Abstract
Background:
Autosomal recessive primary microcephaly (MCPH) is a model disease to study human neurogenesis. In affected individuals the brain grows at a reduced rate during fetal life resulting in a small but structurally normal brain and mental retardation. The condition is genetically heterogeneous with mutations in ASPM being most commonly reported.
Methods and results:
We have examined this further by studying three cohorts of microcephalic children to extend both the phenotype and the mutation spectrum. Firstly, in 99 consecutively ascertained consanguineous families with a strict diagnosis of MCPH, 41 (41%) were homozygous at the MCPH5 locus and all but two families had mutations. Thus, 39% of consanguineous MCPH families had homozygous ASPM mutations. Secondly, in 27 non-consanguineous, predominantly Caucasian families with a strict diagnosis of MCPH, 11 (40%) had ASPM mutations. Thirdly, in 45 families with a less restricted phenotype including microcephaly and mental retardation, but regardless of other neurological features, only 3 (7%) had an ASPM mutation. This report contains 27 novel mutations and almost doubles the number of MCPH associated ASPM mutations known to 57. All but one of the mutations lead to the use of a premature termination codon, 23 were nonsense mutations, 28 deletions or insertions, 5 splicing, and 1 was a translocation. Seventeen of the 57 mutations were recurrent. There were no definitive missense mutations found nor was there any mutation/phenotype correlation. ASPM mutations were found in all ethnic groups studied.
Conclusion:
This study confirms that mutations in ASPM are the most common cause of MCPH, that ASPM mutations are restricted to individuals with an MCPH phenotype, and that ASPM testing in primary microcephaly is clinically useful.
Our most defining feature as a species is our brain with its large size and cognitive functions leading to our great adaptability.1 Many genes are involved in the growth of the developing human brain but the identification of those which have a non-redundant and crucial role has proved difficult. Autosomal recessive primary microcephaly (MCPH) has emerged as a model disorder in which to seek such genes, as it is a condition where fetal brain growth is significantly reduced (as is head size throughout life), brain architecture is normal, and there are no apparent abnormalities in other body systems.2–4 Therefore the genes that cause MCPH may be expected to have an important, noticeable and non-redundant role in neurogenesis, but not other developmental processes.5 MCPH is also a diagnosable cause of mental retardation, and one with a substantial recurrence risk of one in four in subsequent children.
The current diagnostic criteria for MCPH are: congenital microcephaly more than −3 SD below age and sex means; mental retardation but no other neurological finding, such as spasticity, seizures, or progressive cognitive decline; normal height and weight, appearance, and results on chromosome analysis and brain scan.6 Despite this, MCPH still remains a clinical diagnosis of exclusion. Further, the recurrence risk of the MCPH phenotype after one affected child (with careful elimination of differential diagnoses) in a non-consanguineous family is one in eight, and in a consanguineous family one in six.7–9 Our first aim in designing this study was to be able to diagnose MCPH with greater accuracy, particularly at an early age, and to examine if the current diagnostic criteria accurately reflect the phenotypic spectrum of the disorder.
MCPH can be caused by recessive mutations in up to seven genes.4 6 Unexpectedly most of the known MCPH genes, CDK5RAP2, ASPM and CENPJ (better known as CPAP10), encode centrosomal proteins, highlighting the importance of the centrosome in neurogenesis.3 11–13 Despite this, a common mechanism explaining the role of the MCPH genes in neurogenesis has yet to emerge. All four known MCPH proteins are also present in the midbody (the microtubular structure linking daughter cells at the final stage of cytokinesis) and have apparently diverse roles: microcephalin in DNA repair and chromosome condensation, CDK5RAP2 and CENPJ in centriole/centrosome replication, and ASPM in modulating the plane of cytokinesis in neural precursors.14–19 Mutations in the ASPM gene at the MCPH5 locus on chromosome 1q31.3 have been considered the most common cause of MCPH.6 20 21 Our second aim in this study was to determine the frequency of ASPM mutations in microcephalic individuals, delineate the spectrum of mutations seen in the ASPM gene, and evaluate the utility of sequencing this gene in clinical practice.
