Abstract
The ultimate goal of antihypertensive therapy is cardiovascular risk reduction. As lowering blood pressure per se reduces risk for myocardial infarction only by 20% - 25%, it is obvious that a better protection is needed. An optimal strategy to reduce risk in hypertensives may include lifestyle modification, promotion of adherence to therapy, early and aggressive target levels achievement by appropriate drug choice. Clinical trial data suggest that RAAS blockers can reduce the risk at least partly independently of BP lowering.
In addition, as hypertension is associated with a constellation of other risk factors, the global risk reduction is nowadays going to become the gold standard in therapy. The most common and important coexisting risk factor is hypercholesterolemia. This is not simply a co-existence but there is an independent and causal relationship between lipids and hypertension and there is a physiologic rationale and evidence for statins use especially in patients with complicated hypertension or in patients with more than two risk factors.
So, whilst blood pressure lowering is undoubtedly beneficial, we have to focus on the global cardiovascular risk. We must go beyond blood pressure and the most effective way to go "beyond BP" is to add a statin.
Keywords: blood pressure, cardiovascular risk, statin
Hypertension has been recognized as a major public health issue. The association of hypertension with cardiovascular (CV) morbidity and mortality is well established. Abundant epidemiological data have shown that the risk of CV disease rises with increasing blood pressure (BP) levels, starting at ≥115/75 mm Hg, in a strong, independent, graded and continuous manner. Traditionally the ultimate goal of antihypertensive therapy is the prevention of atherosclerotic cardiovascular (CV) and renal complications and there is no doubt that antihypertensive therapy reduces CV risk. Numerous clinical trials have shown that lowering blood pressure (BP) reduces CV risk by 20% - 25% for myocardial infarction, 35%-40% for stroke and by 50% for heart failure. The medical society cannot be proud for this low reduction. It is obvious that a better protection is needed. Today a target of 65 % risk reduction in hypertensives as well as an 80 % in general population seems feasible. Yet, the precise physiologic mechanisms by which hypertension increases CV risk, and antihypertensive therapy lowers the risk, remain unclear1,2,3.
Despite the robust association of hypertension with CV risk in populations, some patients with hypertension do not experience CV events during long life spans and CV events are observed to occur in normotensive individuals. It is nowadays widely accepted that hypertension is associated with a constellation of other CV risk factors, such as the metabolic syndrome components, endothelial dysfunction, arterial stiffness and nephropathy, indicating its part in a multifactorial disease process. Although atherosclerosis usually presents clinically in middle aged, the underlying pathology begins in the first decade of life. Hypertension starts in the childhood and from the beginning and in all stages is associated with other CV risk factors. Clinical trial data suggest that some antihypertensive therapies, particularly those that block the renin-angiotensin-aldosterone system (RAAS), can reduce CV disease risks at least partly independently of BP lowering although a major controversy involves this question. Hypertension remains extremely common, with an estimated prevalence of 30% of the adult population, of whom only about 30% have their BP controlled to the recommended level of <140/90 mm Hg. Even today, hypertension is not yet under control and the reason for that is because it is undercontrolled. Aspects concerning adherence and target BP achievement are of great importance2,3.
An optimal strategy to reduce CV risk may include lifestyle modification, promoting adherence to early and aggressive target levels achievement, appropriate drug choice and especially a global risk reduction. In this review article we are referring to the significance of these topics with emphasis at global risk reduction as today a significant shift is observed over this topic in hypertension therapy.
Lifestyle modification
As atherosclerosis begins from childhood it is necessary at first to remind the need for healthy lifestyle to prevent hypertension development (Primordial Prevention). Interventions to alter CV risk and relative complications can either target the total population or the small proportion of individuals at high risk. Population healthy lifestyle modification is necessary and more effective both for prevention and treatment of hypertension and prevention and treatment of atherosclerotic complication as well. Note that the high risk approach protects only susceptible individuals while a population approach controls the cause of the disease progress. Such high-risk strategies that aim to achieve a large risk reduction in people at high total CV risk are more effective than strategies based solely on elevated levels of single risk factors. However, unless such strategies are applied to a large proportion of the population, they are unlikely to have a large overall impact on population levels of disease. In contrast, repeated population surveys have shown that even modest improvements in population risk –factor levels can have large effects on national CVD mortality rates over a relatively short period of time. Population strategies are cost-effective, they address the underlying causes of CVD and they reduce the number of people requiring drug treatment in future years. To reduce the increasing global burden of CVD, effective high-risk strategies need to be supplemented by population strategies focused on such factors as tobacco and diet, particularly in developing countries in which widespread use of risk-reducing therapies may not me feasible.
