Abstract
Objectives
To investigate clinical features and outcomes in patients with acute cholecystitis with gall bladder perforation receiving open cholecystectomy or percutaneous transhepatic gall bladder drainage in the emergency department.
Methods
From 1996 through 2005, 33 patients with non‐traumatic gall bladder perforation, among 585 patients with acute cholecystitis, were enrolled. Patients were divided into two groups: open cholecystectomy in 16 patients and percutaneous transhepatic gall bladder drainage in 17 patients. Medical records, including demographic data, past history of systemic diseases or gallbladder stones, initial clinical presentations, laboratory data, physical status, therapeutic interventions, and outcomes, were analysed.
Results
Mean patient age was 72.6 years (range 54–92 years). 28 patients (84.8%) were male. Median time of symptom onset before emergency department diagnosis was 5 days (range 0.5–30 days). Estimated incidence of gall bladder perforation was 5.6% (33/585). 27 patients (81.8%) had gallstones operatively or in image studies. All patients had either right upper quadrant pain/tenderness or epigastric pain/tenderness. Only 9 (27.3%) patients had positive Murphy's sign. Six patients in the percutaneous transhepatic gall bladder drainage group received further open cholecystectomy. Overall mortality was 24.2% (8/33). The direct cause of death was disease related sepsis in all patients. Patients receiving percutaneous transhepatic gall bladder drainage had a higher survival rate than those receiving open cholecystectomy (100% vs 50%, p<0.001). No differences in complications and length of hospital stay of survivors were observed between groups.
Conclusions
In this study, we delineated clinical features of patients with gall bladder perforation. Better clinical outcome is observed for percutaneous transhepatic gall bladder drainage, and this is suggested as an initial therapeutic choice, especially in high risk patients who are likely to need surgery.
The choice of therapeutic modalities for acute cholecystitis includes both open cholecystectomy and percutaneous transhepatic gallbladder drainage. If left untreated, acute cholecystitis can progress to gall bladder perforation. During the past decades, open cholecystectomy has been used to treat acute cholecystitis with gallbladder perforation contributing to the mortality rate ranging from 8.6% to 23% in respective studies.1,2 Risk factors, including older age, increased disease severity, and comorbidities with multiple systemic diseases, were considered to account for the high mortality rate.3,4 In recent years, percutaneous transhepatic gallbladder drainage has been successfully adopted as an alternative or a bridge before elective cholecystectomy for acute cholecystitis,5 and even used in high risk patients for a greatly improved outcome.5,6,7 A favourable outcome was also demonstrated in patients with a localised gall bladder perforation under percutaneous transhepatic gallbladder drainage treatment.8 To the best of our knowledge, there is no report in the literature that compares the outcomes of patients with gall bladder perforation after either open cholecystectomy or percutaneous transhepatic gallbladder drainage at the time of diagnosis in the emergency department. The purpose of this study was to compare the clinical characteristics and outcomes of open cholecystectomy or percutaneous transhepatic gallbladder drainage in patients with gall bladder perforation who were diagnosed in the emergency department. The results of this study will provide a therapeutic reference for both emergency physicians and consultant surgeons managing patients with acute cholecystitis.
Methods
Study design
We conducted this retrospective study in the emergency department of a tertiary referral medical centre, where a mean (SD) of 73 064 (5123) patients were treated each year in past decade. The study was declared exempt from informed consent by the local institutional review board.
Study setting and population
From 1996 through 2005, patient cases were retrospectively identified via a hospital computer database using a hospital discharge diagnosis with International Classification of Diseases code 9: 574–575. We double checked our subject group by comparing this list with the available hospital registration for cholecystitis from the department of general surgery and division of gastroenterology. Patients younger than 14 years old, and patients with traumatic or iatrogenic gall bladder perforation, were excluded from the study. Five hundred and eighty‐five patients met the diagnosis of acute cholecystitis.
