Abstract
Objective
This study evaluated a model of the impact of borderline and antisocial personality disorder indications on HIV symptoms and health-related quality of life (HRQoL) in AIDS-bereaved adults, accounting for grief severity, social support and years since HIV diagnosis.
Design
Structural Equation modeling was used to test the proposed model in a sample of 268 HIV-seropositive adults enrolled in an intervention for coping with AIDS-related bereavement.
Main Outcome Measures
Functional Assessment of HIV Infection, HIV symptoms.
Results
The proposed model demonstrated excellent fit with study data and all hypothesized paths were supported. Personality disorder indication was directly related to HIV symptoms and HRQoL, and indirectly related through both social support and grief severity. Social support was negatively related to HIV symptoms and positively related to HRQoL, while grief severity was positively related to HIV symptoms and negatively related to HRQoL. Finally, HIV symptoms had a direct negative relationship with HRQoL.
Conclusion
Personality disorders have a direct negative effect on HIV symptoms and HRQoL, and indirect effects through grief severity and social support.
Keywords: HIV/AIDS, quality of life, bereavement, personality disorders, social support
Introduction
Personality disorders (PD) and problematic personality traits represent stable maladaptive patterns of thinking, feeling, behaving, and relating, and have been linked to HIV risk behavior, poor quality of life, reduced treatment adherence, poorer or delayed treatment outcomes, and compromised relationships with caregivers (Black et al., 2006; Haller & Miles, 2003; Hutton & Treisman, 2008; Palmer, Salcedo, Miller, Winiarski, & Arno, 2003; Perseius, Andersson, Asberg, & Samuelsson, 2006; Singh & Ochitill, 2006; Treisman & Angelino, 2004). The prevalence of personality disorders among people living with HIV is between 19% and 36% (versus about 10% in the general population), with antisocial PD and borderline PD being the most common (Hutton & Treisman, 2008; Singh & Ochitill, 2006; Treisman & Angelino, 2004). Despite their prevalence, very little research has examined the role of personality disorders or traits in HIV infection, particularly around physical health and functioning. In fact, we are unaware of any research on the impact of personality disorders or traits on the health-related quality of life (HRQoL) of people living with HIV/AIDS.
The current study examined the relationship between personality disorders or traits (PD indication) and HIV symptoms and HRQoL through a secondary data analysis of a sample of bereaved HIV-positive adults who had lost loved ones to AIDS (Sikkema et al., 2006; Sikkema, Hansen, Kochman, Tate, & Difranceisco, 2004). As personality disorders impact one's ability to maintain stable, supportive relationships, including relationships with caregivers and health-protective social networks, social support was hypothesized to mediate the relationship between PD indication and HIV symptoms and HRQoL. Also, as bereavement has been linked to HIV symptom onset (Bower, Kemeny, Taylor, & Fahey, 1998; Reed, Kemeny, Taylor, & Visscher, 1999), grief severity was included in the analysis. Thus, a structural model was tested to examine the direct impact of PD indication on HIV symptoms and HRQoL, as well the indirect impact of PD indication through the potential mediating variables of social support and grief severity.
HIV Infection and Health-Related Quality of Life
With the availability of highly active antiretroviral therapy (HAART), HIV/AIDS has effectively been “transformed from a progressive, fatal illness to a manageable chronic disease” (Mrus et al., 2006, p S39). Given the increases in lifespan, and the potential for serious adverse drug effects, which accompany HAART, HRQoL has emerged as a salient measure of disease impact among persons living with HIV/AIDS (Aranda-Naranjo, 2004; Wu, 2000). HRQoL encompasses multiple domains, including, but not limited to, physical functioning, cognitive functioning, emotional status, and social role performance. HIV specific variables that negatively impact HRQoL include the number, type, and severity of symptoms and the length of time since diagnosis (Bing et al., 2000; Cowdery & Pesa, 2002; Davis, 2004). Psychiatric symptoms (Gore-Felton et al., 2006; Haller & Miles, 2003), grief (Silverman et al., 2000), and poor social support (Burgess et al., 2000) have also been shown to negatively impact HRQoL.
Despite the remarkable advances in treatment, there is no cure for HIV/AIDS, and millions continue to die from the disease. More than half a million people have died from AIDS in the U.S., including between 15,798 and 17,849 annually from 2000 to 2004 (Centers for Disease Control and Prevention, 2006). While HAART prolongs the lives of many people living with HIV/AIDS, about 45% of those in need of HAART in the U.S. do not receive it (Centers for Disease Control and Prevention, 2006). Additionally, reductions in AIDS-related deaths attributed to HAART are being offset by increases in deaths from non-AIDS-defining comorbid conditions among the HIV infected (Lau, Gange, & Moore, 2007). As HIV is typically spread within social and sexual networks, the loss of loved ones to HIV/AIDS is a common experience among the HIV-infected, 80% of whom report a significant loss due to AIDS (Sikkema et al., 2000). Further, bereavement associated with AIDS-related loss has been linked to more rapid symptom onset and increased mortality among the HIV infected (Bower et al., 1998; Reed et al., 1999).
The Relationship of Grief and Social Support to Health-Related Quality of Life
While many people adapt to bereavement over time, for others grieving remains unresolved or complicated (Prigerson & Jacobs, 2001; Zhang, El-Jawahri, & Prigerson, 2006). Factors that increase the risk of complicated grief reactions include: (a) High levels of stress concurrent with the death, (b) lengthy illness leading to the death, and (c) a perceived lack of support from others (Mallinson, 1999; Rando, 1992). People living with HIV infection who are simultaneously coping with AIDS-related loss are particularly vulnerable to complicated grief reactions (Sikkema, Hansen, Meade, Kochman, & Lee, 2005). These individuals must face the death of a loved one to the same disease that is threatening their own life (Sherr, Hedge, Steinhart, Davey, & Petrack, 1992), they are often members of disenfranchised communities, and they have frequently experienced multiple losses with a consequent loss of social support resources. This is particularly relevant for the HIV infected as negative mental and physical health consequences have been associated with bereavement (Silverman et al., 2000; Vanderwerker & Prigerson, 2004) and complicated grief has been found to predict reduced HRQoL of life better than major depressive episodes or posttraumatic stress disorder (Silverman et al., 2000).
