Abstract
Prehospital cervical spine (c‐spine) immobilisation is common, despite c‐spine injury being relatively rare. Unnecessary immobilisation results in a significant burden on limited prehospital and emergency department (ED) resources. This study aimed to determine whether the incidence of unnecessary c‐spine immobilisation by ambulance personnel could be safely reduced through the implementation of an evidence‐based algorithm. Following a training programme, complete forms on 103 patients were identified during the audit period, of which 69 (67%) patients had their c‐spines cleared at scene. Of these, 60 (87%) were discharged at scene, with no clinical adverse events reported, and 9 (13%) were taken to the local ED with non‐distracting minor injuries, all being discharged home the same day. 34 (33%) patients could not have their c‐spines safely cleared at scene according to the algorithm. Of these, 4 (12%) patients self‐discharged at scene and 30 (88%) were conveyed to an ED as per the normal procedure. C‐spine clearance at scene by ambulance personnel may have positive impacts on patient care, efficient use of resources and cost to healthcare organisations.
Blunt trauma can lead to cervical spine injury (CSI) in 2–4% of cases.1 Although the incidence of actual spinal cord injury is low (0.7%) and the reported rate of missed CSI is very low (0.01%), the consequences of an inappropriately managed CSI are significant.2 Following implementation of the Advanced Trauma Life Support course3 in the UK, and publication of guidelines by the Faculty of Prehospital Care, Royal College of Surgeons, Edinburgh, UK, on spinal immobilisation and extrication,4 the practice is now to assume the presence of CSI in any patient with a potential mechanism for CSI or relevant clinical findings, and proceed to triple immobilisation of the cervical spine (c‐spine). In the UK, this means a cervical collar, head restraints and either a long spinal board or orthopaedic scoop stretcher. “Full immobilisation” with no actual underlying injury may be associated with unnecessary patient morbidity in addition to inefficient use of resources by the ambulance service and emergency departments (EDs). Several studies5,6,7 have now shown that ED nurses can safely remove c‐spine protection from low‐risk patients without medical involvement.
Our objective was to introduce a clinical decision algorithm to allow qualified ambulance personnel to discriminate safely between patients who do, or do not, require cervical immobilisation. In addition, we anticipated that in patients with no other injuries who would otherwise have been conveyed to the ED, a change in practice would result, enabling ambulance personnel to treat and discharge patients at scene.
Methods
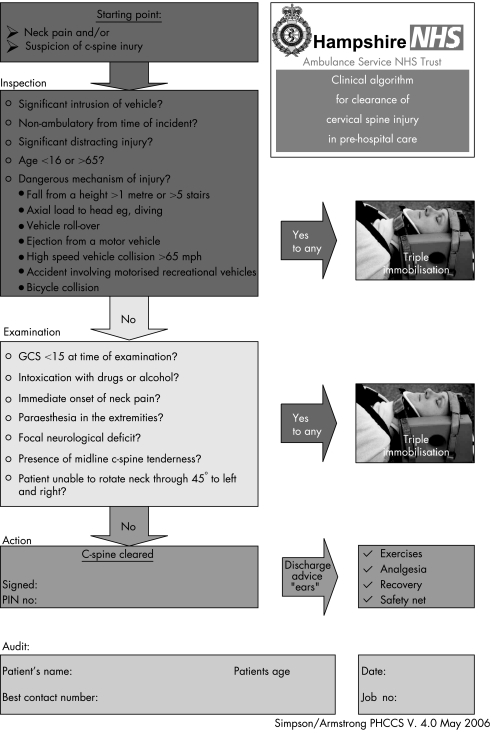
Using the National Emergency X‐Radiography Utilization Study criteria8 and National Institute for Health and Clinical Excellence9 guidelines, a clinical decision algorithm was constructed, which indicated the need for conventional triple immobilisation of the patient's c‐spine if any one of a sequence of criteria were positive (fig 1).10
Figure 1 Clinical decision algorithm. c‐spine, cervical spine; GSC, Glasgow Coma Scale.