Study protocol
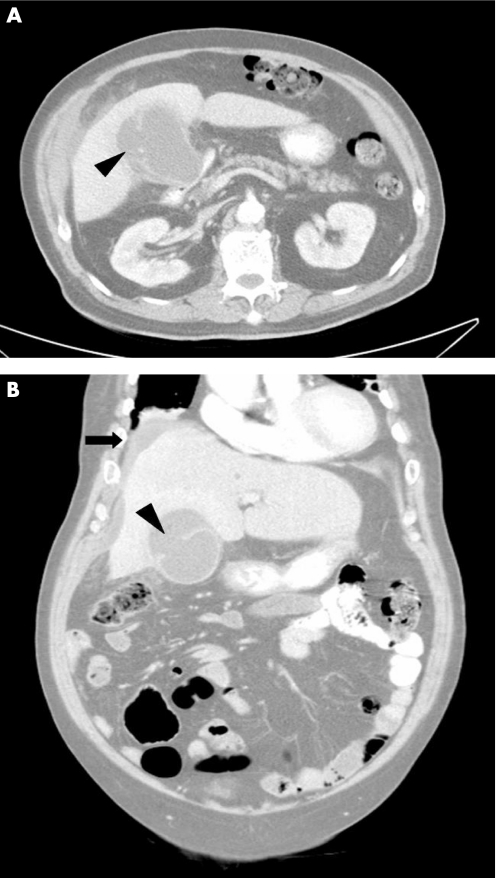
The diagnosis of gall bladder perforation was based on both clinical presentation and either surgical findings with proven pathology or imaging study by the radiologist. The clinical presentations were signs and symptoms similar to acute cholecystitis accompanied by peritoneal signs, with tenderness, rebounding, or muscle guarding over the right upper quadrant or whole abdomen. The imaging study demonstrated a defect of the gallbladder wall or fluid accumulation around a distended gall bladder found on ultrasound9,10 and/or computed tomography (CT) scan.11,12 Figure 1 shows the typical findings on contrast enhanced CT in a patient with gall bladder perforation. A total of 33 adult patients met the inclusion criteria of acute cholecystitis with gall bladder perforation in the emergency department. The medical records of all 33 patients, including demographic data, past history of systemic diseases or gallbladder stone, initial clinical presentations, laboratory data, APACHE II score (Acute Physiology and Chronic Health Evaluation), physical status classified by American Society of Anesthesiologist (ASA),13 therapeutic interventions, complications during hospitalisation and outcomes, were reviewed and analysed. Two therapeutic interventions, open cholecystectomy or percutaneous transhepatic gallbladder drainage, were used to treat patients. Patients received either open cholecystectomy or percutaneous transhepatic gallbladder drainage, as agreed by the patient or family. All procedures were fully explained. The patients understood the benefits and risks of both interventions provided by the medical team, which comprised an emergency physician, a surgeon and a gastroenterologist. In addition to open cholecystectomy or percutaneous transhepatic gallbladder drainage intervention, empiric antibiotics and other supportive treatments were given to all patients. In patients who had surgical pathology, we use the Niemeier classification and divided the gall bladder perforations into three categories14: type I included patients with free perforation of gall bladder and generalised peritonitis; type II included those patients with a localised perforation; and type III included patients with a cholecystoenteric fistula with or without gallstone ileus.
Figure 1 Axial (A) and coronal (B) plane of contrast enhanced CT scan of an 80‐year‐old man with right upper quadrant pain, showing a hypodense fluid collection in communication with the distended gall bladder by a defect on its lateral wall (arrow head) and fluid accumulations over perihepatic and subhepatic area (arrow).
Data collection and analysis
Based on the different therapeutic interventions—open cholecystectomy or percutaneous transhepatic gallbladder drainage—we divided the 33 patients into two groups to analyse the demographic data, clinical features, laboratory data, APACHE II score, ASA classification, complications during hospitalisation, and outcomes. All of the clinical features were compared by non‐parametric (Mann‐Whitney) test for continuous variables or χ2 and Fisher exact test for categorical variables when appropriate. Continuous data are presented as mean (SD). Dichotomous values were given as frequencies and percentages. A value of p<0.05 was considered significant.
