Crane.18 This retrospective study of 210 patients presenting during an 8‐week period showed that it was possible to stratify UK ED patients with syncope according to ACP guidelines.6,7 Patients in ACP group 1 (high risk) had a 1‐year mortality of 36%, compared with patients assigned to ACP group 2 (intermediate risk; 14%) and to ACP group 3 (low risk; 0%). Our study confirms the findings of Crane, showing that our ED guidelines (based on the European Society of Cardiology,9,10 ACP6,7 and the American College of Emergency Physician guidelines8) can successfully risk stratify UK ED patients with syncope.
Following our existing ED guidelines and making a decision to admit a high‐risk patient with a “high‐risk” factor led to a reasonable sensitivity (0.636) and good specificity (0.716) for serious outcome. Considering admission for all medium‐ and high‐risk patients ensures that no serious outcomes are missed; however, this would lead to a large increase in admissions for only a small increase in the detection of patients with serious outcomes. Despite our guidelines suggesting that medium‐risk patients could be considered for discharge to outpatient review, 19 of the 51 medium‐risk patients were admitted to hospital and no patients with serious outcomes were discharged. This suggests that the doctor's judgement may have played an important part in deciding which medium‐risk patients may have been at increased risk. If they have not already, all UK EDs should have similar guidelines in place in order to effectively risk stratify patients presenting with syncope.
The OESIL score was originally derived and validated to predict 12‐month all‐cause mortality. It differs from the SFSR in that the original study demonstrated that an increasing OESIL score is associated with an increased risk of a serious outcome, whereas the SFSR relies only on the presence of one of five high‐risk factors. Our study findings are similar to those of the original study; however, where to place the cut‐off for admission to hospital is unclear and was not defined in the original study. Admitting patients who have an OESIL score >1 has the required sensitivity, but would have led to 11 more admissions. Setting a higher cut‐off is associated with an improved specificity at the expense of a reduced sensitivity.
The SFSR was originally devised to predict a 7‐day serious outcome. Again, our study findings are similar to the results of the original study, the SFSR showing a sensitivity of 1 and a specificity of 0.455. Adopting this rule, however, would have led to 15 more admissions with the detection of no more serious outcomes. This suggests that although the SFSR may be a sensitive tool in the UK ED population, its use would increase admissions with only a small increase in the detection of patients with serious outcome. It is interesting that the OESIL risk factor “age >65” alone performs better than both the SFSR and our existing ED guidelines.
Clearly, there is a need for a large prospective study of syncope in the UK ED population. Existing CDRs show some promise; however, there is room to improve these tools. There are large differences in practice and admission policies between UK and North American EDs and therefore there is a definite need to derive and validate a more useful tool for use in the UK population. Despite this being costly and time consuming its potential benefits are many, including reducing unwarranted admissions, improving patient outcome and satisfaction and allowing resources to be concentrated on patients most at risk of adverse events.
Conclusion
This pilot demonstrates that a study to derive and validate an ED syncope stratification rule is feasible. The pilot also enabled the study method and data collection process to be assessed and revised before starting the main ROSE study.
This study has evaluated the OESIL score, the SFSR and our existing ED guidelines, and has shown that each is able to identify an increased probability of medium‐term serious outcome in patients with syncope despite the OESIL score being initially derived and validated for long‐term prediction and the SFSR for short‐term outcome. The SFSR shows good sensitivity at the expense of an increase in admissions to hospital; however, our existing ED syncope guidelines and the OESIL score, although being able to successfully risk stratify patients, are not sufficiently sensitive to be able to reduce admissions without missing patients who later go on to develop a serious outcome.
Undoubtedly, there is a need for a simple UK‐derived clinical decision rule for patients presenting with syncope to enable safe, effective clinical care and to aid less experienced decision makers.
Acknowledgements
We thank Ina Sutherland in medical records and the medical and nursing staff in the Edinburgh Royal Infirmary Emergency Department.
