Abstract
Gastric volvulus is a rare disease with an unknown incidence. Unless it stays in the back of the diagnostician's mind, diagnosis of gastric volvulus, which can have significant morbidity and mortality associated with it, can be easily missed. Unstable vital signs and distressed appearance are not always present, as in textbook cases. The presence of a hiatal hernia with persistent vomiting despite initial antiemetic treatment should trigger one to think of gastric volvulus, despite the patient appearing very stable. With the advent of CT and laparoscopic surgery, the gold standards for diagnosing and treating this disease are ever evolving.
Case presentation
An 82‐year‐old female with a history of hiatal hernia, peptic ulcer disease and asthma presented to the emergency department with an acute onset of sharp epigastric pain for 4–5 h without radiation, which was associated with nausea and emesis. Emesis was non‐bilious and non‐bloody. The pain and emesis were temporally concurrent.
On review of systems, she denied any diaphoresis, shortness of breath, constipation, diarrhoea, previous similar episodes, and use of non‐steroidal anti‐inflammatory drugs and alcohol. Surgical history included laparoscopic cholecystectomy.
On physical examination, she was found to be afebrile, with stable vital signs. She was in mild distress, spitting into a wash basin. Abdominal examination revealed mild epigastric tenderness with normal active bowel sounds. No peritoneal signs were noted.
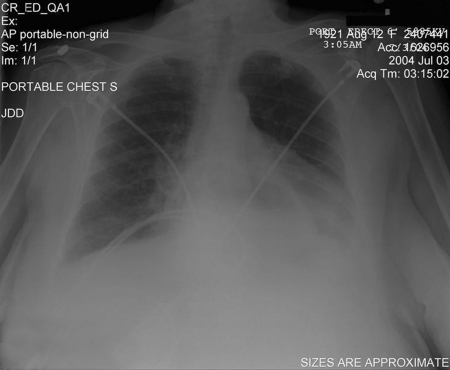
Electrocardiography revealed a normal sinus rhythm, and a chest x ray examination showed a large hiatal hernia (fig 1). Laboratory testing revealed only a mildly elevated white cell count of 13.4×109/l.
Figure 1 Chest radiograph showing a large hiatal hernia.
While in the emergency department, she received antiemetic medications with minimal relief. Use of a nasogastric tube (NGT) alleviated some of the symptoms; however, she continues to have persistent nausea. The NGT suctioned out 200 ml of clear, non‐bilious fluid. Her vital signs remained stable and within normal limits during her stay in the emergency room.
At that time, a small bowel follow‐through barium study was ordered, which revealed a large gastric volvulus. She was taken to the operating room for surgical repair of the volvulus and the hiatal hernia. A Nissen fundoplication and an anterior gastropexy were performed. The patient recovered without any complications, and was discharged to a rehabilitation facility.
Discussion
Gastric volvulus is a rare entity that can be elusive to diagnose. The incidence is unknown, due to the existence of a chronic form of gastric volvuli. The peak age group of incidence is in the fifth decade, with equal frequencies between the sexes and across all races. Acute gastric volvuli carry a mortality rate of 42–56%, secondary to gastric ischaemia, perforation or necrosis.1
Classically, Borchardt's triad of vomiting, epigastric pain and an inability to pass an NGT should trigger one to think of gastric volvulus as the primary diagnosis. Borchardt's triad has been reported to occur in 70% of cases.2 However, a retrospective study on the common presentations of chronic gastric volvulus over a 5‐year period has shown that dysphagia, epigastric pain and chest pain occur 29% of the time individually.3
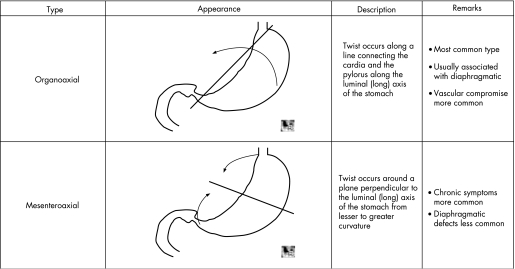
Symptoms are brought on by the rotation of the stomach by more than 180°. Rotation of the stomach along the long axis extending from the gastro‐oesophageal junction to the pylorus is termed mesenteroaxial rotation. Organoaxial gastric volvulus results from the rotation of the stomach around the axis that bisects the lesser and greater curvatures of the stomach (table 1).4 The organoaxial type constitutes about 59% of all gastric volvulus, whereas 29% are mesenteroaxial (fig 2). The remaining 12% are a mixture of both.5
Figure 2 Organoaxial and mesenteroaxial rotation. Reproduced with permission from 2004 Learning Radiology.com
