Abstract
Objective
To investigate the accuracy of assessment of burn surface area and depth using a basic camera‐equipped mobile phone.
Methods
31 patients with minor burns were assessed at the Welsh Centre for Burns & Plastic Surgery.
Results
A high correlation was found between assessment of burn surface area and burn depth using a camera mobile phone compared with a live assessment.
Conclusion
There are a number of implications for the use of mobile phone technology in hospitals and its potential use in the management of major in addition to minor burns, as well as other forms of trauma. The untapped potential for this technology in a hospital environment is highlighted.
Use of mobile phones in hospitals has been controversial, with restrictions on their use being widespread. These restrictions are founded on a small evidence base as recently reported,1 and any risks appear small, leading to widespread disregard of these restrictions by some patients and staff. There are also suggestions that there should be greater restrictions on camera phones. This has led to minimal research on the potential clinical applications of mobile phones, the technology for which is becoming increasingly sophisticated.
A camera mobile phone has the prerequisites for a complete telemedicine system, with the potential capability to enable assessment of both total burn surface area (TBSA) and burn depth (fig 1). These prerequisites include the ability to capture an image, store it temporarily, transmit this image to a remote location, and view this image without loss of resolution. Teledermatology for the diagnosis and treatment of skin conditions is already routine practice in some centres, but is expensive.2 The benefits of mobile phones for this purpose over and above other methods of data transmission are significant. Traditional telemedicine equipment is very costly, requires major infrastructure in two locations, requires training, and is unavailable in most hospitals. The main alternative includes email or computer‐based data transmission. However, this also requires significant infrastructure at both ends requiring the following steps:
Figure 1 A partial thickness burn captured on the camera phone used for this study.
Image capture (for example, digital camera)
Transfer of image onto computer (cable or possibly wireless transmission)
Processing of image by software program to reduce file size (and image quality) to allow email transmission
Sending of email
Receipt and viewing of email at remote location
The above system is limited by infrastructure such as possession of a computer, of a broadband or other high speed internet connection, and of a digital camera. It would be difficult to contemplate its use in remote areas or war zone scenarios.
The advantage of a mobile phone is that image capture, transmission and receipt can be done very quickly without loss of image resolution, independent of major infrastructure at either end, and to any location within range of a mobile phone signal.
The major important factors when assessing isolated burn injuries relate to the burn site, the burn size (TBSA), and the burn depth. A number of important management decisions are based upon these factors, including whether transfer to a burn centre is indicated,3 what fluid resuscitation is required, whether surgery is indicated, and what dressings might be most appropriate. The experience of burns surgeons is that the TBSA in particular, as well as the depth of burn, is often inaccurately assessed at primary presentation. As burn care becomes concentrated into large centres, receiving centres are often a long distance from a referring unit. The need for accurate initial assessment is therefore important because an under‐ or overestimate of the injury area or depth can lead to inappropriate fluid resuscitation for prolonged periods of time or to unnecessary transfer of patients.
We undertook this study to see the feasibility and practicality of using a camera mobile phone to assess burns, and to provide a baseline in relation to future advances in the technology both for burn care and for hospital practice in general.
Methods
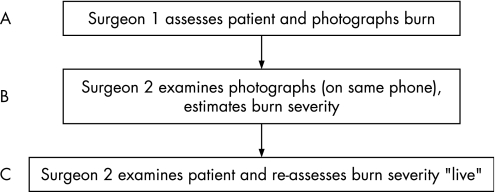
Thirty‐one consecutive patients at the Welsh Burns Centre with minor burns (<10% TBSA) were assessed. All injuries were sustained within 48 h of assessment. All burn injuries at the Welsh Burn Centre are routinely photographed. Parallel with routine digital photography of the burn injuries, photographs were also taken with the camera phone following detailed explanation of the nature of the study and written consent. This was a 1 mega‐pixel Nokia 7610 mobile phone with a thin film transistor screen size of 35×41 mm (176×208 pixels), displaying 65 000 colours. The photographing surgeon also undertook a live assessment of the depth and TBSA of the burn. A second surgeon then documented estimated %TBSA and depth of burn, first from the images on the (same) phone, and then from a live assessment (fig 2). As digital transmission of image data does not lead to degradation of image quality, it was unnecessary for the purposes of this study to actually transmit any data, and instead the same phone was used to simulate the transmitting phone as well as the “receiving” phone. After assessment, images were deleted. Correlation coefficients were then calculated comparing the accuracy of estimated TBSA and burn depth from the images compared to the live assessments.
Figure 2 Schematic to show method of live and photographic assessments of patients. Data analysis assessed correlation between A and B and B and C.