In contrast, research on social support consistently shows a positive effect on HRQoL. In fact, among the few conceptual models of HIV-specific HRQoL that have been proposed (e.g., Spirig, Moody, Battegay, & De Geest, 2005; Szaflarski et al., 2006), social support is identified as a key protective element. Social support has been theorized to provide an overall positive effect on well-being and to reduce maladaptive responses to stressful life events (Cohen & Wills, 1985). Indeed, numerous studies have linked social support to HRQoL among HIV-positive adults (Cowdery & Pesa, 2002; Gielen, McDonnell, Wu, O'Campo, & Faden, 2001; Liu et al., 2006; Safren, Radomsky, Otto, & Salomon, 2002; Wu, 2000). In addition to having a direct impact on HRQoL, social support may impact HRQoL indirectly through it's relationship with other associated variables, including problematic personality traits (Burgess et al., 2000), complicated grief (Ott, 2003), and HIV symptoms (Spirig et al., 2005).
The current study evaluated the impact of PD indication on HIV symptoms and HRQoL in a sample of persons with HIV/AIDS who have experienced an AIDS-related loss. Using structural equation modeling (SEM), we examined the direct and indirect relationships of borderline PD and antisocial PD indications, social support, and grief severity on HIV symptoms and HRQoL. Time since HIV diagnosis and number of AIDS-related losses were included in the model as control variables. The overall fit of the hypothesized model to the actual data was tested, as well as specific study hypotheses that: (a) PD indications would have a direct negative effect on HIV symptoms and HRQoL, and indirect effects through social support and grief severity; (b) social support would have a direct positive effect on HIV symptoms and HRQoL, and an indirect effect through grief severity; and (c) grief severity would have a direct negative effect on HIV symptoms and HRQoL.
Methods
Participants and Procedure
Between June 1997 and April 1999, 268 HIV-positive individuals (94 women, 174 men) who had lost a partner/lover, spouse, family member, or close friend to AIDS were recruited to take part in a randomized, controlled trial of a group intervention for coping with AIDS-related bereavement (Hansen et al., in press; Sikkema et al., 2006; Sikkema et al., 2004). Participants were recruited through HIV service organizations and medical and mental health care providers in Milwaukee, WI, and New York, NY according to the following eligibility criteria: (a) health care provider verification of HIV-positive serostatus; (b) experience of an AIDS-related loss not less than one month and not more than two years ago; (c) not currently psychotic, as measured at screening by the Structured Clinical Interview for DSM-IV Screen Patient Questionnaire (SCID Screen PQ; First, Gibbon, Spitzer, & Williams, 1996); and (d) no more than mild cognitive impairment as measured by the Mini Mental Status Exam (MMSE; Folstein, Folstein, & McHugh, 1975).
Information regarding demographics, HIV-infection, AIDS-related loss history, psychiatric history, and mental status (MMSE) was obtained. Two computerized diagnostic screening interviews were administered, the SCID Screen PQ (First et al., 1996) for study eligibility, and the Computer-Assisted SCID-II (CAS-II) program components for antisocial and borderline personality disorders (First, Gibbon, Spitzer, Williams, & Benjamin, 1997). Of the 322 persons screened, 54 did not enter the study (38 dropped out, 15 were ineligible, and 1 died). Those enrolled in the study did not differ from those 54 not enrolled on most demographic characteristics or severity of grief. However, non-participants were more likely than participants to be heterosexual (χ2 = 6.9, p < 0.01) and had fewer sex partners who died of AIDS (t = -2.0, p < 0.05). After screening, eligible participants completed an additional assessment battery, for which they received $40. All affiliated institutional review boards approved the research protocol, and all participants provided written informed consent prior to enrollment.
Measures
Participant Gender
A dichotomous variable indicating participant gender was created. As participants were part of a group intervention study, and groups were conducted separately for heterosexual men, men who have sex with men, and women, three transsexual participants self-selected their gender identification for this study according to their comfort with group composition. Thus, two transsexual participants selected to be grouped with men who have sex with men, and one selected to be grouped with women.
Personality Disorder Indication
A dichotomous variable was created to identify personality disorder indication based on responses to the Computer-Assisted SCID-II (CAS-II) (First et al., 1997). For the current study, only the screening questions for antisocial PD and borderline PD were included. Participants in this study were part of a group intervention RCT, and these disorders may present the most complications for group treatment. While the authors of CAS-II do not recommend using this instrument to establish a diagnosis (First et al., 1997), a number of studies indicate that the CAS-II has utility for this purpose. For example, the CAS-II has been shown to correlate with other measures of personality and symptoms (Piedmont, Sherman, Sherman, & Williams, 2003), have a low false negative rate (Jacobsberg, Perry, & Frances, 1995), have high stability over time (Ouimette & Klein, 1995), and have high sensitivity and utility as an epidemiological tool to estimate rates of personality disorders within a population (Ekselius, Lindstrom, von Knorring, Bodlund, & Kullgren, 1994). No significant differences were found between participants with borderline PD and antisocial PD indications on study variables, and only 16 participants were classified as antisocial, therefore these two variables were combined into a single dichotomous variable indicating the presence or absence of a PD indication. This same procedure has also been used in a study predicting substance use in HIV positive adults (Hansen et al., in press).
Social Support
A latent variable representing the construct of social support was created using the four subscales of the Interpersonal Support Evaluation List (ISEL) (ISEL; Cohen, Mermelstein, Kamarck, & Hoberman, 1985). The ISEL measures perceived social support using four 10-item subscales: (1) Tangible Support, which reflects the availability of material aid; (2) Appraisal Support, which measures the availability of others with whom one can discuss issues of personal importance; (3) Self-Esteem Support, which measures the presence of others who bolsters one's sense of self-worth; and (4) Belonging Support, which reflects the presence of others with whom one can identify and socialize. The ISEL has adequate psychometric properties, including criterion validity, test-retest reliability, and internal consistency (Cohen et al., 1985). For the current sample, internal consistency was good (Tangible Support, α = .84; Appraisal Support, α = .83; Self-Esteem Support, α = .74; Belonging Support, α = .83).