The primary feature of MCPH is microcephaly—a reduced occipitofrontal head circumference (OFC)—which is an imperfect indicator of microencephaly (a small brain). Ideally volumetric magnetic resonance imaging (MRI) studies should be performed to quantitate brain volume, but this is not available in current clinical practice, whereas head circumference charts are tried, tested and useful.22–24 The choice of a cut-off value for microcephaly is important but arbitrary. Half of mentally retarded individuals are microcephalic7 25 and half of children with OFC of −2 SD or less have normal intelligence.26 To define microcephaly some authors use an OFC <2 SD below the mean for age and sex, which results in 2% of the general population being considered microcephalic.27 28 Others use <3 SD so that 0.1% of the general population are microcephalic and most do have mental retardation. 7 24 29 Added to this are probable ethnic variations and differences in norms between growth charts. Because of all of these considerations we use an OFC of more than −3 SD to define microcephaly in this study, realising that it could exclude a small number of true microcephalics but by corollary be unlikely to include people with normal brain volumes or intelligence.
METHODS
Three cohorts of microcephalic individuals were investigated. The first cohort (cohort 1) is of 99 consecutively ascertained consanguineous families of Pakistani or Arab origin seen by one author (CGW), the first 56 of which have been previously partly reported.6 Seventy-three families had multiple affected members and 26 consisted of a singleton child. No family was more distantly related than parents being second cousins. All fulfilled the current MCPH diagnostic criteria, with the exception that a brain MRI scan was only available in eight families (all showed no architectural anomalies). The second cohort (cohort 2) is of 27 non-consanguineous MCPH families of predominantly European origin, including five sib pairs. All had a normal brain scan and conformed to standard MCPH diagnostic criteria. The third cohort (cohort 3) is of 45 children (from 45 families) that was examined specifically to answer the questions, “Are the current MCPH clinical criteria too restrictive?” and its corollary, “Do ASPM mutations cause a wider phenotype than just MCPH?”. All 45 children had congenital microcephaly and mental retardation but there was no exclusion for the presence of epileptic fits, spasticity or other gross motor problems, growth problems, the presence of profound mental retardation or brain malformations. All had a brain scan examined by one author (WBD). The phenotypes of this cohort are given in supplemental table 1. DNA was obtained from all affected individuals and where possible their parents. Research ethics approval was given for these studies by the host institutions.
Table 1. All reported autosomal recessive primary microcephaly (MCPH) mutations in ASPM.
| Mutation | Predicted protein effect | Reported in more than one family? | Ethnic group | Reference |
| c.74delG | p.Arg25fs | No | Caucasian | This paper |
| c.297+1460_3391-242del21844 | Loss of microtubular binding domain | No | Caucasian | This paper |
| c.349C>T | p.Arg117X | Yes | Caucasian, Indian | 20, 37 |
| c.440delA | p.Lys147fs | No | Caucasian | This paper |
| c.577C>T | p.Gln193X | No | Caucasian | This paper |