Results
Of 33 patients with acute cholecystitis with gall bladder perforation, 16 patients received open cholecystecomy and 17 patients received percutaneous transhepatic gallbladder drainage. The incidence of gall bladder perforation was 5.6% (33/585) in patients with acute cholecystitis. The mean age of all 33 patients was 72.6 (9.2) years, and only four patients were younger than 65 years. Twenty‐eight patients (84.8%) were male. The mean duration of symptoms and signs that occurred before emergency department diagnosis was 6.3 (7.0) days (median 5.0). Twenty‐six patients (78.8%) had at least one of the systemic or cardiopulmonary diseases, including hypertension, diabetes mellitus, cancer, chronic obstructive pulmonary disease, or coronary artery disease. Only eight patients (24.2%) had a history of gallstones. However, in operative findings and imaging studies, either gall bladder or biliary stones were detected in 27 patients (81.8%) with 13 in open cholecystectomy and 14 in percutaneous transhepatic gallbladder drainage, respectively. All patients had either right upper quadrant pain/tenderness or epigastric pain/tenderness. Only nine (27.3%) patients had positive Murphy's sign. With respect to individual laboratory data, serum liver parameters were elevated, including alanine aminotransferase in 12 patients (36.4%), aspartate aminotransferase in 15 (45.5%), γ‐glutamyl‐transferase in 14 (45.2%), alkaline phosphatase in 24 (72.7%), and total bilirubin in 14 (42.4%) of 33 patients. Additionally, elevated C reactive protein was found in 23 of 24 patients (95.8%, mean (SD) 18.3 (8.2) mg/dl). Mildly elevated mean white blood cell count was found. No statistical significance was found in the demographic data, past history, clinical signs and symptoms, laboratory data, and physical status between both patient groups (table 1). According to the ASA classification,13 two patients were classified as V (moribund), and 29 patients were classified as IV (severe systemic disease). Two patients were classified as III (moderate systemic disease).
Table 1 Comparison of demographic, clinical characteristics, and laboratory data in 33 patients with gall bladder perforation undergoing open cholecystectomy or percutaneous transhepatic gallbladder drainage.
| OC (n = 16) | PTGBD (n = 17) | p Value | |
|---|---|---|---|
| Age (years)* | 73.9 (9.4) | 71.4 (9.2) | NS |
| Duration of symptoms and signs before diagnosis (day)* | 5.3 (4.2) | 7.4 (8.9) | NS |
| Past history† | |||
| Gallbladder stone | 3 (18.8) | 5 (31.3) | NS |
| Hypertension | 9 (56.3) | 9 (52.9) | NS |
| Diabetes mellitus | 5 (31.3) | 6 (35.3) | NS |
| CAD | 2 (12.5) | 4 (25.0) | NS |
| Cancer | 2 (12.5) | 2 (12.5) | NS |
| COPD | 0 | 4 (25.0) | NS |
| Clinical symptoms/signs† | |||
| RUQ pain/tenderness | 15 (93.8) | 16 (94.1) | NS |
| Murphy's sign | 5 (31.3) | 4 (23.5) | NS |
| Epigastric pain/tenderness | 12 (75.0) | 11 (64.7) | NS |
| Diffuse pain/tenderness | 8 (50.0) | 4 (23.5) | NS |
| Fever/chills | 12 (75.0) | 14 (87.5) | NS |
| Nausea/vomiting | 10 (62.5) | 8 (47.1) | NS |
| WBC (4500–11000/mm3)* | 13648.1 (5653.5) | 15505.9 (8679.6) | NS |
| Band (%) | 3.8 (4.9) | 1.7 (3.3) | |
| Segment (45–75%) | 83.5 (7.6) | 85.1 (4.7) | |
| AST (0–40 U/l)* | 70.1 (75.6) | 58.8 (63.3) | NS |
| ALT (0–40 U/l)* | 37.1 (39.9) | 64.6 (92.8) | NS |
| ALP (10–100 U/l)* | 129.7 (45.7) | 155.9 (95.3) | NS |
| Total bilirubin (0.2–1.6 mg/dl)* | 3.5 (4.5) | 3.6 (4.5) | NS |
| BUN (0–20 mg/dl)* | 33.4 (24.2) | 28.3 (16.5) | NS |
| Creatinine (0–1.5 mg/dl)* | 2.4 (2.3) | 1.5 (0.7) | NS |
| APACHE II score* | 21.3 (2.2) | 21.5 (3.5) | NS |
| ASA classification†‡ | |||
| III | 1 (6.3) | 1 (5.9) | |
| IV | 15 (93.7) | 14 (82.4) | |
| V | 0 | 2 (11.8) |
ALT, alanine aminotransferase; ALP, alkaline phosphatase; APACHE, Acute Physiology and Chronic Health Evaluation; AST, aspartate aminotransferase; BUN, blood urea nitrogen; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; NS, not significant; OC, open cholecystectomy; PTGBD, percutaneous transhepatic gallbladder drainage; RUQ, right upper quadrant; WBC, white blood cell count.