Traumatic Grief Reaction
A latent variable representing traumatic grief was created using the Grief Reaction Index (GRI) (Lennon, Martin, & Dean, 1990) and the two subscales of the Impact of Events Scale (IES) (Horowitz, Wilner, & Alvarez, 1979). The 12-item GRI measures common grief symptoms of numbness, denial, and preoccupation with the deceased (α = .87, current sample). The 15-item IES measures stress associated with traumatic events. It consists of two subscales, including a seven-item Intrusive Subscale reflecting intrusive stress experiences (such as stress-related thoughts, feelings, or bad dreams) and an eight-item Avoidance Subscale reflecting the avoidance of ideas, feelings, and situations associated with a traumatic stressor. Participants completed the IES with the loss of a loved one (or loved ones) to AIDS as the referent traumatic stressor. The IES has been widely used across numerous studies and has well established psychometric properties (Sundin & Horowitz, 2003). Internal consistency was good in the current sample (Intrusion, α = .89; Avoidance, α = .89).
HIV Symptoms
A continuous variable indicating current level of HIV-related symptoms was derived from the sum of participant responses on a 20-item scale (Folkman, Chesney, Collette, Boccellari, & Cooke, 1996). This scale asked participants to rate the severity of 12 physical symptoms associated with HIV infection, including sweating, weight loss, fatigue, shingles, thrush, neuropathy and shortness of breath; as well as 8 more general symptoms, such as headaches, stomach pain, back pain, stiffness, joint or muscle aches or tightness in the chest; over the previous four months using a five-point Likert scale ranging from 0 (not present) to 4 (very severe). Reliability was adequate, with a coefficient alpha of .86 (current sample).
Time since HIV Diagnosis
Participants were asked to indicate the month and year they were diagnosed with HIV infection. A continuous variable was then computed to reflect the number of months between the date of the current assessment and the date of HIV diagnosis.
AIDS-Related Losses
Participants were asked how many people living with HIV they have known who have died from AIDS in the following categories: Friends, lovers/partners, family members, casual sex partners, acquaintances, and others. For the analysis, all categories but the “others” category were summed into a count variable. This resulted in a positively skewed distribution, and a logarithmic transformation was used prior to the SEM analysis.
Health-Related Quality of Life
A continuous variable indicating health-related quality of life was based on the total score of the Functional Assessment of HIV Infection (FAHI; Cella, McCain, Peterman, Mo, & Wolen, 1996). The core of this 55-item self-report measure was based on the Functional Assessment of Cancer Therapy - General (FACT-G) questionnaire, a general health-related quality of life instrument, with an additional subscale specific to HIV infection. The subscales of the FAHI include: Physical Well-being, Social/family Well-being, Emotional Well-being, Relationship with Physician, Functional Well-being, and Additional HIV-specific Concerns. As internal consistency ranged from marginal to good for various subscales, and a measurement model created using SEM indicated poor fit between the FAHI subscales and the study data, individual FAHI subscales were not used in the current analysis. Rather, all items were summed into a total score, with Cronbach's α = .93 in the current sample.
Statistical Analysis
Structural equation modeling (SEM) was used to assess the hypothesized model, including: (a) the overall fit of the model, (b) the amount of variability (R2) of the latent mediating variables and outcome variables accounted for by the predictive variables in the model, and (c) the significance of the direct and indirect structural paths between predictor variables and outcome variables. The goodness of fit χ2, the root mean square error of approximation (RMSEA), the Comparative Fit Index (CFI), and the Tucker-Lewis Index (TLI) were used to evaluate the overall fit of the model. The goodness of fit χ2 assesses the magnitude of discrepancy between the sample and model covariance matrices. A non-significant χ2 value indicates that the hypothesized model does not differ significantly from the actual covariance structure of the data (Hu & Bentler, 1999). The RMSEA assesses absolute fit, taking into account the degrees of freedom in the model. RMSEA values under 0.06 indicate relatively good fit (Hu & Bentler, 1999). The CFI and the TLI assess incremental fit by comparing the absolute fit with an independence model that assumes no relationships among variables. CFI and TLI values equal to or greater than .95 indicate good fit (Hu & Bentler, 1999). The data analysis was conducted using Mplus Version 5.
Results
Demographic and Loss Characteristics
Participants in this study were predominately ethnic minorities (54.1% African-American, 8.6% Hispanic/Latino, 10.1% other) and impoverished, with 90.9% reporting annual incomes under $20,000. Most had completed high school or equivalent (75.7%), with 39.0% reporting some college education. The majority of the men in the sample (78.2%) were men who have sex with men. Participants reported wide variability in disease progression. On average, participants had been living with HIV for seven years (range from two months to 16 years), and, while 35.7% report experiencing no symptoms of HIV, 45.8% report having previously been diagnosed with AIDS. Participants reported tremendous numbers of AIDS-related losses, with many reporting well over 100 deaths. Data was winsorized, with outliers over the 95th percentile (102 AIDS-related deaths) recoded as having experienced 103 AIDS-related deaths, resulting in a sample mean of 16 deaths of loved ones to AIDS (median = 7). One participant in five (19.4%) had lost over 20 loved ones to AIDS. Only 8.6% reported one loss.