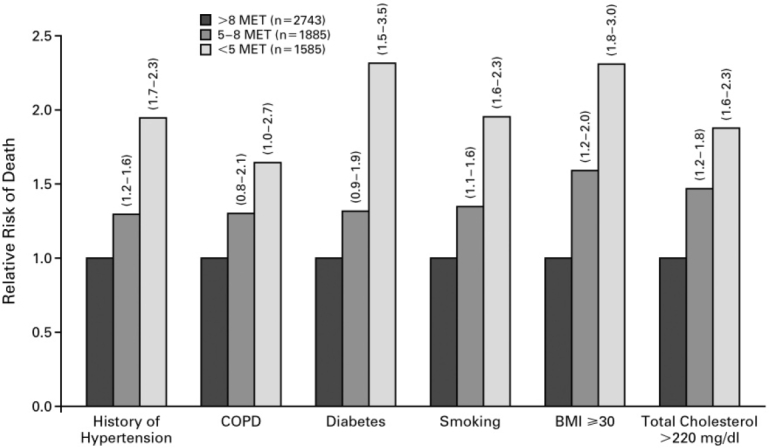
Efforts to BP control and relative risk reduction must primarily focus on non-pharmacological approach. All guidelines recommend weight control, reduced salt intake, reduced alcohol consumption and regular exercise. The importance of exercise can be seen on Fig 1. Exercising hypertensives achieving a good physical performance (exercise tolerance >8 METS) have almost halved their mortality risk. Furthermore, an abnormal BP answer during an exercise stress test seems to be a good predictor of hypertension development4-9.
Figure 1. Relative risk of mortality from any cause among subjects with various risk factors and exercise capacities (95% confidence intervals for the relative risks in parentheses).BMI: Body Mass Index, COPD: Chronic Obstructive Pulmonary Disease; modified from Myers and colleagues (8).
Adherence concepts
Strategies improving adherence are of great importance. Poor adherence is considered as a severe risk factor for atherosclerosis and it is a major factor for why hypertension and the relative risk are not yet under control. Good adherence reduces CV risk. The best adherence has been observed in treatment with ARBs. It is worth to mention that adherence decreases rapidly during the first 3-6 months of treatment. This period of treatment time is critical as after that period the proportion of patients fully and partially adherent increases significantly or it is at least stabilized. The percentage of fully adherent patients is approximately 30 % after 1 year and around 20 % to 30 % are partially adherent. Adherence is strongly associated with goal attainment, especially in persons with mild hypertension. Poor adherence and compliance is not only a matter of patient and drug side effects but it is a concern for physicians, providers and policy services as well. In every day practice we are not doing everything we can10.
Early and aggressive BP lowering
As both atherosclerosis and hypertension begin in childhood, early and aggressive BP lowering is mandatory as it leads to long-term CV risk reduction. The recently published TROPHY trial has clearly demonstrated that treatment of Pre-Hypertension prevents hypertension development. The early intervention reduces CV risk. There is a strong impact of high normal BP on CVD risk. According to Framingham study data, 31% of strokes occur in patients with normal or high normal hypertension. In VALUE study the benefit gained by amlodipine as compared to valsartan is due to rapid reduction and control of hypertension from the beginning of therapy11,12,13. So in reducing BP there is no time to waste: the earlier the better.