The aetiology of the rotation is either primary or secondary. “Primary” refers to the absence of diaphragmatic defects or intra‐abdominal abnormality causing the volvulus. Laxity of the ligaments which anchors the stomach in place within the abdominal cavity, is a common cause. Lengthening of the ligaments due to stretching gives rise to abnormal rotation of the mesentery. In 30% of gastric volvuli, there is a primary cause.6 Secondary gastric volvuli have alternative causes, including congenital or traumatic diaphragmatic hernias, hiatal hernias, eventration of the diaphragm, abdominal bands or adhesions.7 A retrospective analysis in 2004 found that seven out of eight patients with the diagnosis of gastric volvulus at the Kasturba Medical College Hospital, Manipal, South India, between 1986 and 2000 have a secondary cause, including eventration of the diaphragm, Bockdalek hernia and incisional hernias.5 However, a study in 2000 with significantly more subjects found that the most common predisposing factor is a paraoesophageal hiatal hernia (28/36).8
Diagnosing a gastric volvulus is difficult, since there is no one lab value/set of lab values sensitive enough to exclude the diagnosis. The gold standard is a barium swallow, which has a very high sensitivity and specificity for diagnosing a gastric volvulus. A recent study showed that a barium swallow is diagnostic in 14 out of 25 cases and suggestive in an additional 7 out of 25 cases.7 However, there are case reports that advocate the use of abdominal CT, since it can give information about the position and anatomy necessary to hasten surgical intervention.9 Additionally, CTs can be performed in a non‐responsive patient who presents in a stable but critical status.9,10
Treatment can be either surgical or medical in nature. Conservative management consists of endoscopic reduction or percutaneous endoscopic gastrostomy. The risk of gastric perforation is significant in conservative treatment. Therefore, patients should be considered carefully for conservative treatment. The gold standard is open laparotomy with detorsion and prevention with anterior gastropexy. Nissen fundoplication decreases future occurrences in patients with a hiatal hernia.6
In summary, unless it stays in the back of the diagnostician's mind, gastric volvulus can be an easily missed diagnosis, which is associated with significant morbidity and mortality. As mentioned above, patients do not always exhibit unstable vital signs and distressed appearance. The presence of a hiatal hernia with persistent vomiting despite initial antiemetic treatment should trigger one to think of gastric volvulus. With the advent of CT and laparoscopic surgery, the gold standards for diagnosing and treating this disease are ever evolving.
Abbreviations
NGT - nasogastric tube
Footnotes
Competing interests: None declared.
References
- 1.Green J Gastric volvulus. Emedicine 2004. Available at http://www.imedicine.com.online.uchc.edu/DisplayTopic.asp?bookid = 12&topic = 296
- 2.Akoad M Gastric volvulus. Emedicine. 2002. http://www.imedicine.com.online.uchc.edu/DisplayTopic.asp?bookid = 6&topic = 2714 (accessed 16 March 2007)
- 3.Cozart J C, Clouse R E. Gastric volvulus as a cause of intermittent dysphagia. Dig Dis Sci 1998431057–1060. [DOI] [PubMed] [Google Scholar]
- 4. http://www.LearningRadiology.com
- 5.Willsher P C, White R C, Dumbrell P. Idiopathic chronic gastric volvulus. Aust NZ J Surg 199666647–649. [PubMed] [Google Scholar]
- 6.Machado N O, Rao B A. Gastric volvulus with identifiable cause in adults. Presentation and management. Saudi Medl J 2004252032–2034. [PubMed] [Google Scholar]
- 7.Kohli A, Vij A, Azad T. Intrathoracic gastric volvulus‐acute and chronic presentation. J Indian Med Assoc 199795522–523. [PubMed] [Google Scholar]
- 8.Teague W J, Ackroyd R, Watson D I.et al Changing patterns in the management of gastric volvulus over 14 years. Br J Surg 200087358–361. [DOI] [PubMed] [Google Scholar]
- 9.Coulier B, Ramboux A. Acute obstructive gastric volvulus diagnosed by helical CT. Jbr‐Brt Organe Soc R Belge Radiol 20028543. [PubMed] [Google Scholar]
- 10.Cherukupalli C, Khaneja S, Bankulia P.et al CT diagnosis of acute gastric volvulus. Dig Surg 200320497–499. [DOI] [PubMed] [Google Scholar]