Outcome from major trauma is improved by a multidisciplinary trauma team.1 The Royal College of Surgeons (RCS) has suggested criteria for activation of the trauma team,2 although the evidence to support these is limited, and anecdote suggests that criteria vary among similar hospitals. We undertook a cross‐sectional survey of trauma team activation (TTA) criteria used by the six hospitals within the South West Peninsula designated to receive cases of major trauma.
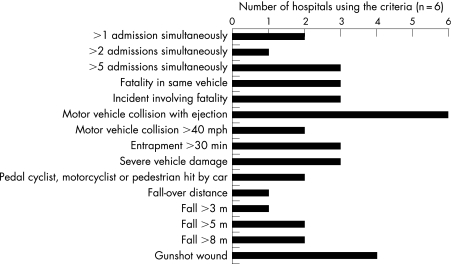
The results highlight a wide variation in the criteria used. One hospital used a two‐tier activation system; the rest had a single set of criteria for TTA. Figure 1 illustrates the variation in mechanistic criteria. Pulse >120/min and oxygen saturations <90% were the most frequently used physiological criteria (67%, n = 4); 67% of hospitals also used systolic hypotension (<90 mm Hg in three hospitals and <100 mm Hg in one hospital). The anatomical criteria again showed disparity, with no criteria being used by more than half of the hospitals. When compared with the RCS recommendations, two hospitals complied and one used RCS criteria along with some locally added elements.
Figure 1 Mechanism of injury criteria.
Criteria would ideally be sensitive and specific in their prediction of serious injury and accurately identify those patients who would benefit most from multidisciplinary care. Regional and national standardisation of TTA criteria would optimise patient care and facilitate healthcare practitioner training while providing a firm basis for research and audit of practice. Now is the opportunity for the College of Emergency Medicine to lead trauma care in the UK by developing such evidence‐based criteria.
We suggest more widespread use of a two‐tier activation system, involving a first tier (a team within the emergency department) activated on the basis of traditional mechanistic criteria, and a second multi‐disciplinary tier activated in the presence of additional physiological abnormality. This has been shown to be safe and cost effective, with no adverse influence on outcome in several centres in the US.3,4,5,6
Footnotes
Competing interests: None.
References
- 1.Petrie D, Lane P, Stewart T C. An evaluation of patient outcomes comparing trauma team activation versus trauma team activation not activated using TRISS analysis. J Trauma 199641870–875. [DOI] [PubMed] [Google Scholar]
- 2.Royal College of Surgeons Better care for the severely injured. London: RCS, 2000
- 3.Ochsner M G, Schmidt J A, Rozycki G S.et al The evaluation of a two‐tier trauma response system at a major trauma center: is it cost effective and safe? J Trauma 199539971–977. [DOI] [PubMed] [Google Scholar]
- 4.Terregino C A, Reid J C, Marburger R K.et al Secondary emergency department triage (supertriage) and trauma team activation: effects on resource utilization and patient care. J Trauma 19974361–64. [DOI] [PubMed] [Google Scholar]
- 5.Plaisier B R, Meldon S W, Super D M.et al Effectiveness of a 2‐specialty, 2‐tiered triage and trauma team activation protocol. Ann Emerg Med 199832436–441. [DOI] [PubMed] [Google Scholar]
- 6.Eastes L S, Norton R, Brand D.et al Outcomes of patients using a tiered trauma response protocol. J Trauma 200150908–913. [DOI] [PubMed] [Google Scholar]