Treatment to Target levels
There is not doubt today that lower is better regarding BP reduction and CV outcomes. The HOT study has clearly demonstrated this hypothesis. Obviously it is more necessary to some categories such as diabetic, CKD, or CAD patients. In this field there is no doubt today, that the lower is the better, and this target can be achieved usually using combinations of drugs. However only a minority of patients in day-to-day practice follows or achieves the need targets for BP control in the family practice where most hypertensives are managed or even in the "experts" clinics. It is well accepted that only 30% of hypertensives are treated at target level although almost all patients can achieve the target with the appropriate combination of drugs. Today the failure to titrate or combine medications despite the knowledge that the patient has not achieved the goal BP, represents clinical inertia and must be overcome. Anecdotally, only nephrologists have shown a long-standing interest in good BP control, and have recognized that lower blood pressures are crucial to maintain renal function in patients with chronic renal disease and malignant hypertension. 14,15,16,17,18
Drug Choice
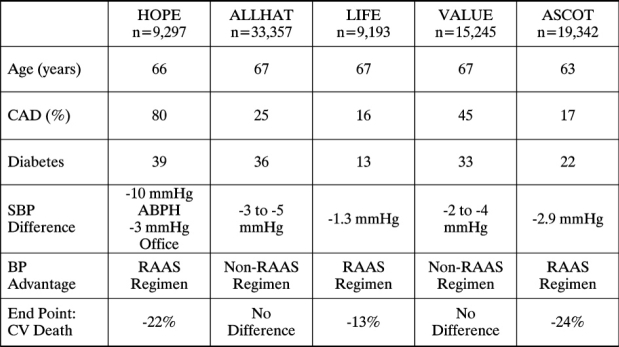
According to ESH / ESC Guidelines the main benefit with antihypertensive therapy results by BP lowering per se. Although the majority of existing evidence indicates that the benefit of antihypertensive therapy is gained mainly by BP lowering per se, there is a strong pathophysiologic basis indicating that some drug categories may be preferred in the context of reducing CV risk. So, beyond the adverse effects ( quality of life is an important parameter we must respect ) and compelling indications, drug choice must be based on the possible beneficial pleiotropic effects on metabolic profile and vasculature. Beyond early, aggressive and optimal BP control, a vascular protection policy dictates optimal RAAS blockade. Kidney disease trials provide strong evidence and a lot of important lessons. Modulation of RAAS along with BP lowering is probably the best root for an optimal CV risk reduction11,19,20,21,22,23. A recently published meta-analysis (Table 1) has clearly demonstrated this22. As it is seen in this table a significant CV death reduction (22 %, 13 % and 24 % respectively) was observed in studies HOPE, LIFE, ASCOT where the BP advantage was gained by a RAAS regimen, while there was not any benefit in studies VALUE and ALLHAT in which the benefit was gained by a non RAAS regimen.
Table 1. RAAS versus Non-RAAS regimens on End Poind of CV Death.
Global CV reduction:An important therapeutic Target
Nowadays a significant shift appears in the literature regarding the whole problem of hypertension. Recognition of the interaction of cardiovascular risk factors led to a new definition and consequently treatment of hypertension as the global cardiovascular risk reduction led to new concepts and therapeutic opportunities. In fact today hypertension is completely reconsidered.
a. New Definition and Classification of Hypertension
A new definition for hypertension has recently been published which moves beyond the tradition of equating hypertension solely with elevated BP levels and instead integrates CV risk factors, early disease markers and overt CV disease into the definition and classification. Hypertension is not equating solely with elevated BP levels. The word hypertension must be almost deleted. It has no meaning. This shift in focus is intended to assist clinicians in assessing global CV risk, regardless of BP level and in identifying and managing hypertension at an earlier disease progress24.
Hypertension is a progressive CV disorder that leads to functional and structural vascular abnormalities that damage the vasculature, heart, kidneys, brain and other organs leading to morbidity and premature death . Since early markers of CV disease are often present even before BP elevation is observed, hypertension cannot be classified solely by discrete BP thresholds. Individuals must only be considered as normotensives if they have resting BP levels usually <120/80 mmHg and parallelly lack any CV risk factors, any identifiable early risk markers and any target-organ damage. These new data regarding hypertension have lately raised the question on whether BP is really a cause or a consequence of CV disease. This last question sounds strange and somewhat mysterious but it is really very attractive. In science, as a romance, things are often beautiful when they are at least somewhat mysterious. This is the beauty of medical science!