*Mean (SD)
†Number (%)
‡American Society of Anesthesiologists physical status classification.
Comparison of complications and outcomes in both patient groups during hospitalisation is shown in table 2. The most common complication during hospitalisation was stress ulcer or upper gastrointestinal bleeding in 15 patients (45.5%), followed by acute renal failure in 5 (15.2%), pneumonia in 5 (15.2%), and urinary tract infection in 4 (12.1%). Patients who received percutaneous transhepatic gallbladder drainage had a significantly higher survival rate than those who received open cholecystectomy (100% vs 50%, p<0.001) (table 2). Overall, the mortality rate was 24.2%. The direct cause of death was disease related sepsis in all patients. There was no between group differences with respect to the total complications and length of hospital stay among survivals.
Table 2 Comparison of complications and outcomes in 33 patients with gall bladder perforation receiving open cholecystectomy or percutaneous transhepatic gallbladder drainage.
| OC (n = 16) | PTGBD (n = 17) | p Value | |
|---|---|---|---|
| Complications during hospitalisation* | 8 (50.0) | 11 (64.7) | NS |
| Stress ulcer or UGI bleeding* | 7 (43.8) | 8 (47.1) | NS |
| Acute renal failure* | 5 (31.3) | 0 | 0.018 |
| Pneumonia* | 5 (31.3) | 0 | 0.018 |
| Urinary tract infection* | 1 (6.3) | 3 (17.6) | NS |
| Survival to discharge* | 8 (50.0) | 17 (100) | 0.001 |
| Hospital stay of survivors (days)† | 21.3 (18.9) | 29.1 (21.2) | NS |
NS, not significant; OC, open cholecystecomy; PTGBD, percutaneous transhepatic gallbladder drainage; UGI, upper gastrointestinal.
*Number (%).
†Mean (SD).
Among the 17 patients with percutaneous transhepatic gallbladder drainage, two patients received endoscopic extraction with papillotomy to remove common bile duct stone, and six patients received elective open cholecystectomy during hospitalisation. No fatal complication developed after these procedures. Eleven patients did not receive subsequent open cholecystectomy during hospitalisation because of older age, with severe comorbid diseases in eight patients and no biliary stone in three patients. Three of these 11 patients without elective open cholecystectomy developed recurrent cholecystitis during the follow up period that ranged from 7–32 months. All three patients had a good recovery after percutaneous transhepatic gallbladder drainage treatment. Table 3 shows the results of Niemeier's classification of the 22 patients who had surgical pathology. It demonstrated that either type I or II patients receiving percutaneous transhepatic gallbladder drainage had a better outcome than those receiving open cholecystectomy, but the difference was not statistically significant.
Table 3 Therapeutic strategies and outcomes according to Niemeier's classification in 22 patients with surgical pathology.
| OC (n = 16) | PTGBD with elective OC (n = 6) | Total patients (n = 22) | |
|---|---|---|---|
| Type I | 3/8 (37.5)* | 2/2 (100)* | 5/10 (50.0)* |
| Type II | 5/8 (62.5)* | 4/4 (100)* | 9/12 (75.0)* |
| Type III | 0 | 0 | NA |
NA, not accessible; OC, open cholecystecomy; PTGBD, percutaneous transhepatic gallbladder drainage.