| c.719_720delCT | p.Ser240fs | Yes | Pakistani | 3 |
| c.1152_1153delAG | p.Ser384fs | No | Caucasian | This paper |
| c.1179delT | p.Pro393fs | No | Caucasian | This paper |
| c.1258_1264delTCTCAAG | p.Ser420fs | Yes | Pakistani | 3* |
| c.1260_1266delTCAAGTC | p.Ser420fs | Yes | Pakistani | 21* |
| c.1366G>T | p.Glu456X | No | Turkish | This paper |
| c.1406_1413delATCCTAAA | p.Asn469fs | No | Caucasian | This paper |
| c.1590delA | p.Lys530fs | No | Caucasian | This paper |
| c.1727_1728delAG | p.Lys576fs | No | Yemeni | 37 |
| c.1959_1961delCAAA | p.Asn653fs | Yes | Saudi Arabian, Caucasian | This paper, 37 |
| c.1990C>T | p.Gln664X | No | Pakistani | 37 |
| c.2761-25A>G | Creates “AG” motif between branch site and splice acceptor site, exon 10 skipped, exon 11 frameshift with 30 novel aa then stop | No | Caucasian | This paper |
| c.2936+5G>T | Removes splice donor site, additional 2 aa then stop | No | Pakistani | 37 |
| c.2967G>A | p.Trp989X | No | Caucasian | This paper |
| c.3055C>T | p.Arg1019X | Yes | Caucasian | This paper |
| c.3082G>A | Removes splice donor site, additional 3 aa then stop | No | Pakistani | 37 |
| c.3188T>G | p.Leu1063X | No | Pakistani | This paper |
| c.3527C>G | p.Ser1176X | No | Jordanian | 37 |
| c.3663delG | p.Arg1221fs | Yes | Pakistani | 37 |
| c.3710C>G | p.Ser1237X | No | Caucasian | This paper |
| c.3741+1G>A | Removes splice donor site, additional 9 novel aa then stop | No | Caucasian | This paper |
| c.3796G>T | p.Glu1266X | No | African | This paper |
| c.3811C>T | p.Arg1271X | Yes | Dutch†, Asian | This paper, 37 |
| c.3978G>A | p.Trp1326X | Yes | Indian, Pakistani | 20, 21 |
| c.4581delA | p.Gly1527fs | No | Pakistani | 37 |
| c.4795C>T | p.Arg1599X | No | Pakistani | 37 |
| c.4855_4856delTA | p.Tyr1619fs | No | Pakistani | This paper |
| c.5136C>A | p.Tyr1712X | No | Pakistani | 37 |
| c.5149delA | p.Ile1717fs | No | Pakistani | 34 |
| c.6189T>G | p.Tyr2063X | No | Yemeni | 35 |
| c.6335_6336delAT | p.His2112fs | No | Pakistani | This paper |
| c.7489_7493delTATAT | p.Tyr2497fs | No | Caucasian | This paper |
| c.7761T>G | p.Tyr2587X | Yes | Pakistani | This paper, 3 |
| c.7782_7783delGA | p.Gln2594fs | Yes | Caucasian, Pakistani | This paper |
| c.7859_7860delAG | p.Gln2620fs | No | Arab | This paper |
| c.8130_8131delAA | p.Thr2710fs | No | Caucasian | This paper |
| c.8378delT | p.Met2793fs | Yes | Pakistani | This paper |
| c.8508_8509delGA | p.Gln2836fs | Yes | Pakistani | This paper, 34, 37 |
| c.8844delC | p.Ala2948fs | No | Caucasian | This paper |
| c.9118_9119insCATT | p.Tyr3040fs | No | Pakistani | 21 |
| c.9159delA | p.Lys3053fs | Yes | Pakistani | 3, 37 |
| c.9178C>T | p.Gln3060X | Yes | Indian, Caucasian | This paper, 20 |
| c.9190C>T | p.Arg3064X | Yes | Pakistani, Dutch | This paper, 37 |
| c.9238A>T | p.Leu3080X | Yes | Pakistani | This paper, 21 |
| c.9557C>G | p.Ser3186X | Yes | Pakistani | 21, 37 |
| c.9681delA | p.Thr3227fs | No | Pakistani | This paper |
| c.9730C>T | p.Arg3244X | No | Pakistani | 34 |
| c.9745_9746delCT | p.Leu3249fs | No | Pakistani | This paper |
| c.9754delA | p.Arg3252fs | No | Yemeni | 37 |
| c.9789T>A | p.Tyr3263X | No | Pakistani | This paper |
| c.9984+1G>T | Removes splice donor site, additional 29 novel aa then stop | No | Pakistani | 37 |
| c.10059C>A | p.Tyr3353X | No | Pakistani | 34 |
| Translocation | Loss of IQ and armadillo domains | No | European | 33 |
aa, amino acids.