Hypertension is best described by changes in the arterial wall rather than solely by elevated BP levels. This assumes that BP elevation is an insensitive and nonspecific surrogate for the vascular changes and that the changes in the artery wall better represent the disease process. By utilizing CV status in addition to BP, clinicians will likely put a greater emphasis on identifying and managing hypertension at an earlier stage in the disease process, and focusing sharper on treatment aimed towards the protection of arterial wall and prevention of BP levels elevation. Designating individuals with high-risk profiles and BP levels <140/90 mmHg as hypertensive, for example, assists providers and patients in recognizing that a disease state already exists, allowing easier identification of individuals with early hypertensive CV disease. Identifying and controlling coexisting modifiable CV risk factors is critical and hypertension screening should be part of the overall global risk assessment. The new definition of hypertension thus offers a more global riskbased approach for identifying those individuals at any level of BP who have a reasonable likelihood of developing future CV events. By identifying hypertension in individuals with high-risk profiles, independently of BP levels and by focusing on the level of the blood vessel, the overall care of patients at risk for CV events should significantly improve.
The new definition and classification of hypertension has recently raised questions regarding the sensitivity of BP as a marker or risk factor for CV events. As a result there is a shift in antihypertensive therapy primarily focusing on global CV reduction rather than BP levels per se. Global risk reduction is probably the most important target of hypertension treatment.
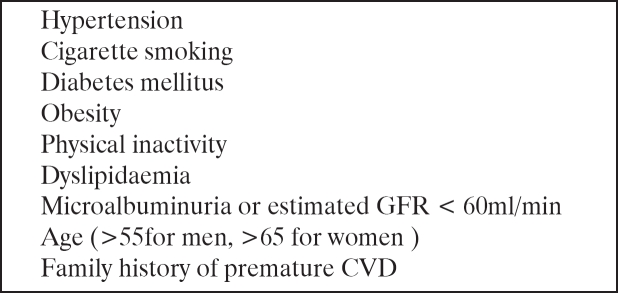
In clinical practice, a significant shift in hypertension therapy is the recognition of the interaction of CV risk factors and application of new treatment strategies. The meaning of global CV risk reduction is very important. Hypertension from the beginning to all stages is associated with other CV risk factors and this global risk profile is essential for CVD prevention. The most important risk factors are shown on Table 2. These nine factors shown on the table account for the 90 % of CVD.
Table 2. Global Risk Profile for CVD.
The multiple risk factor patients can be identified by history, physical examination, biomarkers, risk calculators and imaging modalities. Several tools have been developed to help identify individuals at CV risk. CV risk assessments are usually carried out using risk charts or calculators that are based on epidemiologic data. Antihypertensive therapy should therefore be coordinated with other preventive measures; all strategies used to prevent or manage CV risk factors or early disease markers should be considered as part of the overall regimen to reduce global risk25-29.
b. The Physiologic Rationale and Evidence for Treating Concomitant Risk Factors.
The most common and probably most important coexisting risk factor with hypertension is dyslipidemia. Hypertension and dyslipidemia occur commonly in unison than cannot be accidental, as almost 65 % of hypertensives have also high cholesterol. This is not simply a co-existence but there is a causal interaction among these two factors. There is an independent and causal relationship (not simply association) between baseline lipids and hypertension. This relation is not constant. Effect of high BP is more prominent in low cholesterol levels while effect of cholesterol is more prominent in lower BP levels. Note that 10% BP plus 10% lipids reduction leads to 45% CV risk reduction (10+10=45!!). Hypercholesterolemia increase AT1 receptors expression and this effect is blocked by statins. On the other hand AII increases LOX-1 receptors expression an effect which is blocked by RAAS blockade. The presence of dyslipidemia increases the risk of developing hypertension in later life. Thus, multiple risk factors for cardiovascular disease generate the vascular disease phenotype. High BP and high cholesterol are often thought of as separate "disease entities" and the synergy of these risk factors in the pathogenesis of vascular disease has been poorly recognized and certainly underestimated. At the biological level, there is considerable potential for blood pressure to augment the potency of LDL-C in mediating vascular damage. This can occur via enhanced oxidation of LDL-C and the enhanced pressure-mediated transmigration of LDL-C through the vessel wall. Similarly, LDL-C by virtue of its adverse effects on endothelial function, has the capacity to generate and/or augment the development of hypertension. This effect has been observed in children with familial hypercholesterolaemia and in adults with more modest elevations of LDL-C. Regarding dyslipidemia and development of hypertension, men who are in the highest quintile of TC, non-HDL-C and TC/ HDL-C ratio, have increased risk of developing hypertension. Men in the highest quintile of HDL-C have a 32 % decreased risk of developing hypertension. Moreover, by influencing large and small artery function, LDL-C can modify central aortic hemodynamics and pressures, thereby contributing to pressure –mediated vascular injury. Finally, in the later stages of vascular disease, there is a clear association between the vulnerable lipid-rich plaque rupture and haemodynamic stress in the generation of plaque rupture and the onset of clinical events.