Model Predicting Health-Related QOL
Table 1 presents descriptive information for all variables in the structural model compared by gender. The fit of the hypothesized structural model was tested in a three-step process. First, a confirmatory analysis evaluated the measurement model of the two latent constructs (social support and traumatic grief) without any structural paths (Anderson & Gerbing, 1988). Fit statistics of the measurement model were reasonable (χ2 (13) = 28.67, p = .007; CFI = .99; TLI = .98; RMSEA = .07). Second, manifest variables and hypothesized structural paths were added to the model, and this structural model was evaluated. This model failed to achieve fit within the desired parameters (χ2 (42) = 82.98, p < .001; CFI = .97; TLI = .96; RMSEA = .06). Third, an examination of variable correlations (shown in Table 2), modification indices, and loadings within the structural model suggested that the self-esteem subscale of the ISEL was detracting from model fit, and that the model could be improved by removing this variable. Thus, a final model was evaluated with the ISEL self-esteem subscale removed. This model, shown in Figure 1, achieved excellent fit (χ2 (32) = 38.832, p = .189; CFI = .995; TLI = .992; RMSEA = .028, 90% C.I. .000 - .056). Note that all hypothesized paths are shown. The control variables Time Since HIV Diagnosis was hypothesized to be most salient as a predictor of HIV symptoms and HRQoL, and the control variable AIDS-Related Losses was hypothesized to be most salient as a predictor of social support and grief severity. Figure 1 also presents R2 values for each latent variable and outcome variable, indicating the amount of variance accounted for by the structural paths. Table 3 presents all of the coefficients of the direct paths and summed coefficients of indirect paths modeled in Figure 1.
Table 1. Descriptive Data for Independent and Dependent Variables Compared By Gender.
| Men (N = 174) | Women (N = 94) | |||
|---|---|---|---|---|
| Variables | N (%) | N (%) | χ2 | p value |
| Categorical | ||||
| Axis 2 indicated | 7.38 | .025 | ||
| Antisocial Personality Traits | 14 (8.0%) | 2 (2.1%) | ||
| Borderline Personality Traits | 32 (18.4%) | 28 (29.8%) | ||
| Variables | M (s.d.) | M (s.d.) | t | p value |
| Continuous | ||||
| Years since HIV diagnosis | 7.4 (4.1) | 6.1 (3.8) | 2.36 | .019 |
| AIDS-Related Loss | 9.0a | 5.0 a | 3.59 b | .001 |
| HIV Symptoms | 13.11 (10.12) | 15.72 (11.88) | -1.89 | .060 |
| HRQoL (FAHI) | 112.13 (29.77) | 107.47 (32.71) | 1.18 | .239 |
| Social Support | ||||
| ISEL Appraisal subscale | 20.26 (6.33) | 20.01 (5.85) | 0.31 | .754 |
| ISEL Self-Esteem subscale | 18.72 (4.84) | 17.98 (5.08) | 1.18 | .241 |
| ISEL Tangible subscale | 19.81 (6.52) | 18.73 (6.52) | 1.29 | .199 |
| ISEL Belonging subscale | 20.43 (5.78) | 20.31 (6.08) | 0.16 | .875 |
| Grief Severity | ||||
| Grief Reaction Inventory | 18.59 (9.42) | 20.55 (10.85) | 1.53 | .128 |
| IES Intrusion subscale | 14.65 (9.19) | 15.46 (9.93) | 0.67 | .506 |
| IES Avoidance subscale | 14.46 (10.03) | 17.56 (11.90) | 2.25 | .025 |
Median value;
Mann-Whitney U z score.
Table 2. Correlation Matrix of Variables used in the Structural Equation Model.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Axis 2 indicated | -- | |||||||||||
| 2. Years since HIV diagnosis | -.175 | -- | ||||||||||
| 3. AIDS-Related Loss | -.175 | .353 | -- | |||||||||
| 3. HIV Symptoms | .298 | -.004 | -.012 | -- | ||||||||
| 4. HRQoL (FAHI) | -.402 | .127 | .118 | -.645 | -- | |||||||
| 5. ISEL Appraisal Support | -.250 | .072 | .150 | -.313 | .553 | -- | ||||||
| 6. ISEL Self-Esteem Support | -.324 | .162 | .228 | -.311 | .632 | .599 | -- | |||||
| 7. ISEL Tangible Support | -.206 | .056 | .168 | -.319 | .562 | .729 | .602 | -- | ||||
| 8. ISEL Belonging Support | -.233 | .102 | .181 | -.313 | .609 | .807 | .723 | .806 | -- | |||
| 9. GRI | .238 | -.123 | -.021 | .404 | -.466 | -.266 | -.293 | -.295 | -.259 | -- | ||
| 10. IES Intrusion | .223 | -.119 | -.010 | .389 | -.442 | -.215 | -.243 | -.221 | -.206 | .629 | -- | |
| 11. IES Avoidance | .316 | -.109 | -.124 | .341 | -.465 | -.346 | -.369 | -.335 | -.320 | .636 | .725 | -- |
Note: Bold numbers indicate statistical significance (p < .05). FAHI = Functional Assessment of HIV Infection; ISEL = Interpersonal Support Evaluation List; GRI = Grief Reaction Index; IES = Impact of Events Scale.
Figure 1. Structural Equation Model Predicting Health-Related Quality of Life in a Sample of HIV-Positive Adults Who Have Experienced an AIDS-Related Loss.
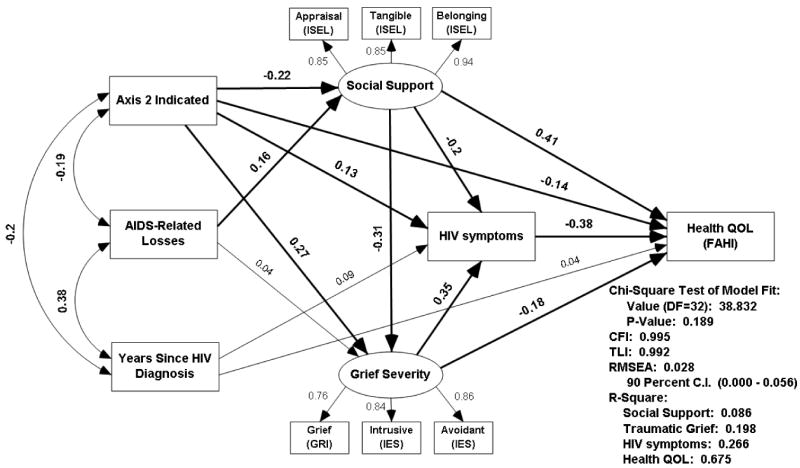
Table 3. Indirect Effects of Predictor Variables on Health-Related Quality of Life.