*These are the same 7 base pair deletion mutation. †c.3811C>T has been found in a total of 3 out of 5 Dutch families with MCPH.
Bold face indicates MCPH associated with epileptic fits.
The position of each mutation is given as the number of bases from the start codon of the reference sequence NM_018136.3.
We sought evidence of linkage to ASPM in all of the consanguineous families. Polymorphic microsatellite marker or SNP chip analysis of all affected members was performed using standard methods and the results were examined for homozygosity at the MCPH5 locus.6 We sought a homozygous locus size of >1 cM, based on our previous study of recessive consanguineous families with proven recessive gene mutations.30 Of the total 99 consanguineous families, in 41 all affected members were homozygous for the MCPH5 locus (33 multi-affected families and eight singletons). In the remaining consanguineous families, affected family members were heterozygous for the MCPH5 locus in the case of singletons, or discordant for a MCPH5 haplotype in the multi-affected families. These families were assumed unlinked and the possibility of compound heterozygosity ignored.31 No linkage analysis was performed in the second two cohorts. The ASPM gene was sequenced using genomic DNA of one affected individual from each of the 41 consanguineous families that were homozygous at the MCPH5 locus, and all of the cohort 2 and 3 families. All exons and splice sites were included. Our recommended primers are given in supplemental table 2. All mutations found were shown to segregate faithfully in the family, although the degree of intrafamilial microcephaly varied, as previously reported.6
RESULTS
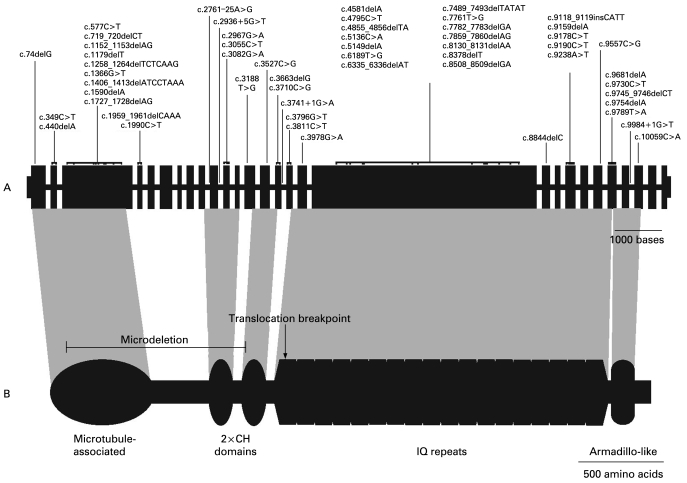
Of the consanguineous families in cohort 1, homozygous ASPM mutations were found in 39/41 of families (95% of families that were homozygous at the MCPH5 locus, 39% of all consanguineous families). Of the families that were homozygous at the MCPH5 locus with no ASPM mutations, one had a singleton affected child and one had an affected pair of first cousins. In cohort 2, of non-consanguineous, predominantly Caucasian individuals, ASPM mutations were found in 11/27 families (40%), and in 3/5 sib pairs. In this cohort 19 mutations were found: four were present in other cohorts, all but one led to a premature termination codon and no novel missense mutations were found. In three families the ASPM mutation was homozygous and the remainder were compound heterozygotes. In cohort 3, of 45 microcephalic individuals with a wider phenotype we found mutations in three families (7%). One consanguineous and one non-consanguineous singleton each had a homozygous nonsense mutation. Both of these homozygous mutations were present in other cohorts. A child from a third family carried two heterozygous protein truncating mutations. The mutations from all three cohorts and all previously reported mutations are described in table 1 and shown in fig 1.
Figure 1.