This synergism between LDL-C and elevated blood pressure mediating vascular dysfunction, highlights its importance in the spectrum of hypertensive vascular disease, ranging from early disturbances in endothelial function and the generation of hypertension, through overt clinical consequences. These observations also highlight the need for a greater emphasis on multiple risk factor intervention to target the continuum of hypertensive disease from its earliest gestation through overt cardiovascular disease. Data from recent clinical trials support this approach29-34.
Several prospective observational studies have shown that overall cardiovascular risk in hypertensive patients is compounded by the presence of additional risk factors. However there was no trial addressing benefits of lipid lowering in primary prevention of CHD in hypertensive patients not conventionally deemed dyslipidaemic. Furthermore there was less than expected CHD prevention using standard BP-lowering therapy although it is obvious that combination of risk factors synergistically cause CHD. This fact led to new therapeutic opportunities and so new studies have been coordinated.
The rationale for the ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) study coordination was the high prevalence of dyslipidemia in hypertensives. In the ASCOT- BPLA (BP Lowering Arm) two different BP treatment strategies were compared (β-blocker ± a diuretic with a calcium-channel blocker ± an ACE inhibitor). In the ASCOT-LLA (Lipid Lowering Arm) in a subgroup of participants with total cholesterol levels <250 mg/dL, a statin (atorvastatin 10 mg) was compared with placebo. Both arms of the trial were stopped prematurely because of unequivocal benefits in the treatment arm.
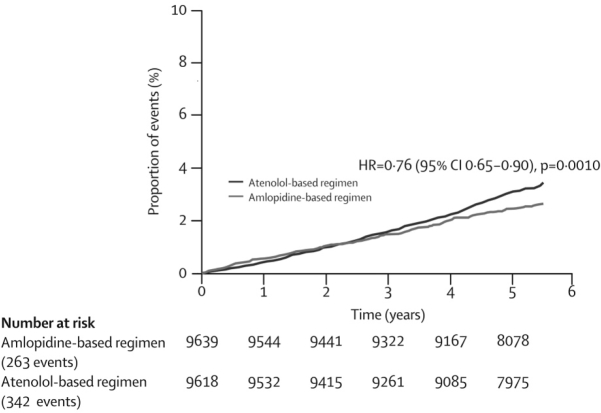
In ASCOT-BPLA, which was stopped early because of mortality differences between the two treatment arms, both total mortality and cardiovascular mortality were reduced significantly in favor of the amlodipine-based regimen (11% and 24%, respectively), (Figure 2). There was a non-significant reduction of 10% in the primary end point of nonfatal MI and fatal coronary heart disease (best explained by a lack of power owing to the premature end of the trial). A 14 % composite coronary end point and a 23 % stroke reduction were achieved in the amlodipine-based regimen, as compared with the atenolol-based one. In addition, the newer amlodipine –based strategy was associated with 30% fewer cases of new-onset diabetes. ASCOT-BPLA demonstrated greater benefits of new vs old drugs both in lowering BP and preventing CVD.
Figure 2. ASCOT-BPLA reduction in Cardiovascular Mortality.
The improved BP control with new drugs explains some, but not all, of the benefit gained. It is due to the beyond blood pressure control effect of these drugs The results of ASCOT have led to changes in European guidelines on optimal management of the hypertensive patient. Further analyses suggest the possibility of synergy between atovastatin and the amlodipine-based treatment strategy. ASCOT-LLA extended the benefit of lipid lowering to hypertensives. In ASCOT-LLA strong significant benefits of the statin on coronary heart disease and stroke were observed. Nonfatal myocardial infarction and fatal coronary disease events were reduced by 36% while stroke reduced by 27% compared to placebo35-42.