*Survived patients/all patients (survival percentage).
Discussion
Gall bladder perforation is a complication experienced by 2–11% of patients with acute cholecystitis.8,15 In the current study, the incidence of gall bladder perforation was 5.6% (33/585) among patients diagnosed with acute cholecystitis in the emergency department. The characteristics of our patients were older age with longer duration of signs and symptoms, high percentage of systemic diseases, right quadrant pain or tenderness, mild leucocytosis, and poor physical status. These clinical presentations were similar to those patients with acute cholecystitis without perforation. This condition may present a great challenge to emergency physicians due to possible delay in patient presentation to the emergency department, difficulty in recognition and diagnosis,16 and association with high morbidity and mortality.8,15,17 Emergency physicians should perform prompt imaging studies, including ultrasound or CT scan, upon suspicion of this uncommon disease.
With regard to the therapeutic intervention for gall bladder perforation, open cholecystectomy should be performed as quickly as possible if gallbladder perforation has developed.1,15 However, the operative mortality rate associated with this surgery is in the range of 8.6–23% according to the literature,1,2 and even up to 90% in some patients with delayed diagnosis or treatment.18 The application of ultrasound guided percutaneous transhepatic gallbladder drainage to treat acute cholecystitis with empyema was proposed by Radder in 1980.19 It is a simple, local, and less invasive procedure, which is mainly indicated in high risk patients with moribund condition, old age, or severe systemic disease unsuitable for open or laparoscopy cholecystectomy.19,20 By using percutaneous transhepatic gallbladder drainage, gallbladder decompression as well as improvement of local circulation and infection can be achieved.21 Currently, it is considered as a bridge before elective open cholecystectomy or an interval laparoscopic cholecystectomy for acute cholecystitis.5,6,22 In addition, percutaneous transhepatic gallbladder drainage can be used for cholangiography, which is very important for revealing the anatomy of biliary tract and further therapeutic suggestions.5,6 In recent years, based on the maturity of this technique, many studies indicate that percutaneous transhepatic gallbladder drainage can greatly reduce both the mortality and morbidity rate in high risk patients with acute cholecystitis.6,7,23 Felice et al reported that 35 patients with gall bladder perforation, receiving either open cholecystectomy or percutaneous transhepatic gallbladder drainage, had a mortality rate of 8.6% and 22%, respectively.1 In other words, patients receiving percutaneous transhepatic gallbladder drainage seemed have poorer outcome than patients receiving open cholecystectomy. However, percutaneous transhepatic gallbladder drainage was used as a rescue treatment for the moribund patients who were unsuitable for open cholecystectomy in their study. In this study, overall mortality rate was high (24.2%), and no mortality was noted in the percutaneous transhepatic gallbladder drainage group. Our high mortality rate may be attributed to many factors, including the older age of the patients (mean age of 72.6 years), multiple comorbid systemic diseases, delayed emergency department visits and diagnosis, and poor physical status classification.