ASPM gene, protein and sites of autosomal recessive primary microcephaly (MCPH) mutations. (A) The exon/intron structure of the ASPM gene. Exons are scaled relative to each other, with exon 18 being the largest at 4.7 kb. Introns vary significantly in size, but for clarity are all shown as having the same arbitrary size. The position of the reported mutations is indicated, with italicised text denoting splicing mutations. All mutations are detailed in table 1. (B) The known and predicted domains of the ASPM protein: a microtubule binding domain; two calponin homology (CH) domains which are possibly responsible for transportation of the ASPM protein to the spindle poles; a region of 81 IQ/calmodulin binding domains; and a conserved armadillo-like C-terminal domain of unknown significance. The regions of the ASPM protein affected by the previously reported translocation breakpoint (Pichon et al33) and the microdeletion first reported here are shown by an arrow and a bar, respectively.
DISCUSSION
This work brings the total number of different ASPM mutations reported to 57. Of these mutations 17 are recurrent. All but one of the mutations reported here and previously is predicted to lead to the use of a premature termination codon in the ASPM gene (which has no common splice variants) (table 1). Of the 57 mutations 23 were nonsense mutations, 28 were small deletions or insertions leading to a change in the reading frame, and five were splice site mutations again leading to the use of a premature stop codon. In one family we found a large deletion of 21 844 bases with the loss of exons 2 through to 13, but which leaves the open reading frame intact. Cloning of the deletion showed a loss of part of intron 1 through to intron 13, and the breaks did not occur in repeat elements. A similar single large deletion has been reported in the MCPH1 microcephalin gene32 and a translocation dissecting ASPM has previously been reported.33 The mutations were spread throughout the gene with no hot-spots (fig 1). There were no clear cut genotype/phenotype correlations of head size centile, degree of mental retardation (profound mental retardation was not seen, nor has it been reported in ASPM MCPH) or the presence of epileptic fits with mutation type or position within the gene.6 However, only a few individuals in these cohorts have had an ethically appropriate IQ test. The findings that the mutations were spread throughout the ASPM gene, that all but one of the mutations led to premature protein truncation, and that there are no genotype/phenotype correlations, argue that the disease mechanism causing MCPH is nonsense mediated decay of the ASPM mRNA leading to a pronounced reduction of the protein in neuroepithelial cells.16 In support of this, two studies have looked at non-neuroepithelial cells from ASPM MCPH patients and found a combination of absent or much reduced levels of ASPM protein and truncated versions of ASPM still containing the C-terminus.14 Presumably these truncated forms of ASPM arise from atypical splicing events and/or translation re-initiation. If these results can be extrapolated to neuroepithelial cells undergoing neurogenic mitosis, then this argues that the MCPH phenotype only occurs when ASPM falls below a critical level.
The role of missense mutations in ASPM remains obscure. We found numerous sequence variants in study families whether they had a premature protein truncating mutation or not (supplemental table 3). Some of these were known single nucleotide polymorphisms (SNPs), some we found recurrently and some were unique to one family, but none would be predicted to cause a loss of function. For the majority of families we could show that parents were heterozygous for these sequence variants, at least ruling out a dominant negative effect (and the region is not known to be imprinted). An ASPM missense mutation has been previously reported,34 and while it was the only mutation found in an MCPH5 linked family it occurred in one of the 70+ IQ domains of the ASPM protein, and its functional significance has not been investigated. So at present there is no evidence that missense ASPM mutations cause MCPH; however, it remains a possibility that missense mutations may cause another phenotype or could cause autosomal dominant microcephaly.
The first aim of this study was to re-examine the current MCPH clinical criteria. We thought this necessary as the initial MCPH criteria were defined in a research setting and we wanted to see if these criteria were sufficiently robust to allow early and accurate diagnosis. We achieved this by examining which cases had ASPM mutations. Cohort 1 and 2 were ascertained using the current criteria and in both a similar high rate of ASPM mutations was found (39% and 40%, respectively). This is particularly important as the two cohorts have different ethnic and geographical origins as well as cohort 1 being inbred in contrast to cohort 2, which was not. So in these two diverse groups the current criteria was an excellent discriminator for ASPM mutations. If these data are taken with previous segregation and clinical analyses which suggest that three quarters of carefully selected cases of primary microcephaly have MCPH, we can conclude that ASPM is the most common cause of MCPH and accounts for one half of Asian and European Caucasian MCPH cases. In contrast, when diagnostic criteria were relaxed (as in cohort 3) to microcephalic children with mental retardation, but not fulfilling the other MCPH criteria, significantly fewer mutations were found (7%, p<0.01 Student t test, 2 df). Retrospective phenotype analysis showed ASPM mutations were only found in individuals meeting MCPH criteria (3/13). In those who did not meet the criteria (n = 32) no ASPM mutations were found.