| Social Support | Grief Severity | HIV Symptoms | HRQoL (FAHI) | ||||
|---|---|---|---|---|---|---|---|
| Direct | Direct | Indirect | Direct | Indirect | Direct | Indirect | |
| Axis II Indicated | -.25*** | .26*** | .07** | .13* | .17*** | -14*** | -.28*** |
| Social Support | -.30*** | -.20** | -.10*** | .41*** | .17*** | ||
| Grief Severity | .35*** | -.18*** | -.13*** | ||||
| HIV Symptoms | -.38*** | ||||||
Value significant, p < .05;
Value significant, p < .01;
Value significant, p < .001.
Two alternative models were tested, though neither provided improvement on the model in Figure 1. A model containing gender and sexual orientation achieved good fit (χ2 (40) = 51.615, p = .103; CFI = .991; TLI = .985; RMSEA = .033, 90% C.I. .000 - .057). Men who have sex with men had experienced more losses, and heterosexual men were less likely to be experiencing HIV symptoms. However, gender and sexual orientation were not associated with any other variables in the model and had no direct or indirect impact on HRQoL. A model with antisocial and borderline PD indications entered independently rather than as a combined variable also achieved good fit (χ2 (36) = 45.328, p = .137; CFI = .993; TLI = .989; RMSEA = .031, 90% C.I. .00 - .056), and the pattern of relationships of antisocial PD and borderline PD were consistent with the model shown in Figure 1, with the exception that the relationship between borderline PD and HIV symptoms only trended toward significance. However, given that there are only 16 participants in the antisocial PD category, the stability of these estimates is questionable.
Discussion
With the widespread availability of HAART, people living with HIV infection in the U.S. are living longer, healthier lives. Consequently, HRQoL is of increasing importance among the HIV infected (Aranda-Naranjo, 2004; Wu, 2000). There is clear evidence that HIV-related symptoms (Bing et al., 2000; Cowdery & Pesa, 2002; Davis, 2004) and complicating comorbid health and psychiatric problems (Gore-Felton et al., 2006; Haller & Miles, 2003; Mrus et al., 2006), impact HRQoL. Previous research using a national probability sample of 2864 HIV positive adults has established that comorbid mood disorders negatively impact HRQoL in HIV positive adults after controlling for HIV symptoms, CD4 count, and stage of disease (Sherbourne et al., 2000). Additionally, complicated grief has been shown to better predict reduced HRQoL than a depressive episode or PTSD (Silverman et al., 2000). The current study extends these findings by demonstrating that an indication of antisocial or borderline personality disorder is a significant predictor of low HRQoL after accounting for social support, grief severity, and HIV symptoms, and directly impacts each of these predictors, resulting in additional indirect effects on HRQoL. There is a dearth of research on the impact of personality disorders on persons living with HIV (Hutton & Treisman, 2008; Singh & Ochitill, 2006), and on HRQoL in general, and to our knowledge this study provides the first empirical evidence linking PD indication with increased HIV symptoms and reduced HRQoL among HIV-seropositive adults.
A total of 28.4% of the study sample had an indication of antisocial or borderline PD. This rate is higher than that found in the general population, but is consistent with documented high rates of personality disorders among HIV-seropositive adults (Hutton & Treisman, 2008; Treisman & Angelino, 2004). Contrary to our expectations, AIDS-Related Losses were positively related to social support, but not to grief severity. It is possible that increased numbers of losses due to AIDS serves to consolidate one's support network. However, our main study hypotheses were supported. The model tested in this study indicated that in bereaved HIV-positive adults, (a) PD indications were related to increased HIV symptoms and decreased HRQoL above and beyond the influences of social support and grief severity, and related to HIV-symptoms and decreased HRQoL indirectly through decreased social support and increased grief severity. Additionally, (b) social support was directly related to decreased HIV symptoms and increased HRQoL, and indirectly related to HIV-symptoms and HRQoL through decreased grief severity. Finally, (c) grief severity was directly related to increased HIV symptoms and decreased HRQoL. The multiple significant paths through which antisocial and borderline PD indication were linked to increased HIV symptoms and reduced HRQoL in this model indicate that personality disorders are an important diagnostic category to consider in research and intervention efforts for improving HRQoL among HIV-seropositive adults.
The results of this study should be interpreted within the context of the study limitations. While the CAS-II, which was used to assess antisocial and borderline PD indications in this study, has been found to reliably identify personality disorders (Ekselius et al., 1994), it does not represent a formal personality disorder diagnosis as defined by the Diagnostic and Statistical Manual of Mental Disorders- IV (American Psychiatric Association, 1994). Also, study data are cross-sectional observations, thus compromising the ability to draw firm conclusions regarding temporal or casual relationships between variables in the model. For example, the path between social support and grief can be reversed without negatively impacting model fit. We prefer the model as presented, with the paths suggesting that PD indication negatively impacts social support, which results in heightened grief reaction. However, our data do not allow us to test this causal pathway against alternatives. Finally, all data are based on self-report, and there are no biological data present to corroborate reported HIV symptoms or determine disease progression, nor objective data to indicate functional impairment due to grief, PD indication, or HIV disease. Despite these limitations, this study provides some of the first knowledge on the relationship between personality disorder indications and HRQoL in HIV positive adults using one of the largest datasets available of HIV-positive persons experiencing AIDS-related loss. The sample is comprised of women, and gay, bisexual and heterosexual men from diverse racial and ethnic backgrounds, and from geographically diverse regions of the U.S., thus increasing ecological validity and generalizability of findings.