To the best of our knowledge, the current therapeutic interventions for gall bladder perforation are open cholecystectomy and percutaneous transhepatic gallbladder drainage with subsequent cholecystectomy. Other supportive care, including antibiotics and fluid supplementation for sepsis caused by biliary peritonitis, are mandatory. It remains a great challenge to determine the best choice among these procedures for improving survival and reducing hospital complications during the short stay in the emergency department. The clinical characteristics of our 33 study patients, including age, past systemic diseases, clinical symptoms and signs, and risk factors, were comparable with previous case series studies.3,4,24 No statistical significant difference in clinical characteristics was found between both groups, even when utilising the APACHE II score and the ASA classifications for preoperative risk assessment (table 1). We suggest percutaneous transhepatic gallbladder drainage is more beneficial in the initial treatment of gall bladder perforation, due to the higher survival rate. Additionally, fewer complications associated with acute renal failure and pneumonia during hospitalisation were found in patients who received percutaneous transhepatic gallbladder drainage (p<0.05, Fisher exact test). However, some disadvantages were noted, including a longer hospital stay in survival patients, subsequent elective open cholecystectomy, or endoscopic extraction with papillotomy for the removal of biliary stones in the percutaneous transhepatic gallbladder drainage group. The major complications of percutaneous transhepatic gallbladder drainage that occurred frequently included haemorrhage, hypotension due to sepsis or vasovagal reaction, pneumothorax, bile leakage, and puncture of intra‐abdominal organs.25 However, these can be avoided by a well experienced invasive radiologist, who can successfully achieve a 100% safety record.5 Minor complications included incorrect catheter positioning, catheter dislodgment, and colonisation of the gallbladder with new bacteria.25 Major complication rates were reported to range from 3–8%, with the incidence of minor complications ranging from 4–13%.26,27 In 17 patients receiving percutaneous transhepatic gallbladder drainage in this study, three patients suffered from catheter dislodgment with successful replacement later. Two patients had minor local bleeding with spontaneous resolution after conservative treatment. Overall, no major complication was detected, but minor complications occurred in five patients (29.4%).
Limitations
This investigation has several limitations. First, data were collected from a retrospective chart review. Some clinical presentations or records may not have been documented completely. Second, due to retrospective analysis, both the diagnostic modalities and treatments of the gall bladder perforation cases could not be standardised. We could not strongly advocate that percutaneous transhepatic gallbladder drainage was absolutely superior to open cholecystectomy in treating gall bladder perforation. A randomised prospective trial would serve to prove which method is better. Third, in patient selection, patients whose gall bladder perforation developed during hospitalisation, but not in the emergency department, and patients with traumatic cause were excluded from our study. Further investigation is needed to delineate therapeutic strategies for these patients. Fourth, the emergency department diagnosis of gall bladder perforation may be false positive or false negative in some patients without surgical validation. This is an insuperable limitation of this study; however, we have made every effort to provide the correct diagnosis by clinical and image correlation.
Conclusions
We delineated the clinical characteristics of 33 patients with gall bladder perforation who presented to a single emergency department setting and received either percutaneous transhepatic gallbladder drainage or open cholecystectomy at a medical centre over the past 10 years. Based on outcomes assessment, percutaneous transhepatic gallbladder drainage was shown to have a better survival rate and fewer complications. However, a longer duration of hospital stay was noted. We suggest that percutaneous transhepatic gallbladder drainage can be considered as an initial therapeutic choice in patients with gall bladder perforation.
Footnotes
Competing interests: None declared.
References
- 1.Felice P R, Trowbridge P E, Ferrara J J. Evolving changes in the pathogenesis and treatment of the perforated gallbladder. A combined hospital study. Am J Surg 1985149466–473. [DOI] [PubMed] [Google Scholar]