Web resources
OMIM On-line Mendelian Inheritance in Man:
We suggest one modification to add to the MCPH criteria, that while epileptic fits are not common they should not be an excluding factor. In cohort 1 there were tonic–clonic fits in some affected individuals in two families with ASPM mutations; two out of three affected in one family and both children in a second family. The onset was after the first year of life, status epilepticus did not occur, there was no regression associated with the fits and they were easily controlled with standard medications. A family with primary microcephaly and epileptic fits and a protein truncating ASPM mutation has been previously reported.35 The ASPM mutations that have been associated with epileptic fits are shown in table 1. A remaining clinical problem is the necessity for mental retardation in the diagnostic criteria of MCPH. This cannot always be reliably diagnosed in the first few years of life, although a clinician may be asked to comment on the diagnosis and prognosis of a microcephalic baby or young child. Significant microcephaly (OFC <−4 SD) alone can co-occur with normal intelligence in a number of settings—for example, Bloom syndrome (OMIM 210900), osteodysplastic primordial dwarfism due to pericentrin mutations (OMIM 210720), and autosomal dominant microcephaly (OMIM 156580).36 There are no reports of ASPM mutations associated with microcephaly and normal intelligence, and we found no examples of this in the families of this study. Therefore, positive ASPM testing in a microcephalic baby would be predictive of mental retardation.
The data in this study establish ASPM mutations as the most common cause of MCPH, and that there are no genotype/phenotype correlations. The data also indicate that ASPM mutations are restricted to individuals with an MCPH phenotype, and suggest ASPM testing in primary microcephaly is clinically of use.
Acknowledgments
We thank the Wellcome Trust for funding and all of the families and their clinicians for their help with this study. The Wellcome Trust Diabetes and Inflammation Laboratory, Cambridge provided genomic sequencing support.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
REFERENCES
- 1.Darwin C. The descent of man and selection in relation to sex Princeton: Princeton University Press, 1981 [Google Scholar]
- 2.Mochida GH, Walsh CA. Molecular genetics of human microcephaly. Curr Opin Neurol 2001;14:151–6 [DOI] [PubMed] [Google Scholar]
- 3.Bond J, Roberts E, Mochida GH, Hampshire DJ, Scott S, Askham JM, Springell K, Mahadevan M, Crow YJ, Markham AF, Walsh CA, Woods CG. ASPM is a major determinant of cerebral cortical size. Nat Genet 2002;32:316–20 [DOI] [PubMed] [Google Scholar]
- 4.Woods CG, Bond J, Enard W. Autosomal recessive primary microcephaly (MCPH): a review of clinical, molecular, and evolutionary findings. Am J Hum Genet 2005;76:717–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox J, Jackson AP, Bond J, Woods CG. What primary microcephaly can tell us about brain growth. Trends Mol Med 2006;12:358–66 [DOI] [PubMed] [Google Scholar]
- 6.Roberts E, Hampshire DJ, Pattison L, Springell K, Jafri H, Corry P, Mannon J, Rashid Y, Crow Y, Bond J, Woods CG. Autosomal recessive primary microcephaly: an analysis of locus heterogeneity and phenotypic variation. J Med Genet 2002;39:718–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bundey S, Carter CO. Recurrence risks in severe undiagnosed mental deficiency. J Ment Defic Res 1974;18:115–34 [DOI] [PubMed] [Google Scholar]