Abbreviations
ACP - American College of Physicians
CDR - clinical decision rule
ED - emergency department
EPR - electronic patient record
ROSE - Risk stratification Of Syncope in the Emergency department
OESIL - Osservatorio Epidemiologico sulla Sincope nel Lazio
SFSR - San Francisco Syncope Rule
Footnotes
Competing interests: None declared.
References
- 1.Morag R. Syncope. In: Peak DA, Talavera F, Halamka J, et al eds. eMedicine on line emergency textbook. http://www.emedicine.com/emerg/topic876.htm (accessed 3 Feb 2007)
- 2.Maisel W H, Stevenson W G. Syncope: getting to the heart of the matter. N Engl J Med 2002347931–933. [DOI] [PubMed] [Google Scholar]
- 3.Soteriades E S, Evans J C, Larson M G.et al Incidence and prognosis of syncope. N Engl J Med 2002347878–885. [DOI] [PubMed] [Google Scholar]
- 4.Kapoor W N, Karpf M, Wieand S.et al A prospective evaluation and follow‐up of patients with syncope. N Engl J Med 1983309197–204. [DOI] [PubMed] [Google Scholar]
- 5.Kapoor W N, Hanasu B H. Is syncope a risk factor for poor outcomes? Comparison of patients with and without syncope. Am J Med 1996100646–655. [DOI] [PubMed] [Google Scholar]
- 6.Linzer M, Yang E H, Estes N A., IIIet al Diagnosing syncope. 1. Value of history, physical examination, and electrocardiography: Clinical Efficacy Assessment Project of the American College of Physicians, Ann Intern Med 1997126989–996. [DOI] [PubMed] [Google Scholar]
- 7.Linzer M, Yang E H, Estes NA I I I.et al Diagnosing syncope. 2. Unexplained syncope: Clinical Efficacy Assessment Project of the American College of Physicians, Ann Intern Med 199712776–86. [DOI] [PubMed] [Google Scholar]
- 8.Molzen G W, Suter R E, Whitson R. American College of Emergency Physicians: clinical policy: critical issues in the evaluation and management of patients presenting with syncope. Ann Emerg Med 200137771–776. [DOI] [PubMed] [Google Scholar]
- 9.Brignole M, Alboni P, Benditt D G.et al Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope—update 2004. Executive summary. Eur Heart J 2004252054–2072. [DOI] [PubMed] [Google Scholar]
- 10.Brignole M, Alboni P, Benditt D.et al Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001221256–1306. [DOI] [PubMed] [Google Scholar]
- 11.Martin G J, Adams S L, Martin H G.et al Prospective evaluation of syncope. Ann Emerg Med 198413499–504. [DOI] [PubMed] [Google Scholar]
- 12.Oh J H, Hanusa B H, Kapoor W N.et al Do symptoms predict cardiac arrhythmias and mortality in patients with syncope? Arch Intern Med 1999159375–380. [DOI] [PubMed] [Google Scholar]
- 13.Colivicchi F, Ammirati F, Melina D.et al Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J 200324811–819. [DOI] [PubMed] [Google Scholar]
- 14.Sarasin F P, Hanusa B H, Perneger T.et al A risk score to predict arrhythmias in patients with unexplained syncope. Acad Emerg Med 2003101312–1317. [DOI] [PubMed] [Google Scholar]
- 15.Quinn J V, Stiell I G, McDermott D A.et al Derivation of the San Francisco Syncope Rule to predict patients with short‐term serious outcomes. Ann Emerg Med 200443224–232. [DOI] [PubMed] [Google Scholar]
- 16.Quinn J V, McDermott D A, Stiell I G.et al Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Ann Emerg Med 200647448–453. [DOI] [PubMed] [Google Scholar]
- 17.Thakore S B, Crombie I, Johnston M. The management of syncope in a British emergency department compared to recent American guidelines. Scott Med J 199944155–157. [DOI] [PubMed] [Google Scholar]
- 18.Crane S D. Risk stratification of patients with syncope in an accident and emergency department. Emerg Med J 20021923–27. [DOI] [PMC free article] [PubMed] [Google Scholar]