Results
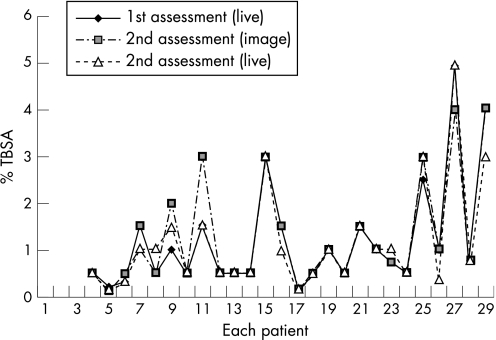
The range of TBSA was 0.1–5.0% (mean 1.2%). There was a strong correlation with the %TBSA assessed using the camera phone images compared with live assessments either by the same assessor (correlation coefficient r = 0.92) or a different assessor (r = 0.91) (fig 3). Using the images, assessors could reliably differentiate full thickness burns from partial thickness burns in almost all cases (94%, n = 29).
Figure 3 Graphical representation of the differences in % total burn surface area (TBSA) as assessed using live and camera phone assessments.
Discussion
When this study commenced, a 1 mega‐pixel camera integrated into a mobile phone was state of the art. By the time of going to press a 5 mega‐pixel camera phone is readily available in the shops. The technological growth in this area is extremely rapid, sophisticated and powerful and yet its potential applications in healthcare remain untapped. Radiographs and images of traumatic injuries have previously been transmitted and interpreted through use of mobile phones,4,5,6 and we illustrate the utility of these devices in the assessment of burns. Within minutes, an emergency department hours away from a burns centre can transmit accurate images to that centre, enabling decisions to be made related to appropriateness of transfer, interim dressings and fluid resuscitation, with profound implications for the quality of patient care as well as cost. This is especially pertinent with the knowledge that emergency departments often miscalculate the TBSA by up to 100%, with greater errors in small burns7 using the common methods such as the rule of nines or Lund and Browder Charts.8
We suggest it is the responsibility of the regulators to draw up both legal and clinical regulatory frameworks to ensure that false assumptions with regards to clinical risk or confidentiality issues do not prevent the assessment and use of increasingly sophisticated mobile phone technology in hospitals for the benefit of patients and healthcare staff.
Conclusions
Camera phones appear to be reliable for the assessment of TBSA and burn depth in minor burns. Although not assessed directly in this study, it is likely that major burns can also be estimated successfully in this way. When used for this purpose, the quality (size and resolution) of the display is as important as the camera resolution. For larger burns, more than one image would be required which may make estimation slightly more difficult, and incorporating the patients' hand into the image can help with assessing proportion. The medico‐legal and confidentiality issues related to image capture and data transfer of this kind need to be addressed in a constructive way to enable integration of this useful tool into clinical practice. Simple precautions are advised when using this technology:
Obtain consent for photography and storage of this image (a standard National Health Service photography request should cover this)
Anonymity of the images
A “unit” phone rather than a personal phone may be more appropriate in the receiving unit.
As this technology develops there may be a role to help decision making between receiving units remote from definitive burn centres.
Footnotes
Conflicts of interest: none
References
- 1.Derbyshire S W G, Burgess A. Use of mobile phones in hospitals. New guidelines are less restrictive but still overcautious. BMJ 2006333767–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wootton R, Bloomer S E, Corbett R.et al Multicentre randomised control trial comparing real time teledermatology with conventional outpatient dermatological care: societal cost‐benefit analysis. BMJ 20003201252–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Burn Care Review National burn injury referral guidelines. In: Standards and strategy for burn care. London: NBCR, 200168–69.
- 4.Lam T K, Preketes A, Gates R. Mobile phone photo messaging assisted communication in the assessment of hand trauma. ANZ J Surg 200474598–602. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh C H, Tsai H H, Yin J W.et al Teleconsultation with the mobile camera‐phone in digital soft‐tissue injury: a feasibility study. Plast Reconstr Surg 20041141776–1782. [DOI] [PubMed] [Google Scholar]
- 6.Archbold H A, Guha A R, Shyamsundar S.et al The use of multi‐media messaging in the referral of musculoskeletal limb injuries to a tertiary trauma unit using: a 1‐month evaluation. Injury 200536560–566. [DOI] [PubMed] [Google Scholar]
- 7.Hammond J S, Ward C G. Transfers from emergency room to burn center: errors in burn size estimate. J Trauma 1987271161–1165. [DOI] [PubMed] [Google Scholar]
- 8.Benson A, Dickson W A, Boyce D. In: Harding K, Grey J, eds. ABC of wound healing. Oxford: Blackwell Publishing/BMJ Books 200624–27.