- 8.Bundey S. Genetics and neurology , 2nd ed.London: Churchill Livingstone, 1992 [Google Scholar]
- 9.Tolmie JL, McNay M, Stephenson JB, Doyle D, Connor JM. Microcephaly: genetic counselling and antenatal diagnosis after the birth of an affected child. Am J Med Genet 1987;27:583–94 [DOI] [PubMed] [Google Scholar]
- 10.Hung LY, Tang CJ, Tang TK. Protein 4.1 R-135 interacts with a novel centrosomal protein (CPAP) which is associated with the gamma-tubulin complex. Mol Cell Biol 2000;20:7813–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson AP, Eastwood H, Bell SM, Adu J, Toomes C, Carr IM, et al. Identification of microcephalin, a protein implicated in determining the size of the human brain. Am J Hum Genet 2002;71:136–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bond J, Roberts E, Springell K, Lizarraga SB, Scott S, Higgins J, Hampshire DJ, Morrison EE, Leal GF, Silva EO, Costa SM, Baralle D, Raponi M, Karbani G, Rashid Y, Jafri H, Bennett C, Corry P, Walsh CA, Woods CG. A centrosomal mechanism involving CDK5RAP2 and CENPJ controls brain size. Nat Genet 2005;37:353–5 [DOI] [PubMed] [Google Scholar]
- 13.Zhong X, Pfeifer GP, Xu X. Microcephalin encodes a centrosomal protein. Cell Cycle 2006;5:457–8 [DOI] [PubMed] [Google Scholar]
- 14.Kouprina N, Pavlicek A, Collins NK, Nakano M, Noskov VN, Ohzeki J, Mochida GH, Risinger JI, Goldsmith P, Gunsior M, Solomon G, Gersch W, Kim JH, Barrett JC, Walsh CA, Jurka J, Masumoto H, Larionov V. The microcephaly ASPM gene is expressed in proliferating tissues and encodes for a mitotic spindle protein. Hum Mol Genet 2005;14:2155–65 [DOI] [PubMed] [Google Scholar]
- 15.Cho JH, Chang CJ, Chen CY, Tang TK. Depletion of CPAP by RNAi disrupts centrosome integrity and induces multipolar spindles. Biochem Biophys Res Commun 2006;339:742–7 [DOI] [PubMed] [Google Scholar]
- 16.Fish JL, Kosodo Y, Enard W, Pääbo S, Huttner WB. Aspm specifically maintains symmetric proliferative divisions of neuroepithelial cells. Proc Natl Acad Sci USA 2006;103:10438–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Driscoll M, Jackson AP, Jeggo PA. Microcephalin: a causal link between impaired damage response signalling and microcephaly. Cell Cycle 2006;5:2339–44 [DOI] [PubMed] [Google Scholar]
- 18.Trimborn M, Schindler D, Neitzel H, Hirano T. Misregulated chromosome condensation in MCPH1 primary microcephaly is mediated by condensin II. Cell Cycle 2006;5:322–6 [DOI] [PubMed] [Google Scholar]
- 19.Graser S, Stierhof YD, Nigg EA. Cep68 and Cep215 (Cdk5rap2) are required for centrosome cohesion. J Cell Sci 2007;120:4321–31 [DOI] [PubMed] [Google Scholar]
- 20.Kumar A, Blanton SH, Babu M, Markandaya M, Girimaji SC. Genetic analysis of primary microcephaly in Indian families: novel ASPM mutations. Clin Genet 2004;66:341–8 [DOI] [PubMed] [Google Scholar]
- 21.Gul A, Hassan MJ, Mahmood S, Chen W, Rahmani S, Naseer MI, Dellefave L, Muhammad N, Rafiq MA, Ansar M, Chishti MS, Ali G, Siddique T, Ahmad W. Genetic studies of autosomal recessive primary microcephaly in 33 Pakistani families: novel sequence variants in ASPM gene. Neurogenetics 2006;7:105–10 [DOI] [PubMed] [Google Scholar]