To evaluate the training, a pilot study was performed within a limited study area—a district general hospital ED and an ambulance station with the same catchment areas. Prior approval was granted by both the Hampshire Ambulance Service Clinical Advisory Group and the clinical audit department at North Hampshire Hospital, Basingstoke, UK. As the guideline was introduced to improve patient safety and formalise an existing practice, gaining consent from the patient was not considered necessary.
Seventeen trained ambulance personnel (paramedics and technicians) were given 3 h of education and training (lecture, skills stations and formative testing) in prehospital c‐spine clearance and patient information9 after head injury using the algorithm, by a faculty of five consultant emergency care practitioners. After training, they were allowed to use the algorithm, with an appropriate patient and return an audit form. Completed forms were returned to the ED for analysis. A database was constructed using Microsoft ACCESS 2000 to collate and report the results. Copies of the algorithm were supplied to the trained ambulance personnel, which served as a reference, a clinical document and the audit tool.
Results
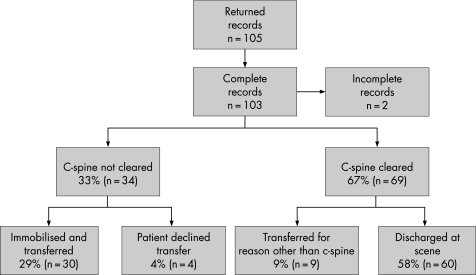
A total of 105 audit forms were returned during the audit period, which extended over 26 months (fig 2). Two cases were excluded with incomplete data. Of the 103 patients, 69 (67%) had no significant CSI identifiable at scene, of which 9 (9%) were taken to the local ED with other injuries, but all were discharged home the same day. In all, 60 (58%) were discharged at scene, with no clinical adverse events reported; 34 (33%) did not have their c‐spines cleared at scene. Of these, 4 (4%) self‐discharged at scene, all of whom would have required immobilisation; in all 4 cases, the criterion for immobilisation was vehicle rollover. A total of 30 (29%) patients were conveyed to an ED.
Figure 2 Flow chart of returned audit forms. c‐spine, cervical spine.
During and in the 6 months following the study period, no reports of missed CSI were reported to the ED or ambulance service by patients, other EDs, general practitioners, regional neurological centres or coroners' offices. In addition, no attendances were identified on the ED attendance database for those patients who self‐discharged at scene during the audit period.
Discussion
No decision‐making tool has yet been validated for the clearance of c‐spine after injury in prehospital care. Such tools have, however, been validated in the hospital environment with some evidence to support clearance of c‐spine by nurses in the ED.5,6,7 Studies of prehospital clearance are limited, with one study recommending that with effective training, audit and quality management, the decision should rest with individual emergency medical services.11
Before the initiation of this work, it was custom and practice for some crews to “clear” c‐spines at the scene. This practice had evolved over time, was idiosyncratic to practitioners, and sometimes resulted in patients being immobilised by hospital staff on arrival at the hospital, when specific criteria such as distracting injury were identified, demonstrating that apparent clinical risk existed in the safe transfer of patients. Given that this was already custom and practice, this work was considered as an improvement in care by formalising this process. Providing clinical guidance on safe clearance of c‐spines was therefore not considered to be research—a view that was upheld by the Hampshire Ambulance Trust Clinical Advisory Group, which supported a pragmatic decision to extrapolate and apply existing evidence to train ambulance personnel within a defined locality and evaluate its impact.
Although the Canadian C‐Spine rules12 have greater sensitivity and specificity in clinical practice, the algorithm used for the study combined the National Emergency X‐Radiography Utilization Study criteria8 and National Institute for Health and Clinical Excellence9 guidelines, both of which are evidence based, into a graphic format. This led the ambulance personnel through a sequence of criteria—any positive identification mandated the application of currently taught practice, that of triple immobilisation of the c‐spine and transfer to the nearest ED for further assessment. Only if all the criteria were negative could the patient be managed without spinal immobilisation.