- 2.Isch J H, Finneran J C, Nahrwold D L. Perforation of the gallbladder. Am J Gastroenterol 197155451–458. [PubMed] [Google Scholar]
- 3.Tsai C J, Wu C S. Risk factors for perforation of gallbladder. A combined hospital study in a Chinese population. Scand J Gastroenterol 1991261027–1034. [DOI] [PubMed] [Google Scholar]
- 4.Roslyn J J, Thompson J E, Jr, Darvin H.et al Risk factors for gallbladder perforation. Am J Gastroenterol 198782636–640. [PubMed] [Google Scholar]
- 5.Sugiyama M, Tokuhara M, Atomi Y. Is percutaneous cholecystostomy the optimal treatment for acute cholecystitis in the very elderly? World J Surg 199822459–463. [DOI] [PubMed] [Google Scholar]
- 6.Berman M, Nudelman I L, Fuko Z.et al Percutaneous transhepatic cholecystostomy: effective treatment of acute cholecystitis in high risk patients. Isr Med Assoc J 20024331–333. [PubMed] [Google Scholar]
- 7.Patel M, Miedema B W, James M A.et al Percutaneous cholecystostomy is an effective treatment for high‐risk patients with acute cholecystitis. Am Surg 20006633–37. [PubMed] [Google Scholar]
- 8.Menakuru S R, Kaman L, Behera A.et al Current management of gall bladder perforations. ANZ J Surg 200474843–846. [DOI] [PubMed] [Google Scholar]
- 9.Madrazo B L, Francis I, Hricak H.et al Sonographic findings in perforation of the gallbladder. Am J Roentgenol 1982139491–496. [DOI] [PubMed] [Google Scholar]
- 10.Sood B P, Kalra N, Gupta S.et al Role of sonography in the diagnosis of gallbladder perforation. J Clin Ultrasound 200230270–274. [DOI] [PubMed] [Google Scholar]
- 11.Mihas A A, Lewis G, Athar M.et al Gallbladder perforation: preoperative diagnosis by combined imaging techniques. Gastrointest Radiol 19921724–26. [DOI] [PubMed] [Google Scholar]
- 12.Kim P N, Lee K S, Kim I Y.et al Gallbladder perforation: comparison of US findings with CT. Abdom Imaging 199419239–242. [DOI] [PubMed] [Google Scholar]
- 13.Keats A S. The ASA classification of physical status–a recapitulation. Anesthesiology 197849233–236. [DOI] [PubMed] [Google Scholar]
- 14.Niemeier O W. Acute free perforation of the gallbladder. Ann Surg 193499922–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abu‐Dalu J, Urca I. Acute cholecystitis with perforation into the peritoneal cavity. Arch Surg 1971102108–110. [DOI] [PubMed] [Google Scholar]
- 16.Ong C L, Wong T H, Rauff A. Acute gall bladder perforation – a dilemma in early diagnosis. Gut 199132956–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lennon F, Green W E. Perforation of the gallbladder. A review of 32 cases. J R Coll Surg Edinb 198328169–173. [PubMed] [Google Scholar]
- 18.MacDonald J A. Perforation of the gallbladder associated with cholecystitis: eight year review of 20 cases. Ann Surg 1966164849–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radder R W. Ultrasonically guided percutaneous catheter drainage for gallbladder empyema. Diagn Imaging 198049330–333. [PubMed] [Google Scholar]
- 20.Akhan O, Akinci D, Ozmen M N. Percutaneous cholecystostomy. Eur J Radiol 200143229–236. [DOI] [PubMed] [Google Scholar]
- 21.Wong S R, Lee K T, Kuo K K.et al Ultrasound‐guided percutaneous transhepatic drainage of gallbladder followed by cholecystectomy for acute cholecystitis–10 years' experience. Kaohsiung J Med Sci 19981419–24. [PubMed] [Google Scholar]
- 22.Macri A, Scuderi G, Saladino E.et al Acute gallstone cholecystitis in the elderly: treatment with emergency ultrasonographic percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Surg Endosc 20062088–91. [DOI] [PubMed] [Google Scholar]
- 23.Li J C, Lee D W, Lai C W.et al Percutaneous cholecystostomy for the treatment of acute cholecystitis in the critically ill and elderly. Hong Kong Med J 200410389–393. [PubMed] [Google Scholar]
- 24.Stefanidis D, Sirinek K R, Bingener J. Gallbladder perforation: risk factors and outcome. J Surg Res 2006131204–208. [DOI] [PubMed] [Google Scholar]
- 25.Gordon B, Werbel Nahrwold D L, Joehl R J.et al Percutaneous cholecystostomy in the diagnosis and treatment of acute cholecystitis in the high‐risk patient. Arch Surg 1989124782–785. [DOI] [PubMed] [Google Scholar]
- 26.VanSonnenberg E, D'Agostino H B, Goodacre B W.et al Percutaneous gallbladder puncture and cholecystostomy: results, complications and caveats for safety. Radiology 1992183163–170. [DOI] [PubMed] [Google Scholar]
- 27.Van Overhagen H, Meyers H, Tilanus H W.et al Percutaneous cholecystostomy for patients with acute cholecystitis and an increased surgical risk. Cardiovasc Intervent Radiol 19961972–76. [DOI] [PubMed] [Google Scholar]