- 22.Opitz JM, Holt MC. Microcephaly: general considerations and aids to nosology. J Craniofac Genet Dev Biol 1990;10:175–204 [PubMed] [Google Scholar]
- 23.Paul AA, Ahmed EA, Whitehead RG. Head circumference charts updated. Arch Dis Child 1986;61:927–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abuelo D. Microcephaly syndromes. Semin Pediatr Neurol 2007;14:118–27 [DOI] [PubMed] [Google Scholar]
- 25.Herbst DS, Baird PA. Nonspecific mental retardation in British Columbia as ascertained through a registry. Am J Ment Defic 1983;87:506–13 [PubMed] [Google Scholar]
- 26.Watemberg N, Silver S, Harel S, Lerman-Sagie T. Significance of microcephaly among children with developmental disabilities. J Child Neurol 2002;17:117–22 [DOI] [PubMed] [Google Scholar]
- 27.Menkes JH. Textbook of child neurology Philadelphia: Lea and Febiger, 1974:148–50 [Google Scholar]
- 28.Aicardi J. Diseases of the nervous system in childhood , 2nd ed.London: Mac Keith Press, 1998 [Google Scholar]
- 29.Book JA, Schut JW, Reed SC. A clinical and genetical study of microcephaly. Am J Mental Defic 1953;57:637–60 [PubMed] [Google Scholar]
- 30.Woods CG, Cox J, Springell K, Hampshire DJ, Mohamed MD, McKibbin M, Stern R, Raymond FL, Sandford R, Malik Sharif S, Karbani G, Ahmed M, Bond J, Clayton D, Inglehearn CF. Quantification of homozygosity in consanguineous individuals with autosomal recessive disease. Am J Hum Genet 2006;78:889–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miano MG, Jacobson SG, Carothers A, Hanson I, Teague P, Lovell J, Cideciyan AV, Haider N, Stone EM, Sheffield VC, Wright AF. Pitfalls in homozygosity mapping. Am J Hum Genet 2000;67:1348–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garshasbi M, Motazacker MM, Kahrizi K, Behjati F, Abedini SS, Nieh SE, Firouzabadi SG, Becker C, Rüschendorf F, Nürnberg P, Tzschach A, Vazifehmand R, Erdogan F, Ullmann R, Lenzner S, Kuss AW, Ropers HH, Najmabadi H. SNP array-based homozygosity mapping reveals MCPH1 deletion in family with autosomal recessive mental retardation and mild microcephaly. Hum Genet 2006;118:708–15 [DOI] [PubMed] [Google Scholar]
- 33.Pichon B, Vankerckhove S, Bourrouillou G, Duprez L, Abramowicz MJ. A translocation breakpoint disrupts the ASPM gene in a patient with primary microcephaly. Eur J Hum Genet 2004;12:419–21 [DOI] [PubMed] [Google Scholar]
- 34.Gul A, Tariq M, Khan MN, Hassan MJ, Ali G, Ahmad W. Novel protein-truncating mutations in the ASPM gene in families with autosomal recessive primary microcephaly. J Neurogenet 2007;21:153–63 [DOI] [PubMed] [Google Scholar]
- 35.Shen J, Eyaid W, Mochida GH, Al-Moayyad F, Bodell A, Woods CG, Walsh GA. ASPM mutations identified in patients with primary microcephaly and seizures. J Med Genet 2005;42:725–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rauch A, Thiel CT, Schindler D, Wick U, Crow YJ, Ekici AB, van Essen AJ, Goecke TO, Al-Gazali L, Chrzanowska KH, Zweier C, Brunner HG, Becker K, Curry CJ, Dallapiccola B, Devriendt K, Dörfler A, Kinning E, Megarbane A, Meinecke P, Semple RK, Spranger S, Toutain A, Trembath RC, Voss E, Wilson L, Hennekam R, de Zegher F, Dörr HG, Reis A.Mutations in the pericentrin (PCNT) gene cause primordial dwarfism. Science 2008;319:816–19 [DOI] [PubMed] [Google Scholar]