The HIV epidemic in the U.S. has been characterized as having a significant psychiatric component due to the role of mental health problems in initial HIV infection, continued transmission risk behavior, poor treatment adherence, and disease progression (Treisman, Angelino, & Hutton, 2001). As many as 50% of those living with HIV have a mood or anxiety disorder, 25% have a current substance abuse or dependence disorder (Bing et al., 2001), and 26% a personality disorder (Treisman & Angelino, 2004). The presence of any of these disorders has been linked to slower rates of virologic suppression and faster rates of virologic failure after initiation of HAART (Pence, Miller, Gaynes, & Eron, 2007). Alternatively, HIV positive patients receiving psychiatric treatment have been shown to have slower disease progression and lower mortality than patients not receiving psychiatric treatment (Belanoff et al., 2005; Himelhoch, Moore, Treisman, & Gebo, 2004). However, although efficacy evidence is accumulating on a few specific behavioral interventions targeting mental health issues which not only reduce psychiatric symptoms, but also increase treatment adherence (Wyatt et al., 2004), decrease HIV transmission risk behavior (Sikkema et al., 2008; Wyatt et al., 2004), and improve health-related quality of life (Sikkema et al., 2005), there is a paucity of effective mental health interventions targeting HIV positive patients that are tailored to both meet patients' mental health needs and address key HIV-related themes. Our findings suggest such interventions to improve HRQoL should focus on (a) enhancing social support; (b) managing HIV infection (i.e., risk reduction, treatment adherence, healthy lifestyle choices); and (c) addressing grief, loss, and trauma. We are aware of only one intervention, Dialectical Behavior Therapy (DBT), that that has been modified to address personality disorders in the context of HIV infection (Wagner, Miller, Greene, & Winiarski, 2004), though empirical support for this modified intervention has yet to be established. It is essential, therefore, that as HIV infected patients live longer, their mental health needs are given adequate attention by providers, that mental health practitioners are part of HIV treatment teams, and that effective interventions for mental health problems, including personality disorders, are developed and/or tailored for the HIV context.
Acknowledgments
This research was supported by grants R01-MH54958, K23-MH076671, and P30-MH62294 (Center for Interdisciplinary Research on AIDS), from the National Institute of Mental Health; and T32-DA019426, from the National Institute on Drug Abuse. The authors gratefully acknowledge our community collaborations with the AIDS Resources Center for Wisconsin, the Madison AIDS Support Network, and the Callen-Lorde Community Health Center in New York City.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/hea/
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103(3):411–423. [Google Scholar]
- Aranda-Naranjo B. Quality of life in the HIV-positive patient: implications and consequences. Journal of the Association of Nurses in AIDS Care. 2004;15 5:20S–27S. doi: 10.1177/1055329004269183. [DOI] [PubMed] [Google Scholar]
- Belanoff JK, Sund B, Koopman C, Blasey C, Flamm J, Schatzberg AF, et al. A randomized trial of the efficacy of group therapy in changing viral load and CD4 counts in individuals living with HIV infection. International Journal of Psychiatry in Medicine. 2005;35:349–362. doi: 10.2190/4N6W-BUYY-CFNE-67XH. [DOI] [PubMed] [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry. 2001;58(8):721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Bing EG, Hays RD, Jacobson LP, Chen B, Gange SJ, Kass NE, et al. Health-related quality of life among people with HIV disease: Results from the multicenter AIDS cohort study. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation. 2000;9(1):55–63. doi: 10.1023/a:1008919227665. [DOI] [PubMed] [Google Scholar]
- Black DW, Blum N, Letuchy E, Doebbeling CC, Forman-Hoffman VL, Doebbeling BN. Borderline Personality Disorder and Traits in Veterans: Psychiatric Comorbidity, Healthcare Utilization, and Quality of Life Along a Continuum of Severity. CNS Spectrums. 2006;11(9):680–689. doi: 10.1017/s1092852900014772. [DOI] [PubMed] [Google Scholar]
- Bower JE, Kemeny ME, Taylor SE, Fahey JL. Cognitive processing, discovery of meaning, CD4 decline, and AIDS-related mortality among bereaved HIV-seropositive men. Journal of Consulting and Clinical Psychology. 1998;66(6):979–986. doi: 10.1037//0022-006x.66.6.979. [DOI] [PubMed] [Google Scholar]
- Burgess AP, Carretero M, Elkington A, Pasqual-Marsettin E, Lobaccaro C, Catalan J. The role of personality, coping style and social support in health-related quality of life in HIV infection. Quality of Life Research. 2000;9(4):423–437. doi: 10.1023/a:1008918719749. [DOI] [PubMed] [Google Scholar]
- Cella DF, McCain NL, Peterman AH, Mo F, Wolen D. Development and validation of the Functional Assessment of Human Immunodeficiency Virus Infection (FAHI) quality of life instrument. Quality of Life Research. 1996;5:450–463. doi: 10.1007/BF00449920. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The Global HIV/AIDS Pandemic, 2006. 2006 from Retrieved May 24, 2007 from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5531a1.htm.