Conclusions
An optimal strategy to reduce CV risk in hypertensives may include lifestyle modification, promotion of adherence to therapy, early and aggressive target levels achievement by appropriate drug choice. However, the global risk reduction is nowadays going to become the gold standard in therapy. There is a strong evidence supportings that the concomitant use of newer BP drugs and statins must be suggested, especially in patients with complicated hypertension. Antihypertensive treatment should depend on global assessment of risk and not on individual risk factors or BP lowering per se. Whilst BP lowering is undoubtedly beneficial, the real target must be the global CV risk. We must go beyond BP and the most effective way to go "beyond BP" is to add a statin.
References
- 1.Franco OH, Peeters A, Bonneux L, de Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–286. doi: 10.1161/01.HYP.0000173433.67426.9b. [DOI] [PubMed] [Google Scholar]
- 2.Staessen JA, Li Y, Thijs L, Wang J-G. Blood pressure reduction and cardiovascular prevention; an update including the 2003-2004 secondary prevention trials. Hypertens Res. 2005;28:385–407. doi: 10.1291/hypres.28.385. [DOI] [PubMed] [Google Scholar]
- 3.Stergiou GS, Thomopoulou GC, Skeva II, Mountokalakis TD. Prevalence, Awareness, Treatment and Control of Hypertension in Greece-The Didima Study. AJH. 1999;12:959–965. doi: 10.1016/s0895-7061(99)00136-3. [DOI] [PubMed] [Google Scholar]
- 4.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on Blood Pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 5.Appel LJ, Moore J, Obarzanek E, et al. For the DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 6.AHA Scientific Statement (Boston) AHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update. Circulation. 2002;106:338–391. [Google Scholar]
- 7.Allison TG, Cordeiro RS, Miller TD. Prognostic Significance of Exercise-Induced Systemic Hypertension in Healthy Subjects. Am J Cardiol. 1999;83:371–375. doi: 10.1016/s0002-9149(98)00871-6. [DOI] [PubMed] [Google Scholar]
- 8.Myers J, Prakash M, Froelicher D, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 9.Singh JP, Larson MG, Manolio TA, et al. Blood Pressure Response During Treadmill Testing as a Risk Factor for New – Onset Hypertension: The Framingham Heart Study. Circulation. 1999;99:1831–1836. doi: 10.1161/01.cir.99.14.1831. [DOI] [PubMed] [Google Scholar]
- 10.Chapman RH, Benner JS, PEtrill AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165:1147–1152. doi: 10.1001/archinte.165.10.1147. [DOI] [PubMed] [Google Scholar]
- 11.Julius St, Kjeldsen SE, Weber M. Outcomes in hypertensive patients at high cardiovascular risk treated regimen based on valsartan or amlodipine: the VALUE randomized trial. Lancet. 2004;363:2022–2031. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- 12.Vassan RS. Impact of High-Normal Blood Pressure on the Risk of Cardiovascular Disease. N Engl J Med. 2001;345:1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 13.Julius S, Nasbitt S, Egen B, et al. TROPHY study. Feasibility of Treating Prehypertension with Angiotensin-Receptor Blocker. N Engl J of Med. 2006:354–367. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 14.WHO. The World Health Report 2003. Available at: http://who.int/whr/2003/en/index.html.
- 15.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% Br Med J. 2003;326:1419–1424. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hansson L, Zachetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351(9118):1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 17.Society of Hypertension – European Society of Cardiology Guideline Committee. 2003 European Society of Hypertension -European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–1053. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Staessen JA, Wang JG, Thijis L. Cardiovascular protection and blood pressure reduction: a metanalysis. Lancet. 2001;358:1305–1315. doi: 10.1016/S0140-6736(01)06411-X. [DOI] [PubMed] [Google Scholar]
- 19.Bosch J, Lonn E, Pogue J, Arnold JM, Dagenais GR, Yusuf S, HOPE/HOPE-TOO Study Investigators Long-term effects of ramipril on cardiovascular events and on diabetes; results of the HOPE Study Extension. Circulation. 2005;112:1339–1346. doi: 10.1161/CIRCULATIONAHA.105.548461. [DOI] [PubMed] [Google Scholar]
- 20.Furberg CD, Wright JT, Davis BR, et al. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002:288–2981. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 21.Dahlof B, Dereveux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359:995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- 22.Wier MR. RAAS versus non RAAS Regimens on Cardiovascular Endpoints. J Clin Hypertens. 2006;8:99–105. [Google Scholar]
- 23.Casas JP, Chua W, Loukogeorgakis S, et al. Effect of inhibitors of the rennin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta - analysis. Lancet. 2005;366:2026–2033. doi: 10.1016/S0140-6736(05)67814-2. [DOI] [PubMed] [Google Scholar]
- 24.Giles TD, Berk BC, Black HR, et al. Expanding the definition and classification of hypertension. J Clin Hypertens. 2005;7:505–512. doi: 10.1111/j.1524-6175.2005.04769.x. on behalf of the Hypertension Writing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lloyd-Jones DM, Leip EP, Larson MG. Prediction of Lifetime Risk for Cardiovascular Disease by Risk Factor Burden at 50 Years of Age. Circualtion. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 26.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 27.Estimating Coronary Heart Disease (CHD) Risk Using Framingham Heart Study Prediction Score Sheets. Available at http://www.nhibi.nih.gov/about/framingham/riskabs.htmAccessed August 1, 2006.