To reinforce the sequence of criteria, the algorithm incorporated a traffic light system. The criteria were grouped into “inspection” (red) and “examination” (amber). This prioritised the immediately apparent factors, such as a patient who is trapped or not fully conscious, over the clinical examination. In particular, the final criterion was assessment of the range of movement of the neck. Only after exclusion of all relevant factors could the c‐spine be cleared (green).
The findings of this audit indicate that after appropriate training, ambulance personnel were able to apply safely a clinical decision algorithm for prehospital c‐spine clearance. A number of potential benefits may be realised by prehospital c‐spine clearance. For the patient, unnecessary c‐spine immobilisation can be avoided. For the ambulance service, there is a potential for safe discharge from the scene, reduction in ambulance transportation and early release of vehicles.
Limitations
The findings from this audit cannot be generalised. The selection of patients depended on the application of the decision algorithm by ambulance crews who were participating in the audit, potentially resulting in selection bias. Formal follow‐up with the patient was not conducted to assess whether they sought alternative healthcare with problems in the neck after prehospital c‐spine clearance.
Conclusion
This audit indicates that trained ambulance personnel can carry out prehospital c‐spine clearance safely and effectively. Further research is required in the form of a multicentre randomised control trial before widespread adoption is recommended.
Acknowledgements
We thank the ambulance staff from Basingstoke Ambulance Station, South Central Ambulance Service (Hampshire Division).
Abbreviations
c‐spine - cervical spine
CSI - cervical spine injury
ED - emergency department
Footnotes
Competing interests: BPA, HKS and CDD are members of the South Central Ambulance Service (Hampshire Division), Clinical Advisory Group.
References
- 1.Davis J W, Phreaner D L, Hoyt D B.et al The aetiology of missed cervical spine injuries. J Trauma 199334342–346. [DOI] [PubMed] [Google Scholar]
- 2.Grossman M D, Reilly P M, Gillett T.et al National survey of the incidence of cervical spine injury and approach to cervical spine clearance in US trauma centres. J Trauma 199947684–690. [DOI] [PubMed] [Google Scholar]
- 3.American College of Surgeons Committee on Trauma. Advanced trauma life support course for physicians. 6th edn. Chicago: American College of Surgeons, 1997
- 4.Faculty of Pre‐Hospital Care of the Royal College of Surgeons of Edinburgh, JRCALC Joint position statement on spinal immobilisation and extrication. J Pre‐hosp Imm Care 19982169–172. [Google Scholar]
- 5.Pitt E, Pedley D K, Nelson A.et al Removal of C‐spine protection by A&E triage nurses: a prospective trial of a clinical decision making instrument. Emerg Med J 200623214–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sexton J. Can nurses remove spinal boards and cervical collars safely? Emerg Nurse 199968–12. [DOI] [PubMed] [Google Scholar]
- 7.Charters A. Can nurses, working in the emergency department, independently clear cervical spines? : a review of the literature, Accid Emerg Nurs 20041219–23. [DOI] [PubMed] [Google Scholar]
- 8.Hoffman J R, Mower W M, Wolfson A B.et al Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med 200034394–99. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Clinical Excellence Head injury: triage, assessment, investigation and early management of head injury in infants, children and adults. Clinical guideline 4, 2003. http://www.nice.org.uk/pdf/cg4niceguideline.pdf (accessed 28 Mar 2007) [PubMed]
- 10.Stiell I G, Wells G A, Vandemheen K L.et al The Canadian C‐spine rule for radiography in alert and stable trauma patients. JAMA 20012861841–1848. [DOI] [PubMed] [Google Scholar]
- 11.Hankins D G, Rivera‐Rivera E J, Ornato J P.et al Spinal immobilisation in the field: clinical clearance criteria and implementation. Prehosp Emerg Care 2001588–93. [DOI] [PubMed] [Google Scholar]
- 12.Stiell I G, Clement C, McKnight R D.et al The Canadian C‐Spine rule versus the NEXUS low risk criteria in patients with trauma. N Engl J Med 20033492510–2518. [DOI] [PubMed] [Google Scholar]