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason BR, Sarason IG, editors. Social Support: Theory, Research, and Application. Boston, MA: Martinus Nijhoff Publishers; 1985. pp. 73–95. [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Cowdery JE, Pesa JA. Assessing quality of life in women living with HIV infection. AIDS Care. 2002;14(2):235–245. doi: 10.1080/09540120220104730. [DOI] [PubMed] [Google Scholar]
- Davis S. Clinical sequelae affecting quality of life in the HIV-infected patient. Journal of the Association of Nurses in AIDS Care. 2004;15 5:28S–33S. doi: 10.1177/1055329004269478. [DOI] [PubMed] [Google Scholar]
- Ekselius L, Lindstrom E, von Knorring L, Bodlund O, Kullgren G. SCID II interviews and the SCID Screen questionnaire as diagnostic tools for personality disorders in DSM-III-R. Acta Psychiatrica Scandinavica. 1994;90(2):120–123. doi: 10.1111/j.1600-0447.1994.tb01566.x. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB. Users guide for the structured clinical interview for DSM-IV disorders, research version (SCID-I, Version 2.0) 1996. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Users guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) 1997. [Google Scholar]
- Folkman S, Chesney M, Collette L, Boccellari A, Cooke M. Postbereavement depressive mood and its prebereavement predictors in HIV+ and HIV- gay men. Journal of Personality & Social Psychology. 1996;70(2):336–348. doi: 10.1037//0022-3514.70.2.336. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gielen A, McDonnell K, Wu A, O'Campo P, Faden R. Quality of life among women living with HIV: The importance violence, social support and self care behaviors. Social Science & Medicine. 2001;52(2):315–322. doi: 10.1016/s0277-9536(00)00135-0. [DOI] [PubMed] [Google Scholar]
- Gore-Felton C, Koopman C, Spiegel D, Vosvick M, Brondino M, Winningham A. Effects of Quality of Life and Coping on Depression among Adults Living with HIV/AIDS. Journal of Health Psychology. 2006;11(5):711–729. doi: 10.1177/1359105306066626. [DOI] [PubMed] [Google Scholar]
- Haller DL, Miles DR. Suicidal Ideation Among Psychiatric Patients with HIV: Psychiatric Morbidity and Quality of Life. AIDS and Behavior. 2003;7(2):101–108. doi: 10.1023/a:1023985906166. [DOI] [PubMed] [Google Scholar]
- Hansen NB, Cavanaugh CE, Vaughan EL, Connell CM, Tate DC, Sikkema KJ. The influence of personality disorder indication, social support, and traumatic grief on alcohol and cocaine use among HIV-positive adults coping with AIDS-related bereavement. AIDS and Behavior. doi: 10.1007/s10461-007-9308-6. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himelhoch S, Moore RD, Treisman GJ, Gebo KA. Does the presence of a current psychiatric disorder in AIDS patients affect the initiation of antiretroviral treatment and duration of therapy? JAIDS. 2004;37:1457–1463. doi: 10.1097/01.qai.0000136739.01219.6d. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Hutton HE, Treisman GJ. The role of personality in HIV risk behaviors: Implications for treatment. In: Cohen MA, Gorman JM, editors. Comprehensive Textbook of AIDS Psychiatry. New York, NY: Oxford; 2008. pp. 141–149. [Google Scholar]
- Jacobsberg L, Perry S, Frances A. Diagnostic agreement between the SCID-II screening questionnaire and the Personality Disorder Examination. Journal of Personality Assessment. 1995;65(3):428–433. doi: 10.1207/s15327752jpa6503_4. [DOI] [PubMed] [Google Scholar]
- Lau B, Gange SJ, Moore RD. Risk of non-AIDS-related mortality may exceed risk of AIDS-related mortality among individuals enrolling into care with CD4+ counts greater than 200 cells/mm3. Journal of Acquired Immune Deficiency Syndromes: JAIDS. 2007;44(2):179–187. doi: 10.1097/01.qai.0000247229.68246.c5. [DOI] [PubMed] [Google Scholar]
- Lennon MC, Martin JL, Dean L. The influence of social support on AIDS-related grief reaction among gay men. Social Science & Medicine. 1990;31(4):477–484. doi: 10.1016/0277-9536(90)90043-r. [DOI] [PubMed] [Google Scholar]
- Liu C, Johnson L, Ostrow D, Silvestre A, Visscher B, Jacobson LP. Predictors for Lower Quality of Life in the HAART Era Among HIV-Infected Men. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2006;42(4):470–477. doi: 10.1097/01.qai.0000225730.79610.61. [DOI] [PubMed] [Google Scholar]
- Mallinson RK. Grief work of HIV positive persons and their survivors. Nursing Clinics of North America. 1999;34(1):163–177. [PubMed] [Google Scholar]
- Mrus JM, Leonard AC, Yi MS, Sherman SN, Fultz SL, Justice AC, et al. Health-Related Quality of Life in Veterans and Nonveterans with HIV/AIDS. Journal of General Internal Medicine. 2006;21(s5):S39–S47. doi: 10.1111/j.1525-1497.2006.00644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott CH. The impact of complicated grief on mental and physical health at various points in the bereavement process. Death Studies. 2003;27(3):249–272. doi: 10.1080/07481180302887. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Klein DN. Testetest stability, mood-state dependence, and informantˆsubject concordance of the SCID-Axis II Questionnaire in a nonclinical sample. Journal of Personality Disorders. 1995;9(2):105–111. [Google Scholar]
- Palmer NB, Salcedo J, Miller AL, Winiarski M, Arno P. Psychiatric and social barriers to HIV medication adherence in a triply diagnosed methadone population. AIDS Patient Care & Stds. 2003;17(12):635–644. doi: 10.1089/108729103771928690. [DOI] [PubMed] [Google Scholar]
- Pence BW, Miller WC, Gaynes BN, Eron JJ. Psychiatric illness and virologic response in patients initiating highly active antiretroviral therapy. JAIDS. 2007;44:159–166. doi: 10.1097/QAI.0b013e31802c2f51. [DOI] [PubMed] [Google Scholar]
- Perseius KI, Andersson E, Asberg M, Samuelsson M. Health-related quality of life in women patients with borderline personality disorder. Scandinavian Journal of Caring Sciences. 2006;20(3):302–307. doi: 10.1111/j.1471-6712.2006.00408.x. [DOI] [PubMed] [Google Scholar]