- 28.Panagiotakos DB, Pitsavos C, Chrysohoou C, et al. The impact of lifestyle habits on the prevalence of the metabolic syndrome among Greek adults from the ATTICA study. Am J Heart. 2004;147:106–112. doi: 10.1016/s0002-8703(03)00442-3. [DOI] [PubMed] [Google Scholar]
- 29.Williams B. hypertension therapy: Focus on surrogate markers such as endothelium, LVH atrial fibrillation, inflammation, albouminuria. JACC. 2005;45:813–822. [Google Scholar]
- 30.Halperin RO, et al. Dyslipidemia and the risk of incident hypertension in men. Hypertension. 2006;47:45–50. doi: 10.1161/01.HYP.0000196306.42418.0e. [DOI] [PubMed] [Google Scholar]
- 31.Cohen JC, Boerwinkle E, Mosley T, et al. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med. 2006;354:1264–1272. doi: 10.1056/NEJMoa054013. [DOI] [PubMed] [Google Scholar]
- 32.Tall AR. Protease variants, LDL, and coronary heart disease. N Engl J Med. 2006;354:1310–1312. doi: 10.1056/NEJMe068026. [DOI] [PubMed] [Google Scholar]
- 33.Tousoulis D, Bosinakou E, Kotsopoulou M, Antoniadis C, Katsi V, Stefanidis C. Effects of early administration of atorvastatin treatment on thrombotic process in normocholesterolemic patients with unstable angina. Int J Cardiol. 2006;106:333–337. doi: 10.1016/j.ijcard.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 34.Cannon CP, Steinberg BA, Murphy SA, et al. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48:438–445. doi: 10.1016/j.jacc.2006.04.070. [DOI] [PubMed] [Google Scholar]
- 35.Balgent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 36.Dahlf B, Sever PS, Poulter NR, et al. Prevention of CV events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo - Scandinavian Cardiac Outcomes Trial Blood Pressure Lowering ARM (ASCOT-BPLA): a multicenter randomized controlled trial. Lancet. 2005;366:895–906. doi: 10.1016/S0140-6736(05)67185-1. for the ASCOT Investigators. [DOI] [PubMed] [Google Scholar]
- 37.Sever PS, Poulter NP. Blood pressure reduction is not the only determinant of outcome. Circulation. 2006;113:2754–2763. doi: 10.1161/CIRCULATIONAHA.105.588020. [DOI] [PubMed] [Google Scholar]
- 38.Moser M. The ASCOT Trial. J Clin Hypertens (Greenwich) 2005;7:748–750. doi: 10.1111/j.1524-6175.2005.05298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294:2437–2445. doi: 10.1001/jama.294.19.2437. [DOI] [PubMed] [Google Scholar]
- 40.Atorvastatin Effective for Stroke Prevention: Presented at ESC. 2006. Available at: http://www.pslgroup.com/dg/25ADAE.htmAccessed August 1, 2006.
- 41.Goff DC, Bertoni AG, Kramer H, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation. 2006;113:113–647. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- 42.Poulter NR, Wedel H, Dahlof B, et al. Role of blood pressure and other variables in the differential cardiovascular event rates noted in the Anglo-Scandinavian Cardiac Outcomes Trial- Blood Pressure Lowering Arm (ASCOT-BPLA) Lancet. 2005;366:907–913. doi: 10.1016/S0140-6736(05)67186-3. [DOI] [PubMed] [Google Scholar]