- Piedmont RL, Sherman MF, Sherman NC, Williams JE. A First Look at the Structured Clinical Interview for DSM-IV Personality Disorders Screening Questionnaire: More Than Just a Screener? Measurement & Evaluation in Counseling & Development. 2003;36(3):150–160. [Google Scholar]
- Prigerson HO, Jacobs SC. Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In: Stroebe Margaret S, Hansson Robert O, Stroebe Wolfgang, Schut Henk., editors. Handbook of bereavement research: Consequences, coping, and care. 2001. [Google Scholar]
- Rando TA. The increasing prevalence of complicated mourning: The onslaught is just beginning. Omega: Journal of Death and Dying. 1992;26(1):43–59. [Google Scholar]
- Reed GM, Kemeny ME, Taylor SE, Visscher BR. Negative HIV-specific expectancies and AIDS-related bereavement as predictors of symptom onset in asymptomatic HIV-positive gay men. Health Psychology. 1999;18(4):354–363. doi: 10.1037//0278-6133.18.4.354. [DOI] [PubMed] [Google Scholar]
- Safren SA, Radomsky AS, Otto MW, Salomon E. Predictors of psychological well-being in a diverse sample of HIV-positive patients receiving highly active antiretroviral therapy. Psychosomatics. 2002;43(6):478–485. doi: 10.1176/appi.psy.43.6.478. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Hays RD, Fleishman JA, Vitiello B, Magruder KM, Bing EG, et al. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. American Journal of Psychiatry. 2000;157:248–254. doi: 10.1176/appi.ajp.157.2.248. [DOI] [PubMed] [Google Scholar]
- Sherr L, Hedge B, Steinhart K, Davey T, Petrack J. Unique patterns of bereavement in HIV: implications for counselling. Genitourinary Medicine. 1992;68(6):378–381. doi: 10.1136/sti.68.6.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Ghebremichael M, Kochman A, Tarakeshwar N, Meade CS, et al. A randomized controlled trial of a coping group intervention for adults with HIV who are AIDS bereaved: longitudinal effects on grief. Health Psychology. 2006;25(5):563–570. doi: 10.1037/0278-6133.25.5.563. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Kochman A, Tate DC, Difranceisco W. Outcomes from a randomized controlled trial of a group intervention for HIV positive men and women coping with AIDS-related loss and bereavement. Death Studies. 2004;28(3):187–209. doi: 10.1080/07481180490276544. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Meade CS, Kochman A, Lee RS. Improvements in health-related quality of life following a group intervention for coping with AIDS-bereavement among HIV-infected men and women. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care & Rehabilitation. 2005;14(4):991–1005. doi: 10.1007/s11136-004-2959-0. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Kalichman S, Hoffmann R, Koob J, Kelly J, Heckman T. Coping strategies and emotional wellbeing among HIV-infected men and women experiencing AIDS-related bereavement. AIDS Care. 2000;12(5):613–624. doi: 10.1080/095401200750003798. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Wilson PA, Hansen NB, Kochman A, Neufeld S, Ghebremichael MS, et al. Effects of a coping intervention on transmission risk behavior among people living with HIV/AIDS and a history of childhood sexual abuse. Journal of Acquired Immune Deficiency Syndromes. 2008;47:506–513. doi: 10.1097/QAI.0b013e318160d727. [DOI] [PubMed] [Google Scholar]
- Silverman GK, Jacobs SC, Kasl SV, Shear MK, Maciejewski PK, Noaghiul FS, et al. Quality of life impairments associated with diagnostic criteria for traumatic grief. Psychological Medicine. 2000;30(4):857–862. doi: 10.1017/s0033291799002524. [DOI] [PubMed] [Google Scholar]
- Singh K, Ochitill H. Personality Disorders. In: Fernandez F, Ruiz P, editors. Psychiatric aspects of HIV/AIDS. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 101–110. [Google Scholar]
- Spirig R, Moody K, Battegay M, De Geest S. Symptom management in HIV/AIDS: advancing the conceptualization. Advances in Nursing Science. 2005;28(4):333–344. doi: 10.1097/00012272-200510000-00005. [DOI] [PubMed] [Google Scholar]
- Sundin EC, Horowitz MJ. Horowitz's Impact of Event Scale evaluation of 20 years of use. Psychosomatic Medicine. 2003;65(5):870–876. doi: 10.1097/01.psy.0000084835.46074.f0. [DOI] [PubMed] [Google Scholar]
- Szaflarski M, Ritchey P, Leonard AC, Mrus JM, Peterman AH, Ellison CG, et al. Modeling the Effects of Spirituality/Religion on Patients' Perceptions of Living with HIV/AIDS. Journal of General Internal Medicine. 2006;21 5:S28–S38. doi: 10.1111/j.1525-1497.2006.00646.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treisman GJ, Angelino AF. The Psychiatry of AIDS: A guide to diagnosis and treatment. Baltimore, MD: The Johns Hopkins University Press; 2004. [Google Scholar]
- Treisman GJ, Angelino AF, Hutton HE. Psychiatric issues in the management of patients with HIV infection. JAMA. 2001;286:2857–2864. doi: 10.1001/jama.286.22.2857. [DOI] [PubMed] [Google Scholar]
- Vanderwerker LC, Prigerson HG. Social Support and Technological Connectedness as Protective Factors in Bereavement. Journal of Loss & Trauma. 2004;9(1):45–57. [Google Scholar]
- Wagner EE, Miller AL, Greene LI, Winiarski MG. Dialectical Behavior Therapy for substance abusers adapted for persons living with HIV/AIDS with substance use diagnoses and borderline personality disorder. Cognitive and Behavioral Practice. 2004;11:202–212. [Google Scholar]
- Wu AW. Quality of life assessment comes of age in the era of highly active antiretroviral therapy. AIDS. 2000;14(10):1449–1451. doi: 10.1097/00002030-200007070-00019. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Longshore D, Chin D, Carmona JV, Loeb TB, Myers HF, et al. The Efficacy of an Integrated Risk Reduction Intervention for HIV-Positive Women With Child Sexual Abuse Histories. AIDS and Behavior. 2004;8(4):453–462. doi: 10.1007/s10461-004-7329-y. Dec 2004. [DOI] [PubMed] [Google Scholar]
- Zhang B, El-Jawahri A, Prigerson HG. Update on bereavement research: evidence-based guidelines for the diagnosis and treatment of complicated bereavement. Journal of Palliative Medicine. 2006;9(5):1188–1203. doi: 10.1089/jpm.2006.9.1188. [DOI] [PubMed] [Google Scholar]


